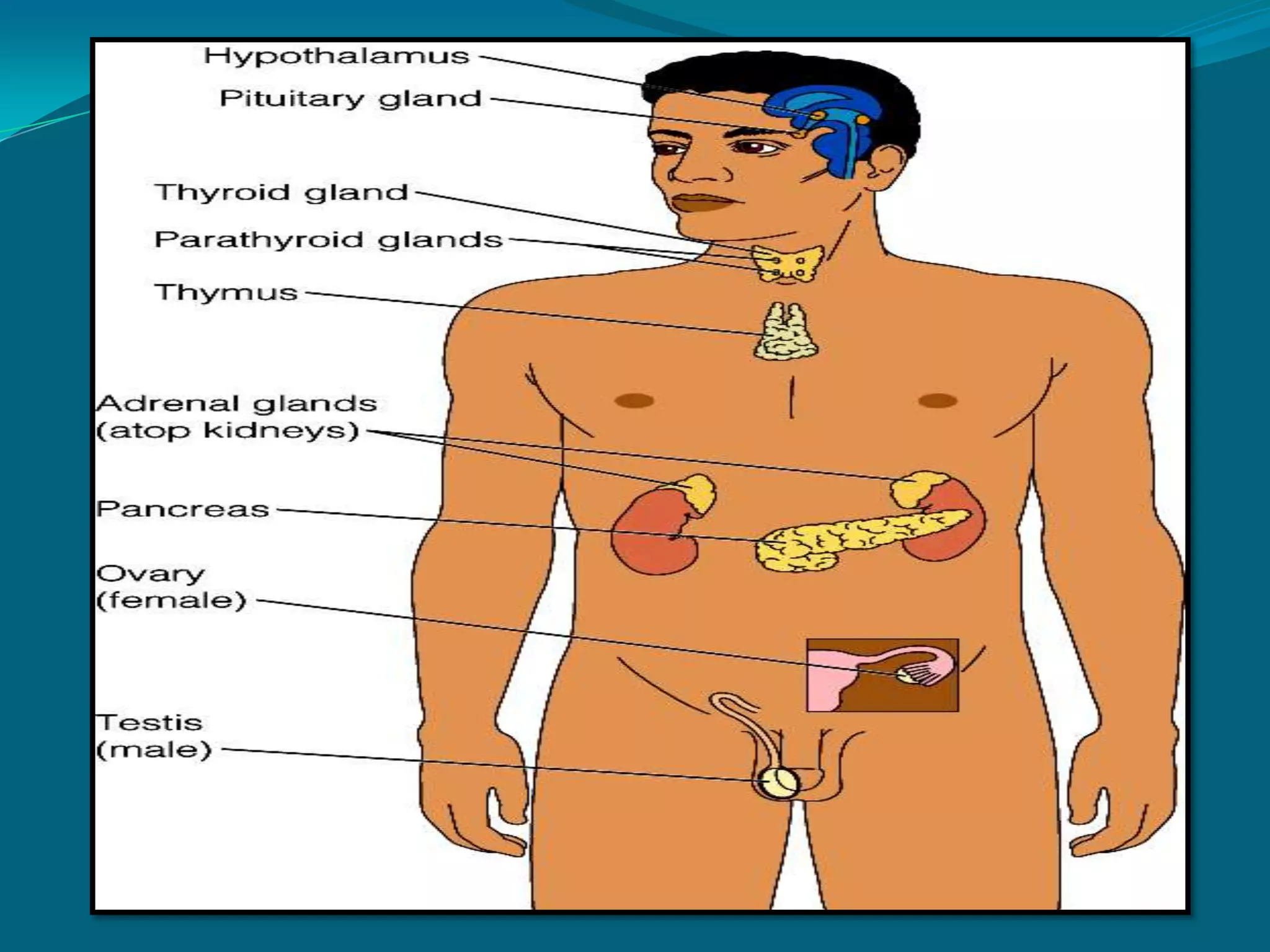
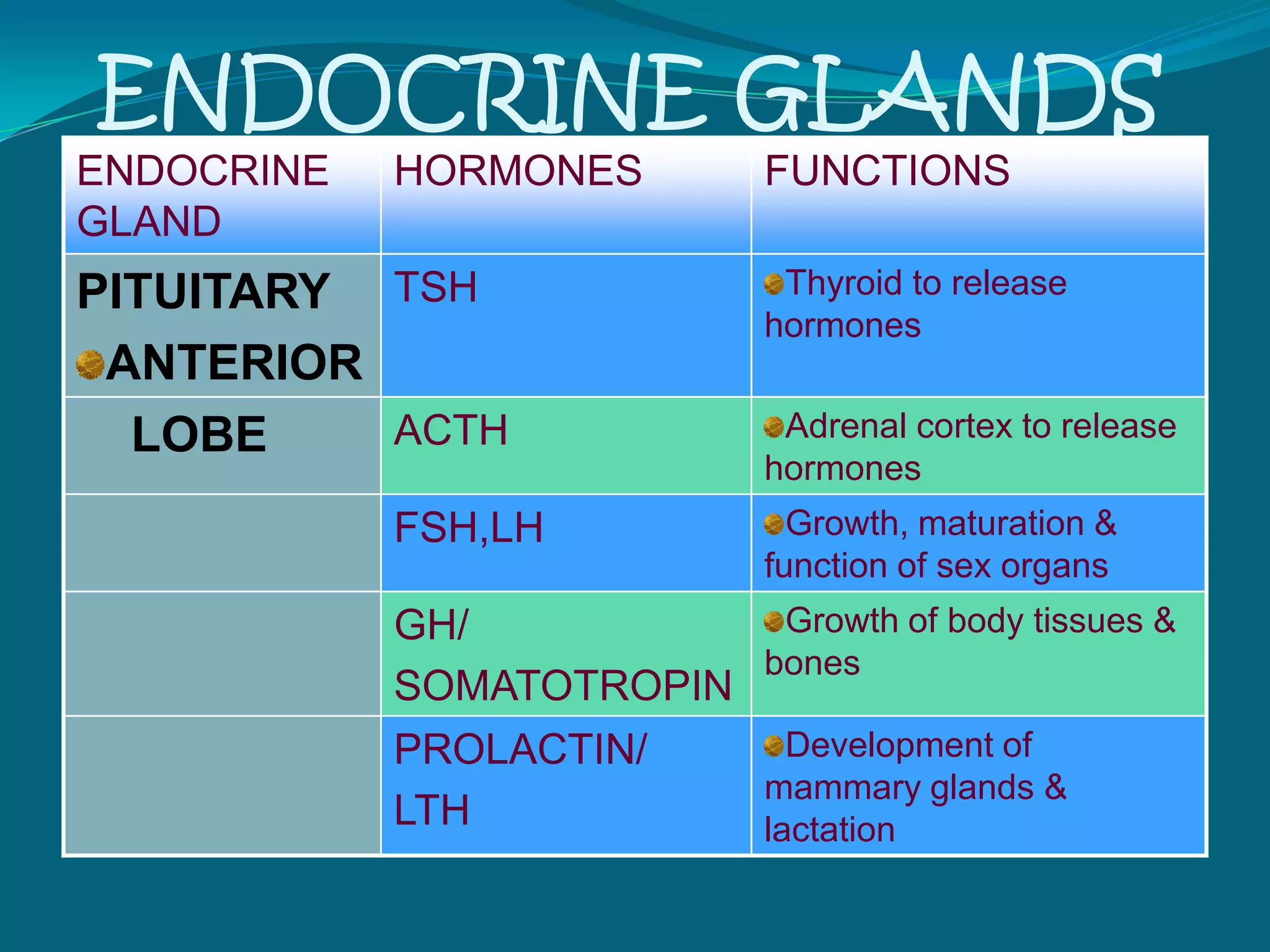
