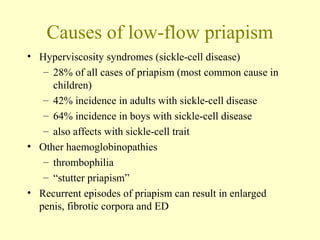
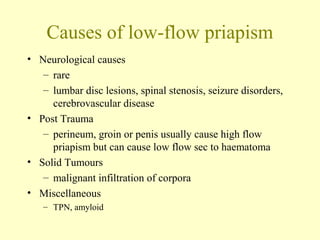
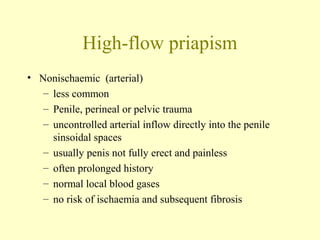
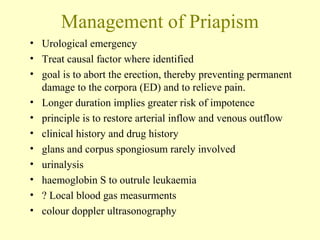
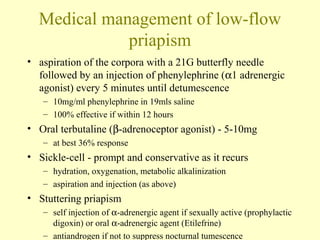
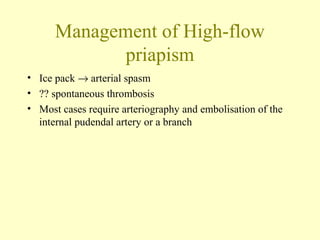
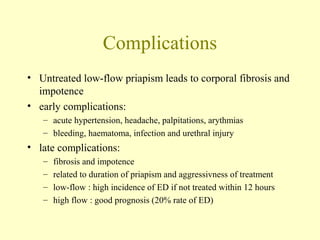
Priapism is a persistent erection not caused by sexual stimulation that lasts over 6 hours. It is classified as low-flow or high-flow. Low-flow priapism is more common and painful due to tissue ischemia. Causes include medications, sickle cell disease, and trauma. Treatment involves aspiration of blood from the corpora followed by injection of medications to restore blood flow. If unsuccessful, surgical shunting procedures may be required to prevent erectile dysfunction. High-flow priapism is less common and usually painless due to direct arterial inflow. Treatment involves embolization of arteries to resolve the erection. Untreated low-flow priapism can lead to permanent erectile dysfunction.