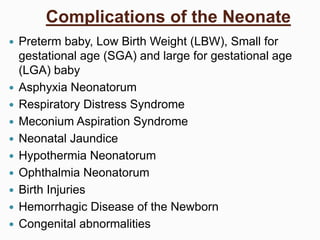
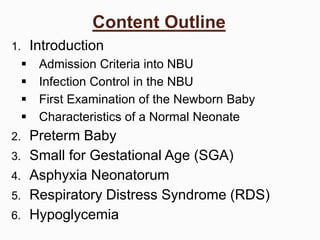
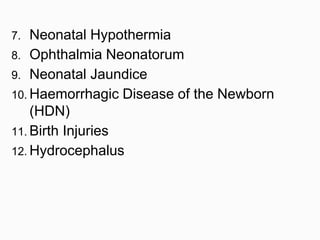
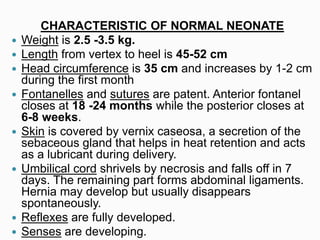
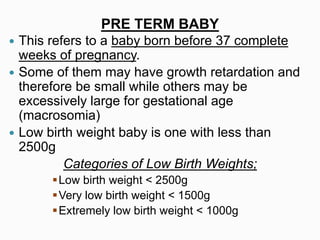
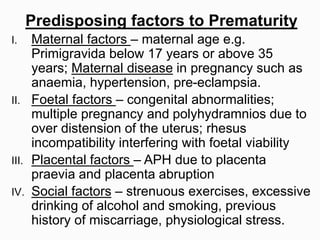
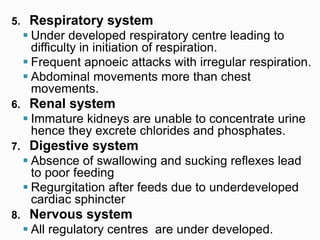
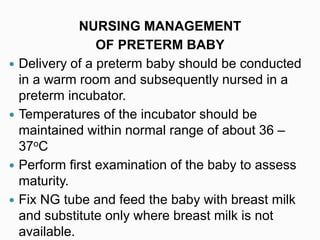
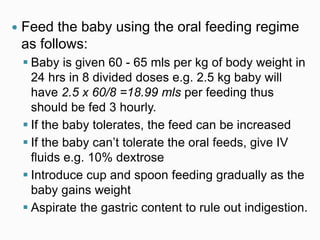
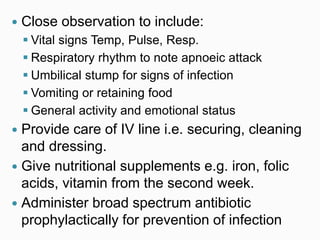
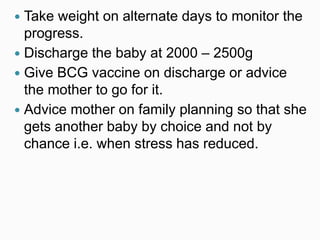
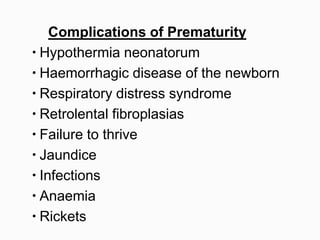
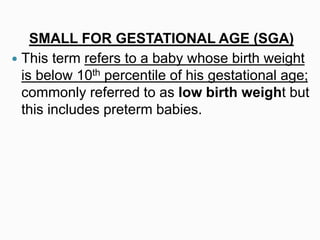
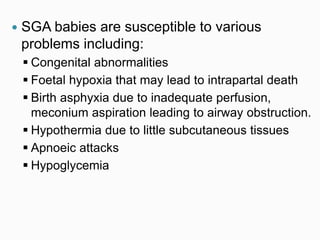
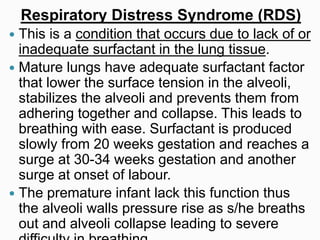
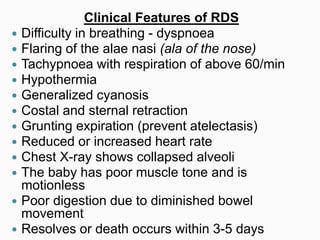
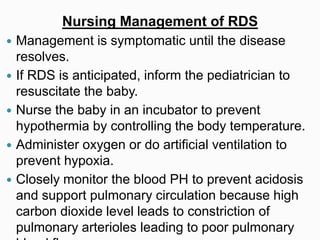
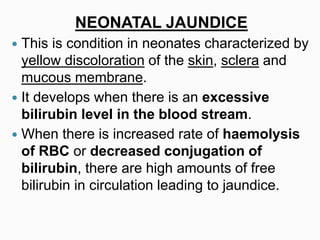
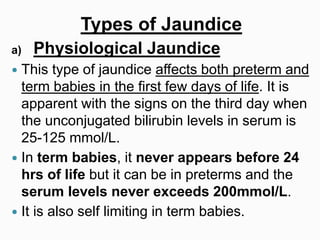
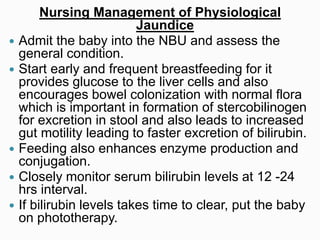
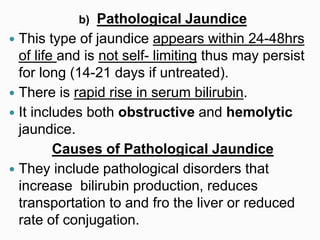
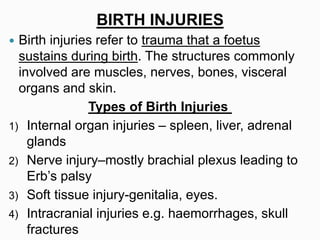
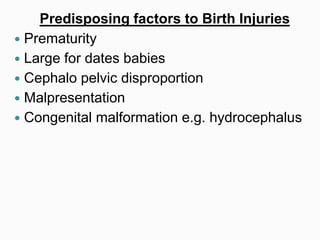
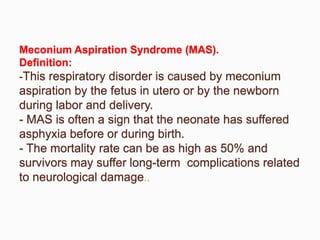
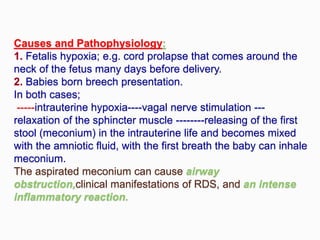
This document discusses complications that can occur in neonates (newborns). It lists potential issues like preterm birth, low birth weight, respiratory distress syndrome, jaundice, infections and birth injuries. The document then provides details on several of these complications, including the signs and symptoms of preterm babies. It describes the physiology of preterm babies and their increased risks due to underdeveloped organ systems. Overall, the document outlines various medical issues that can affect neonates and provides information on managing preterm infants.