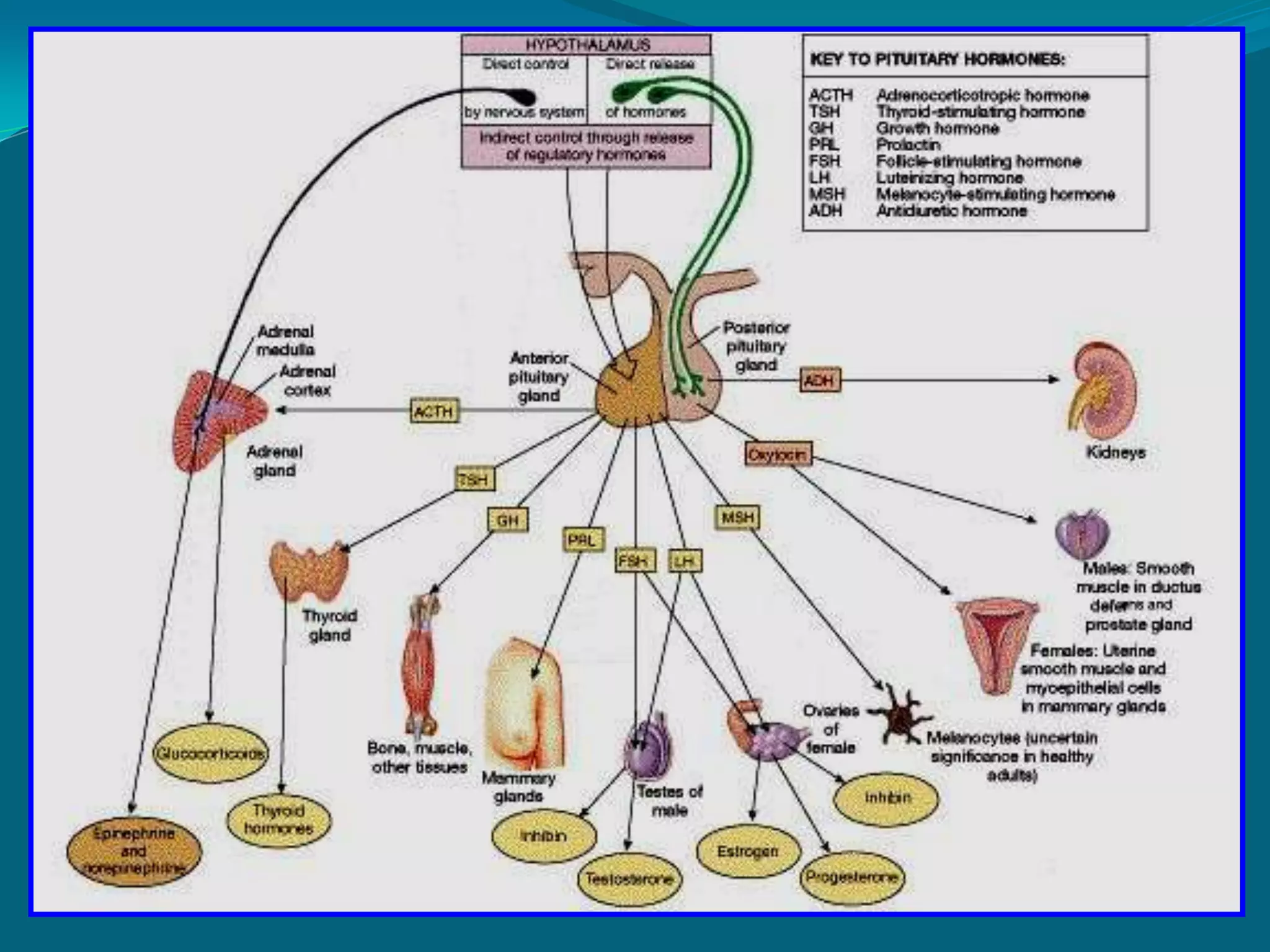
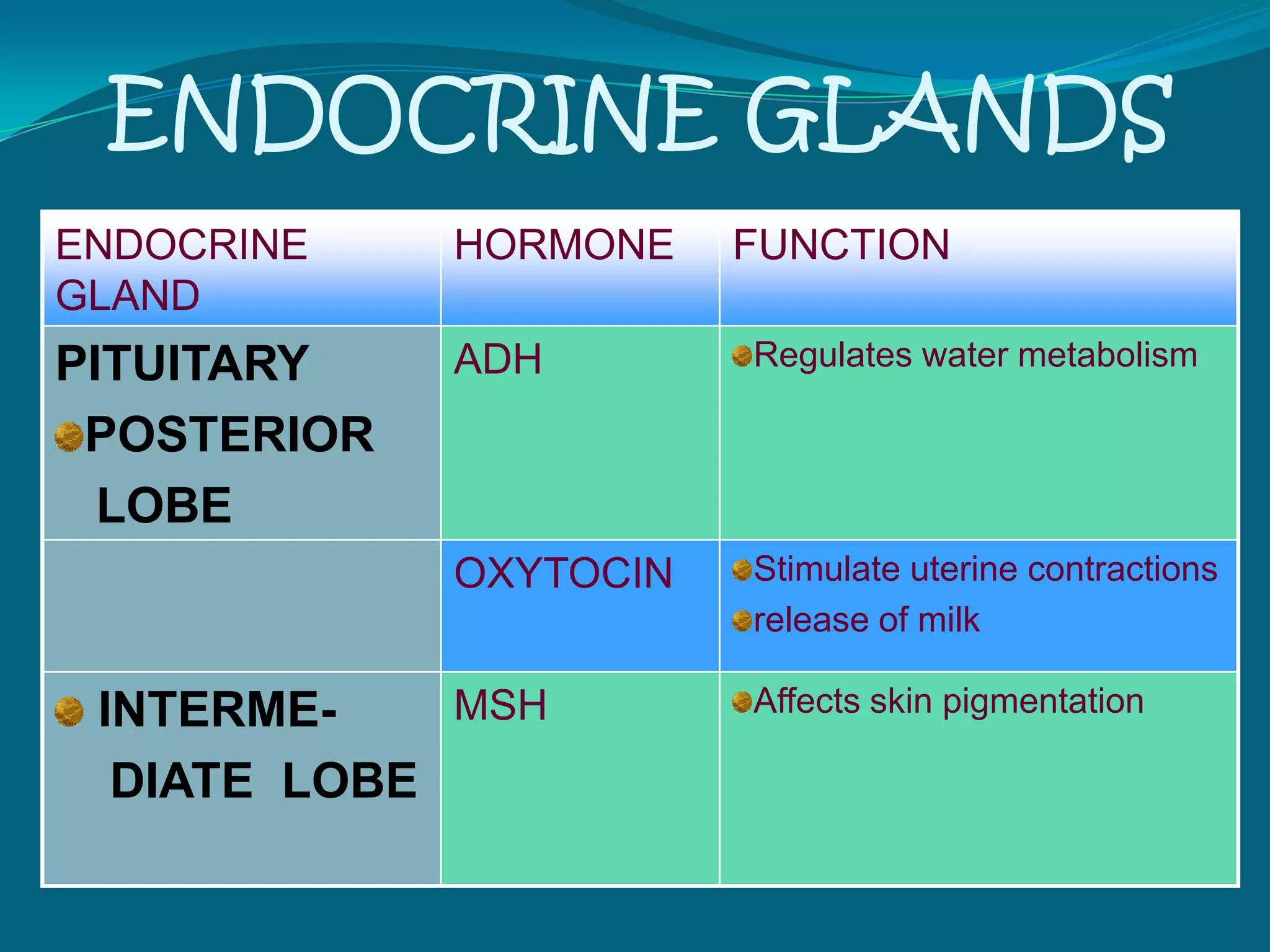
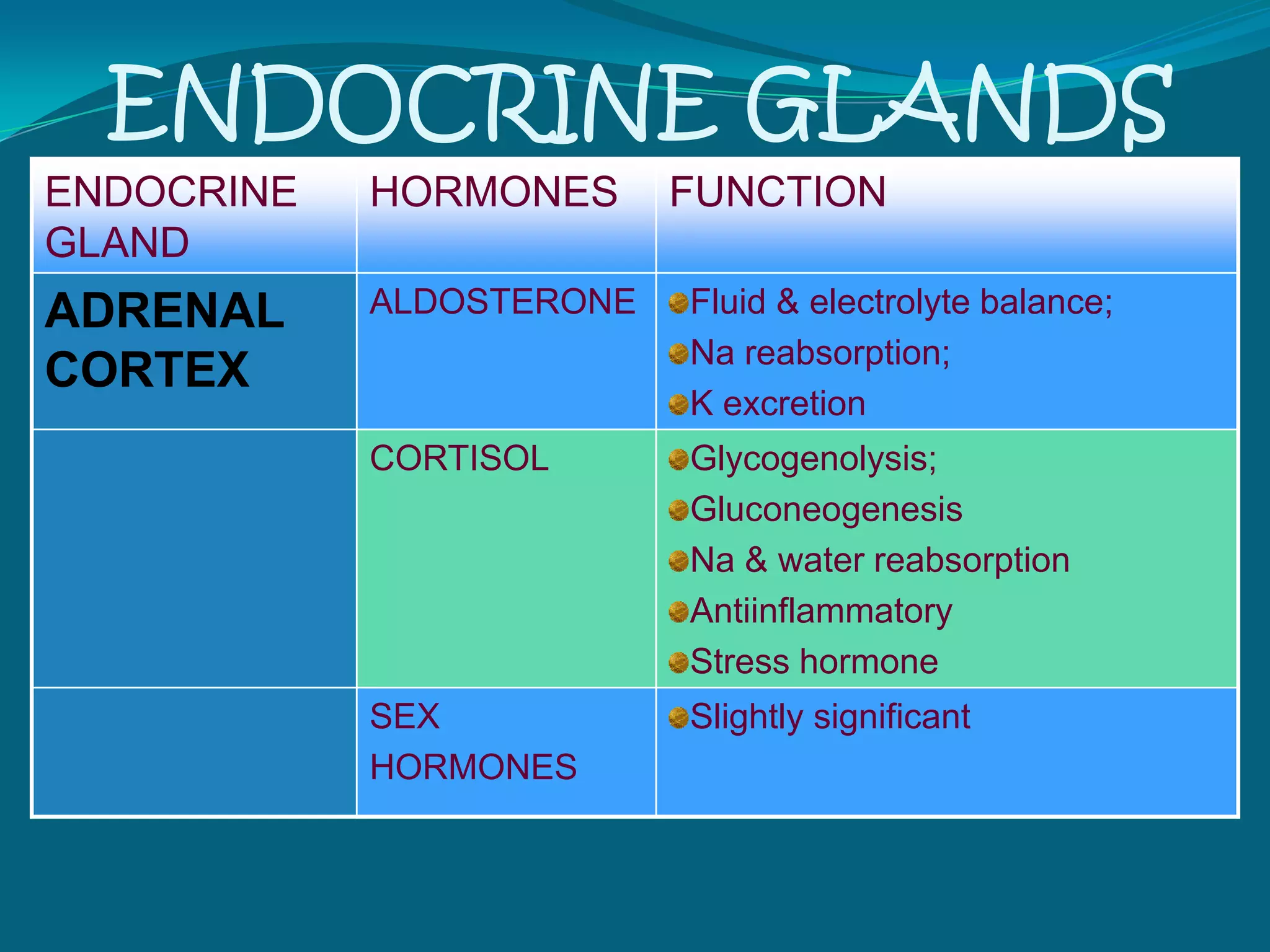
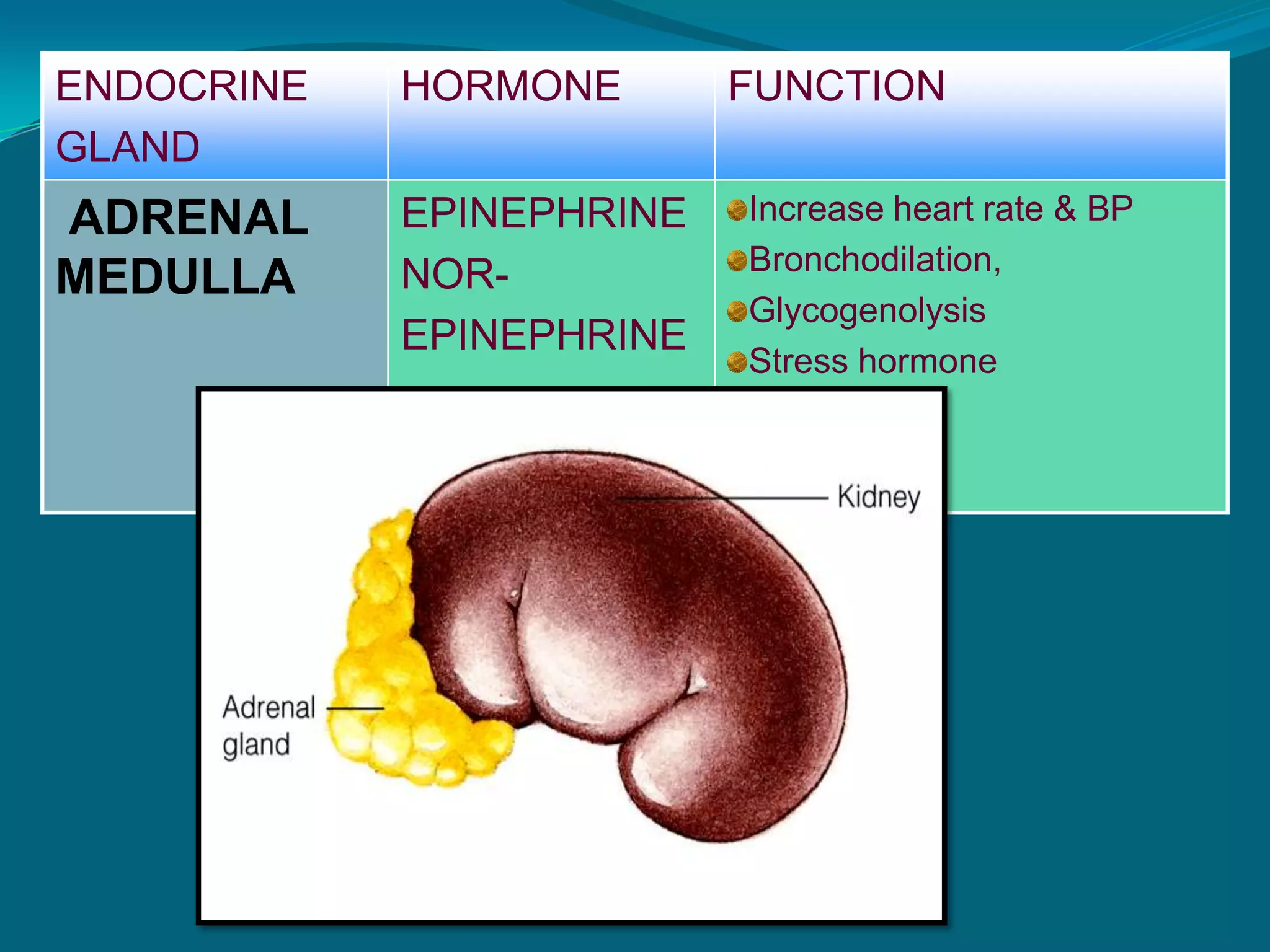
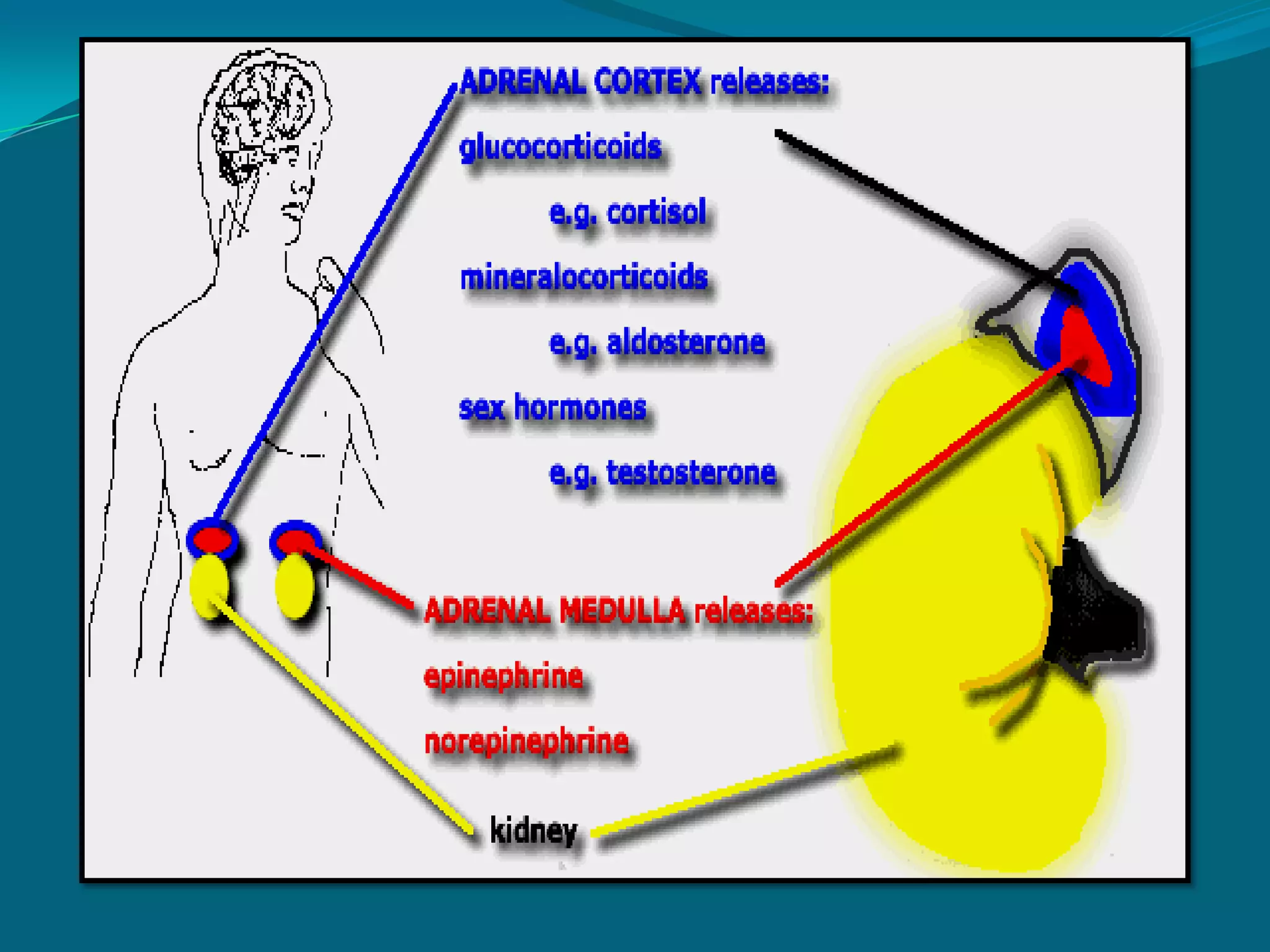
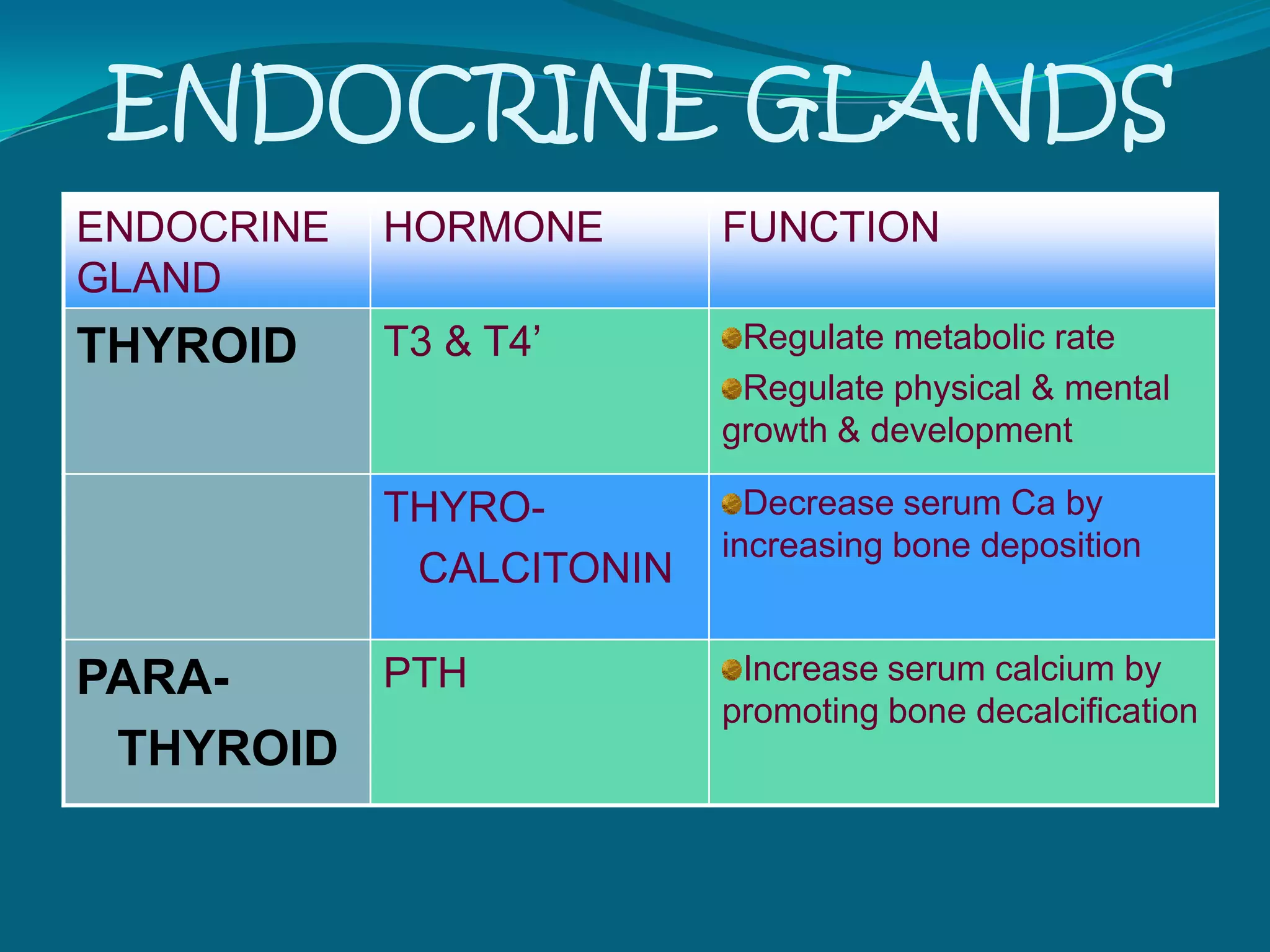
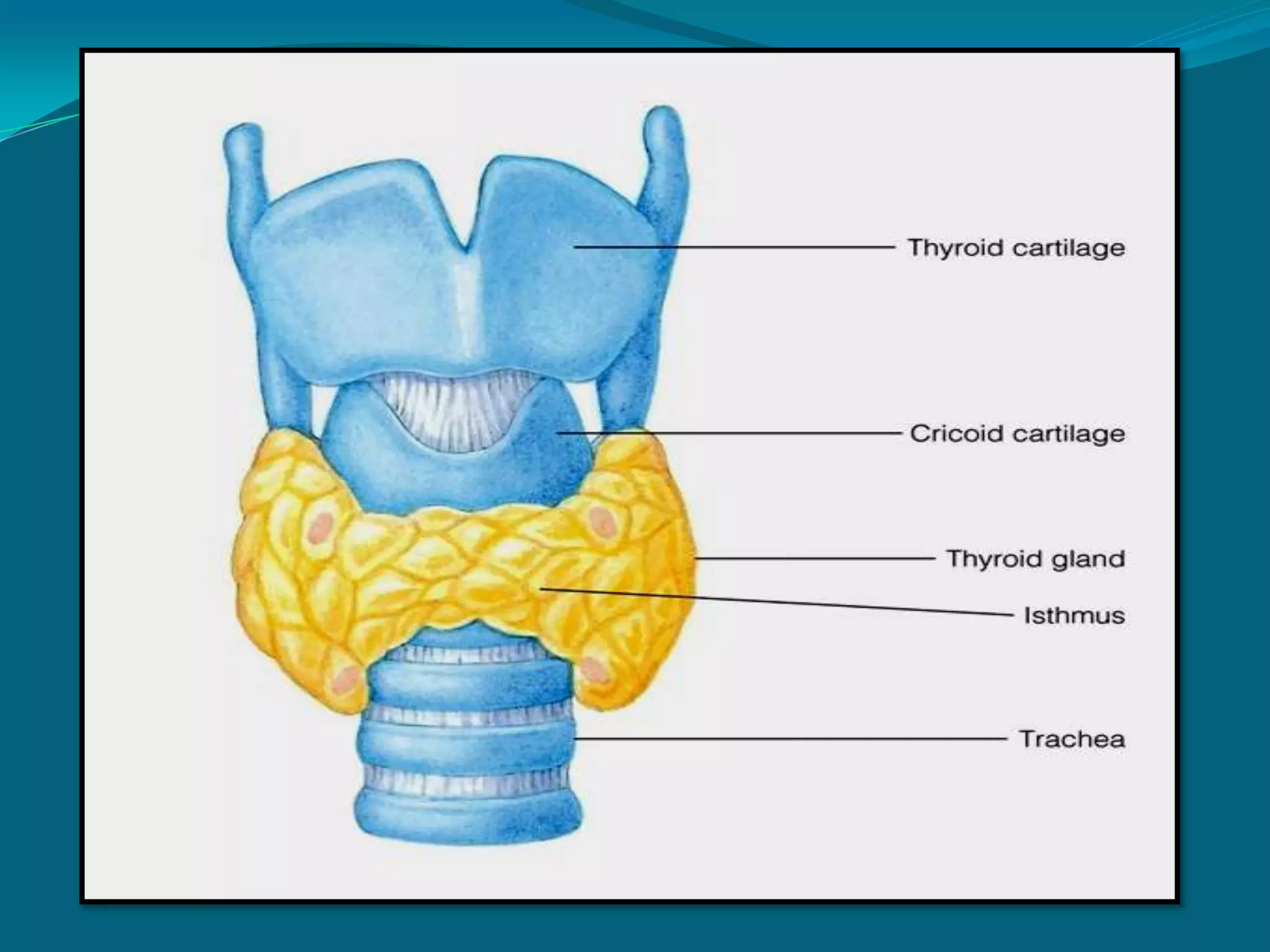
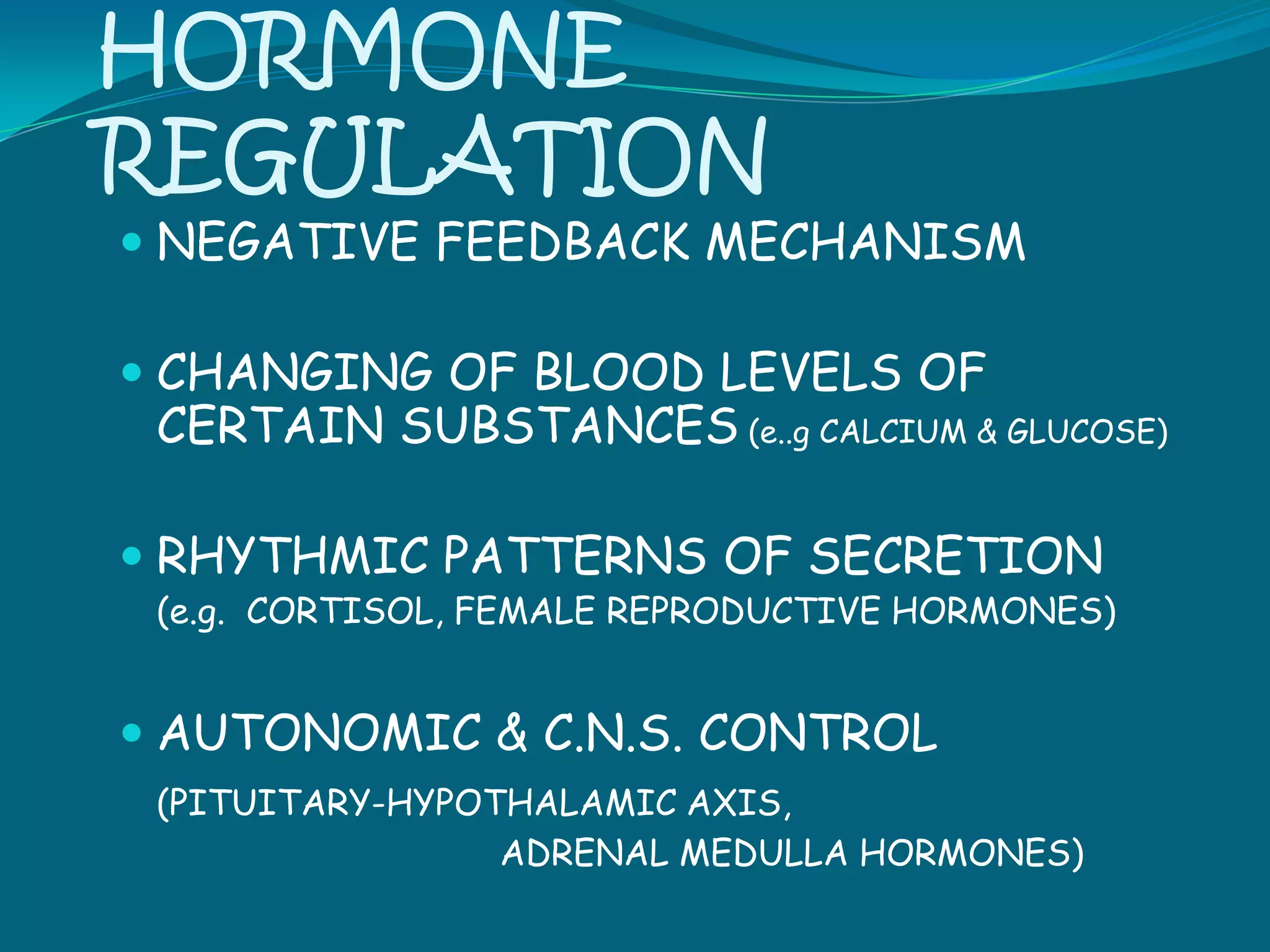
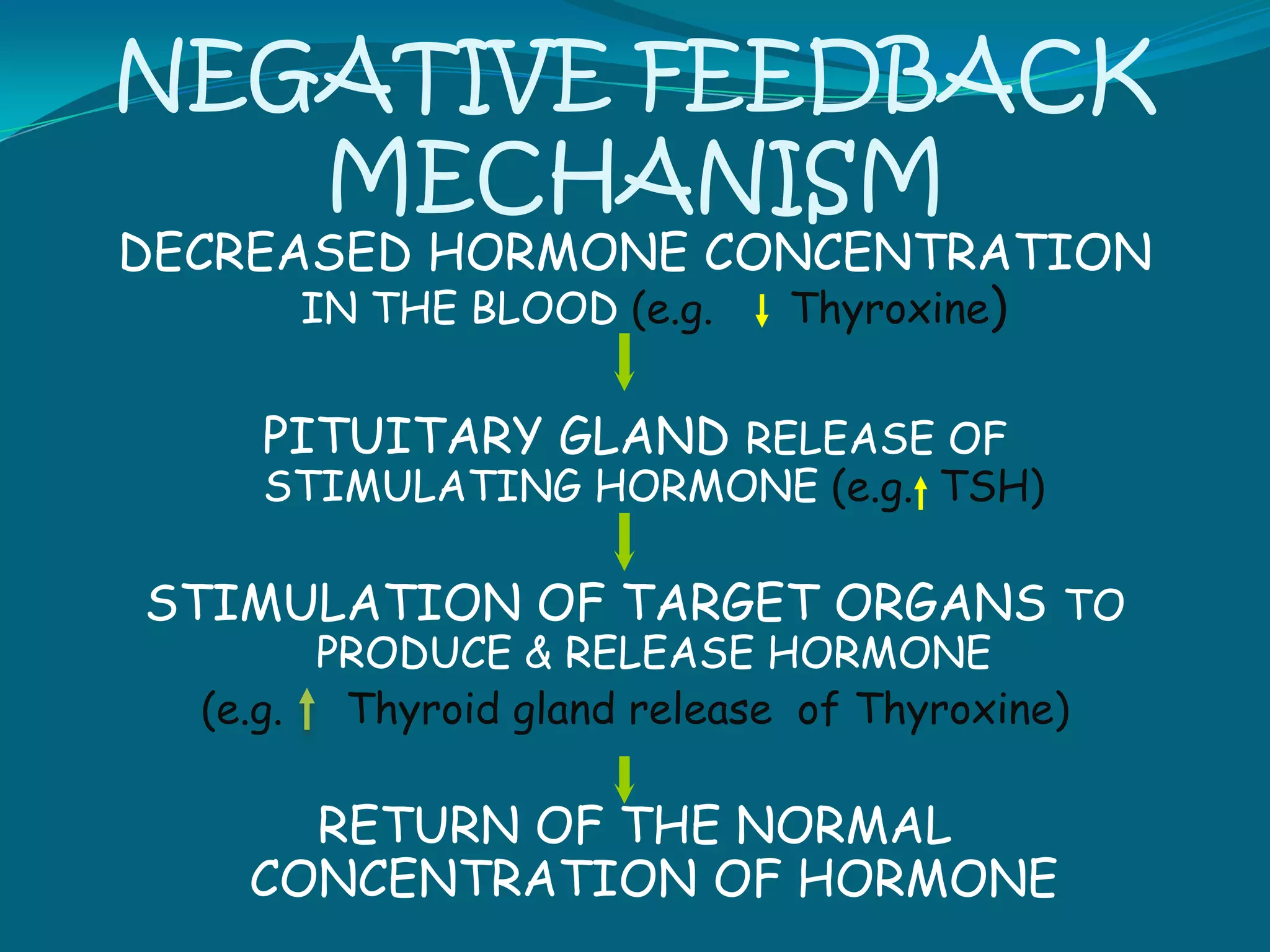
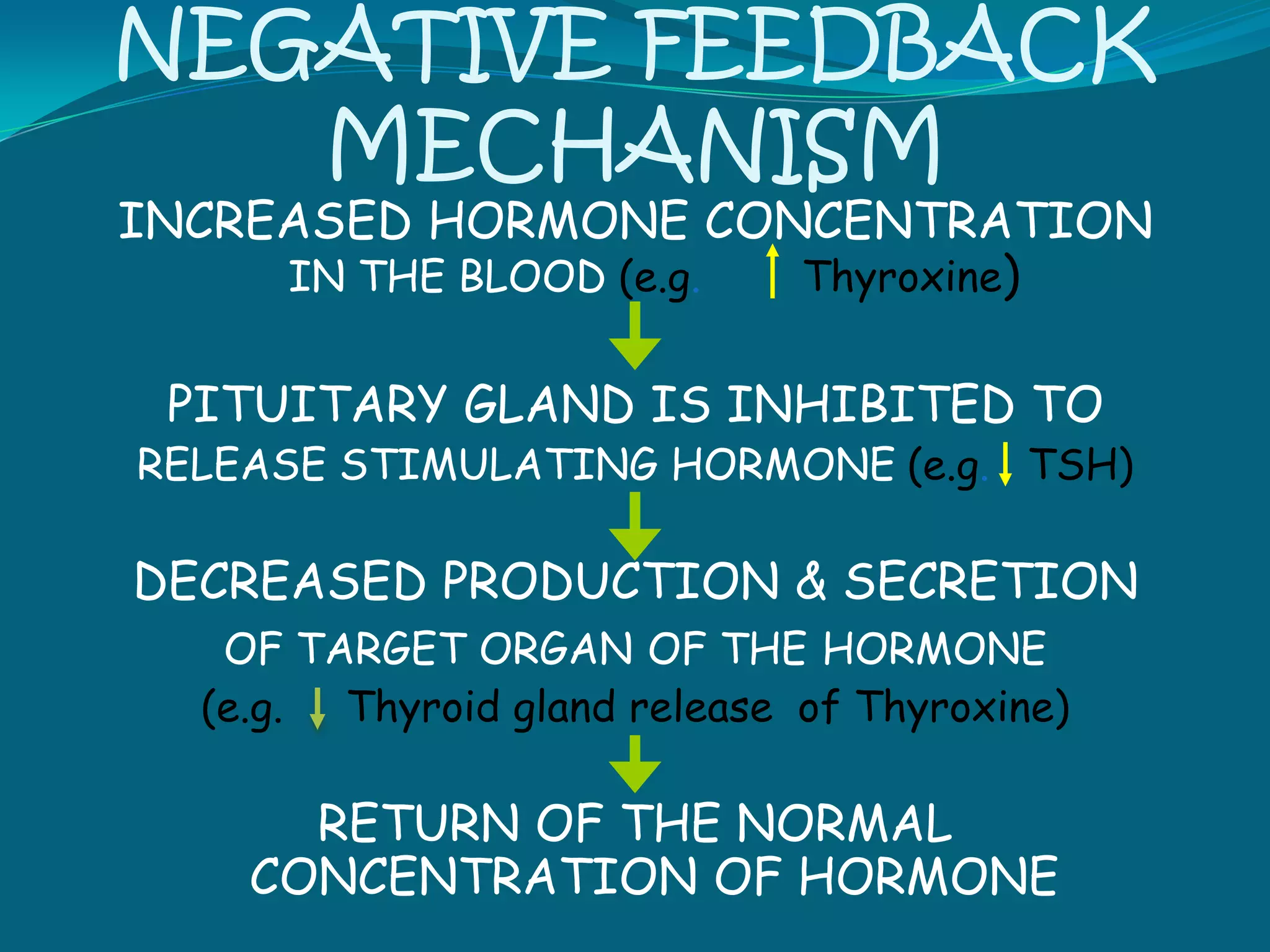
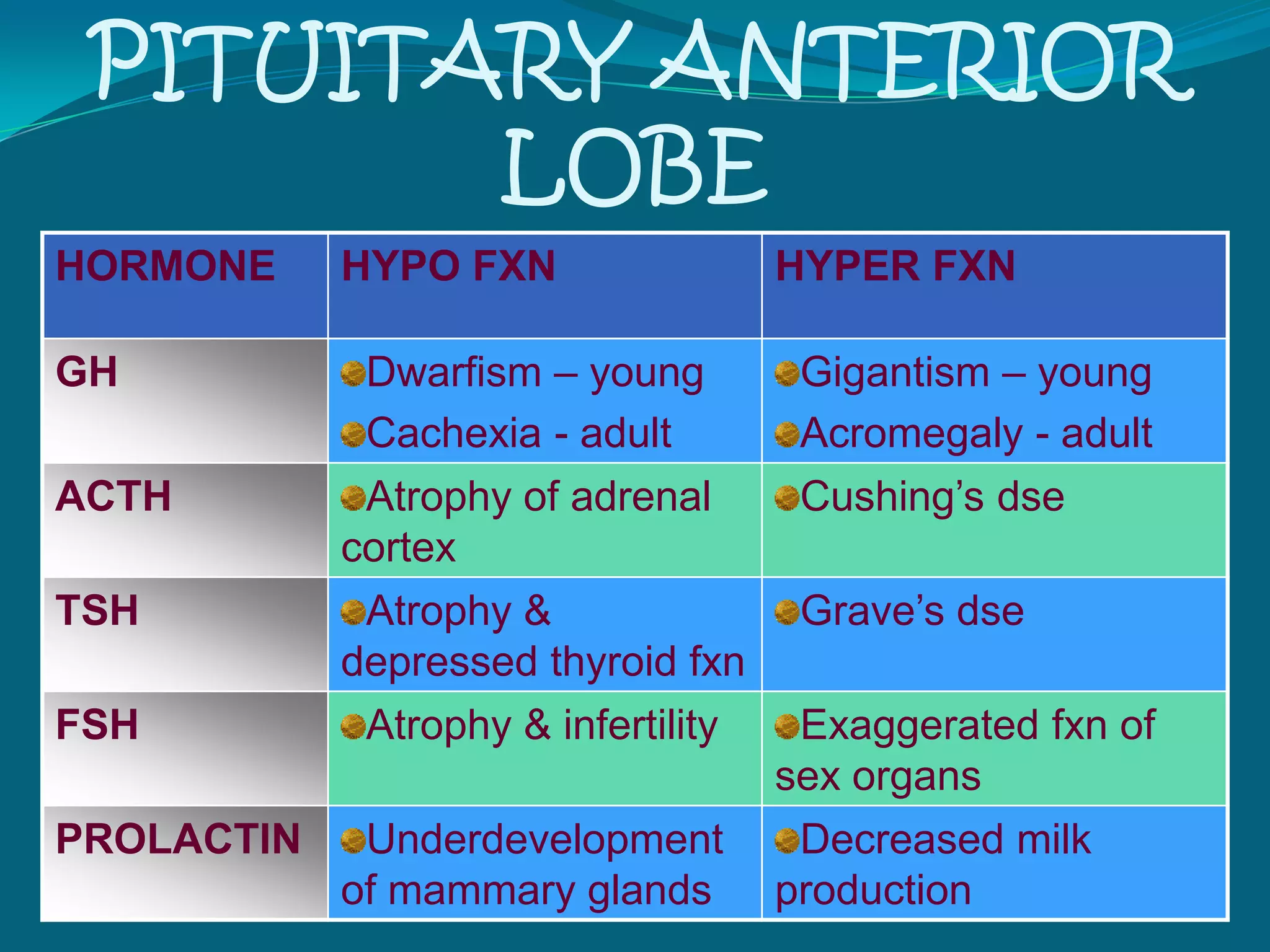
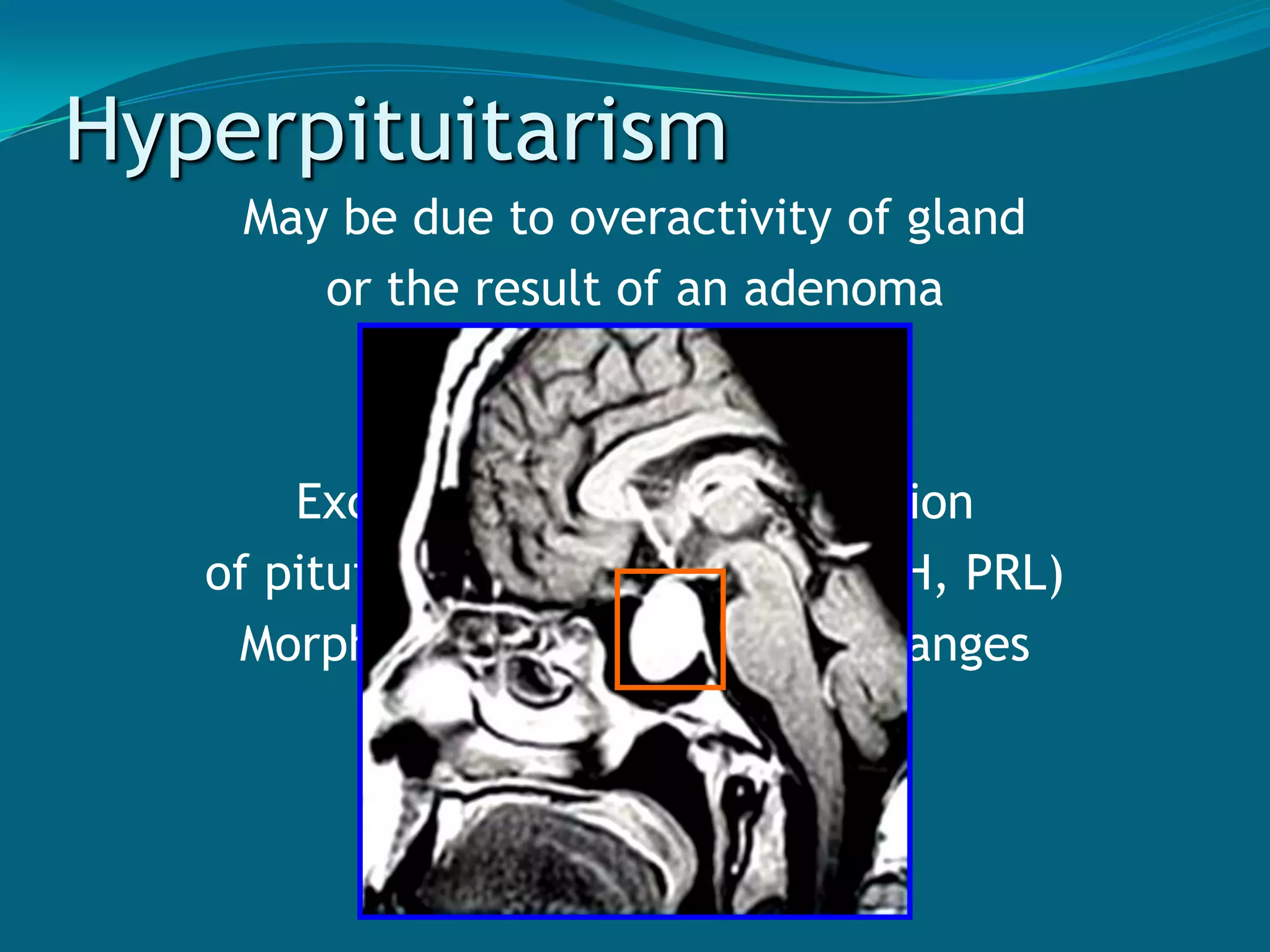
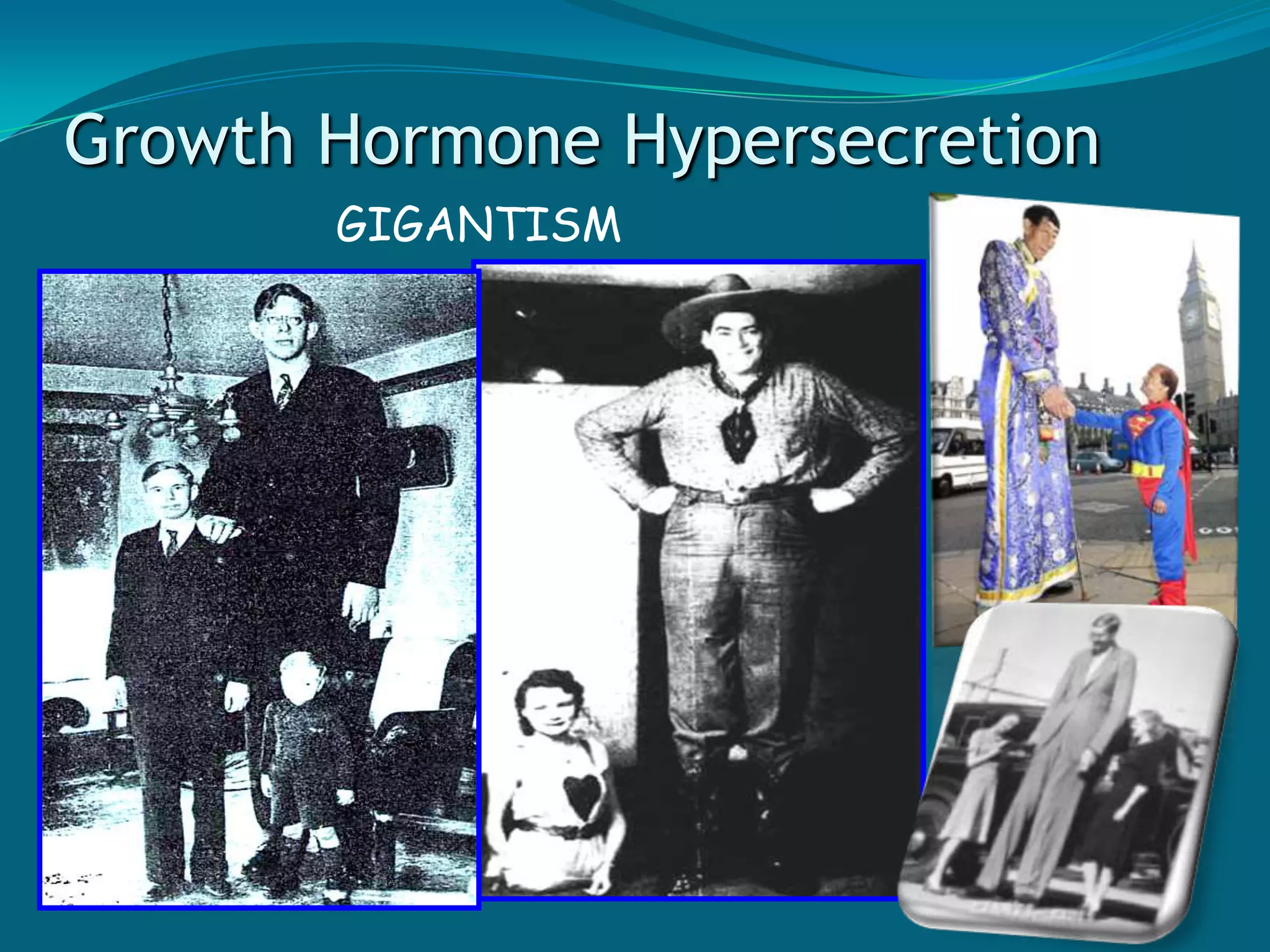
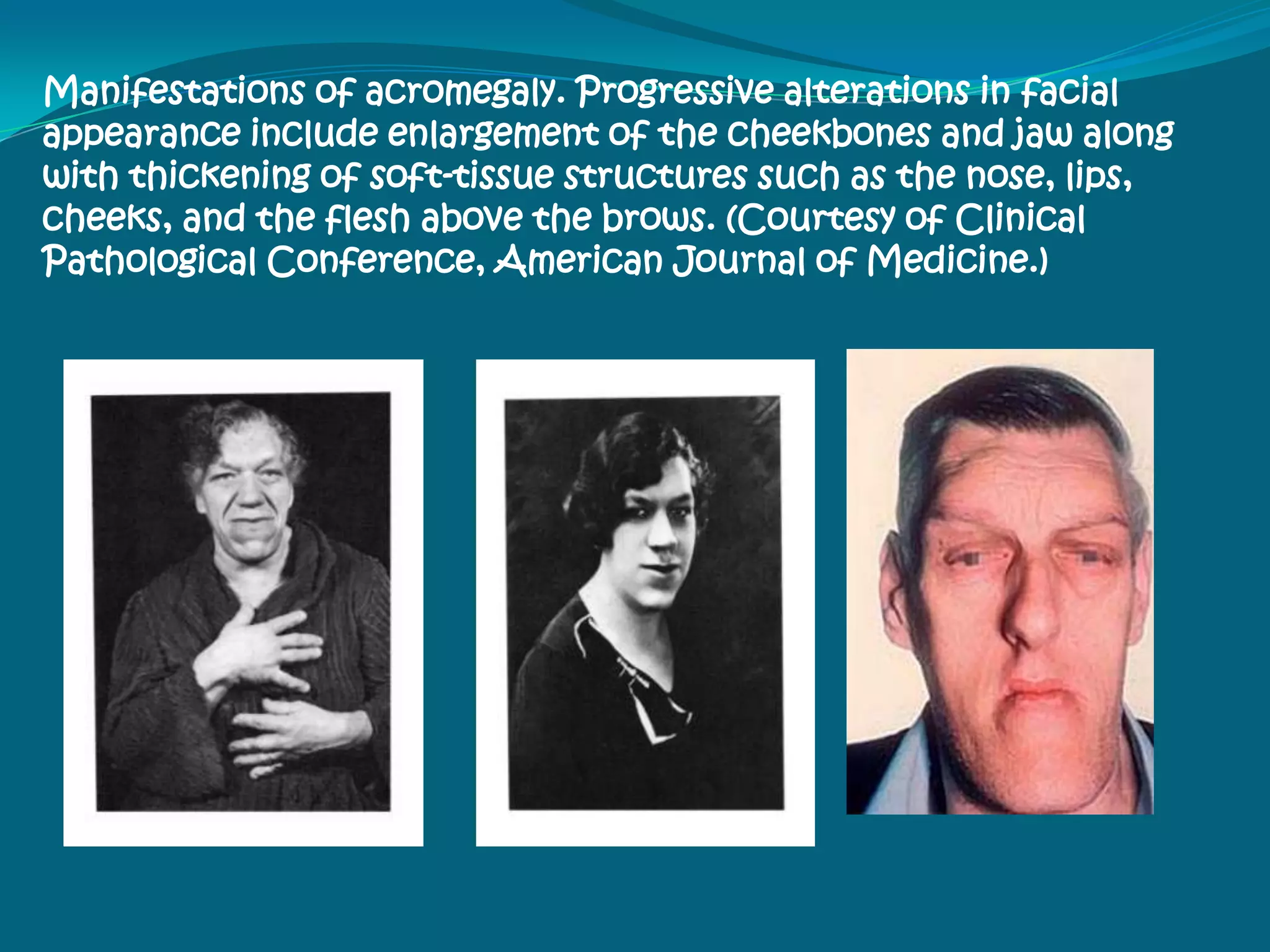
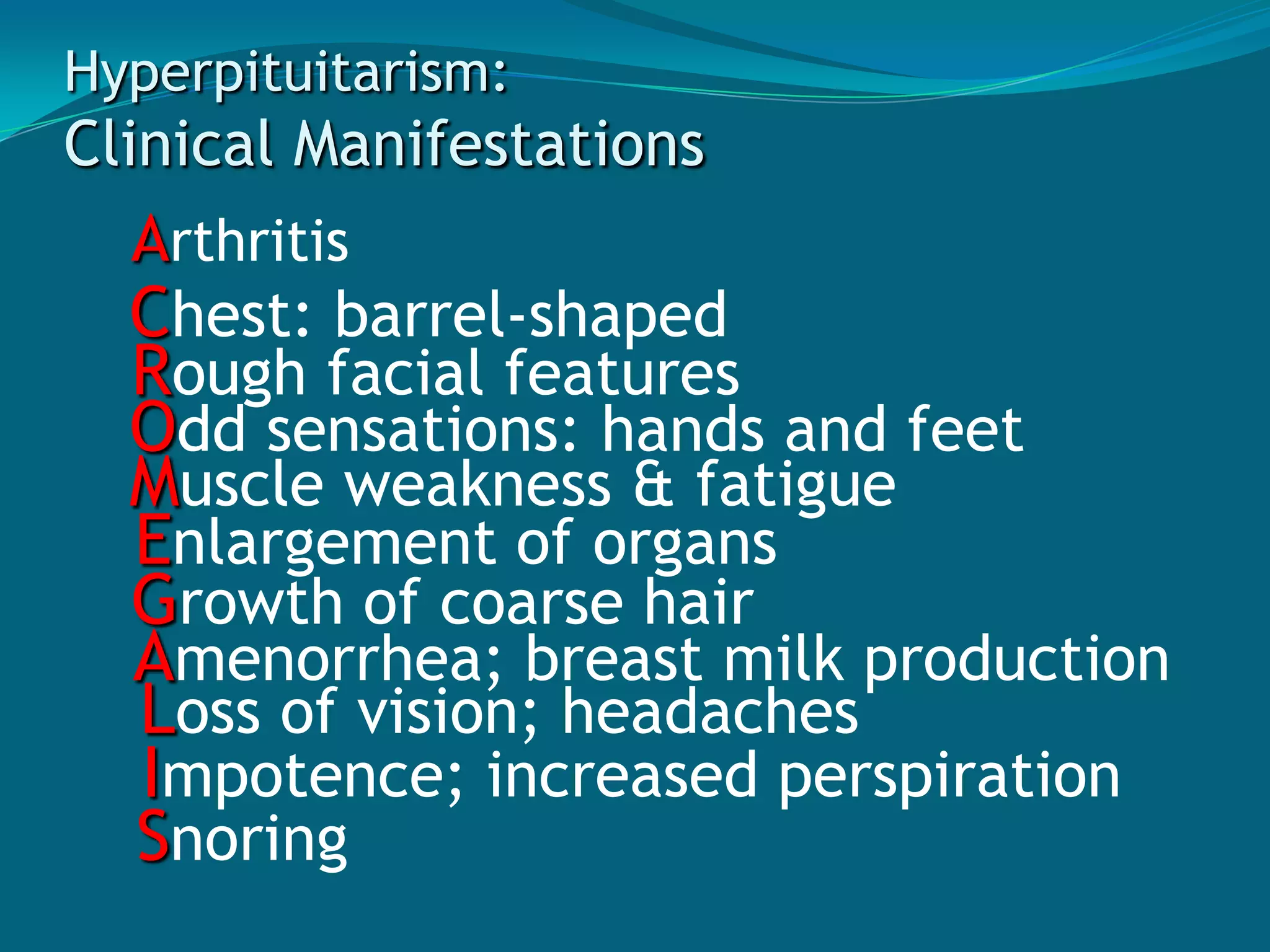
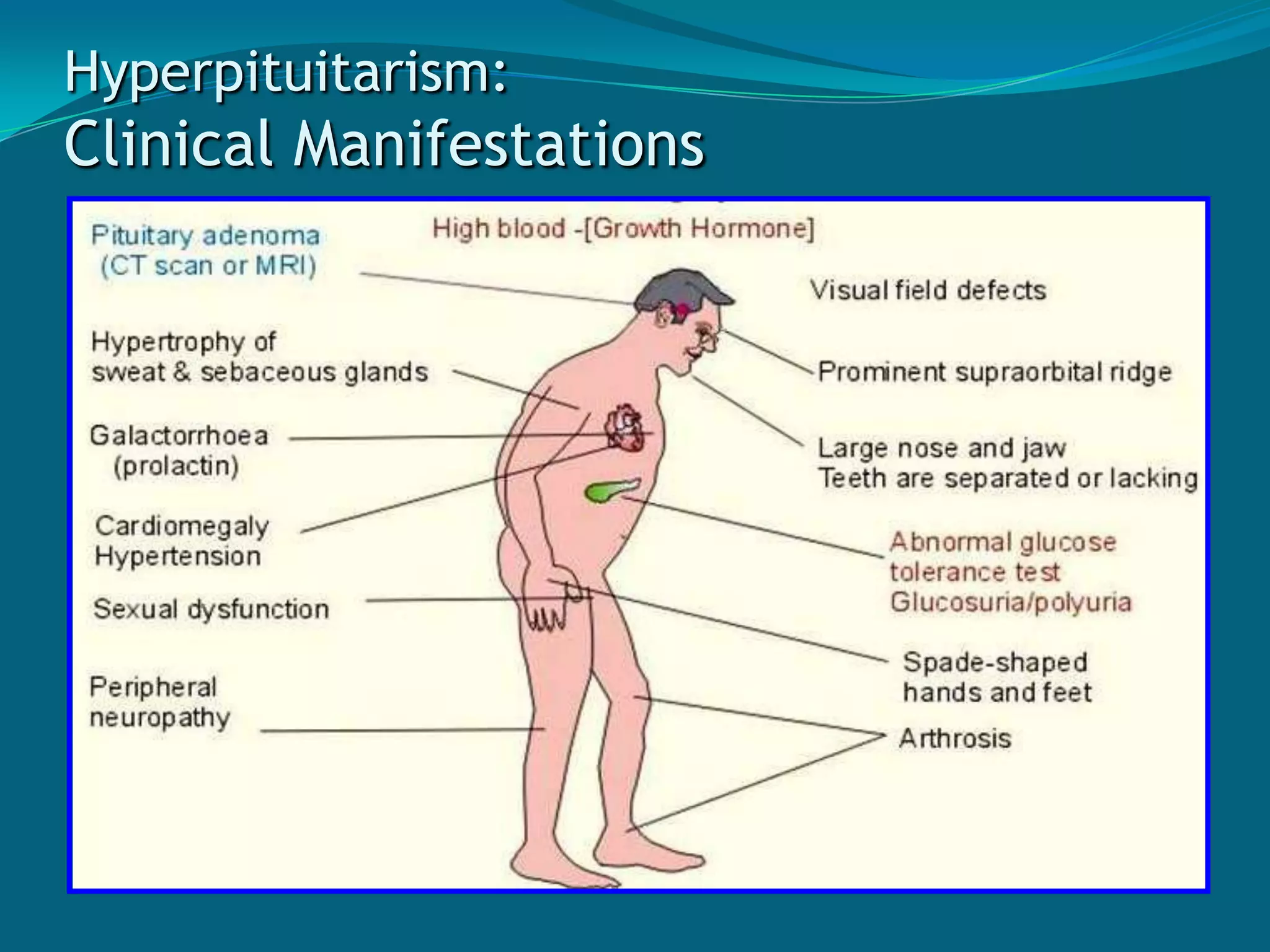
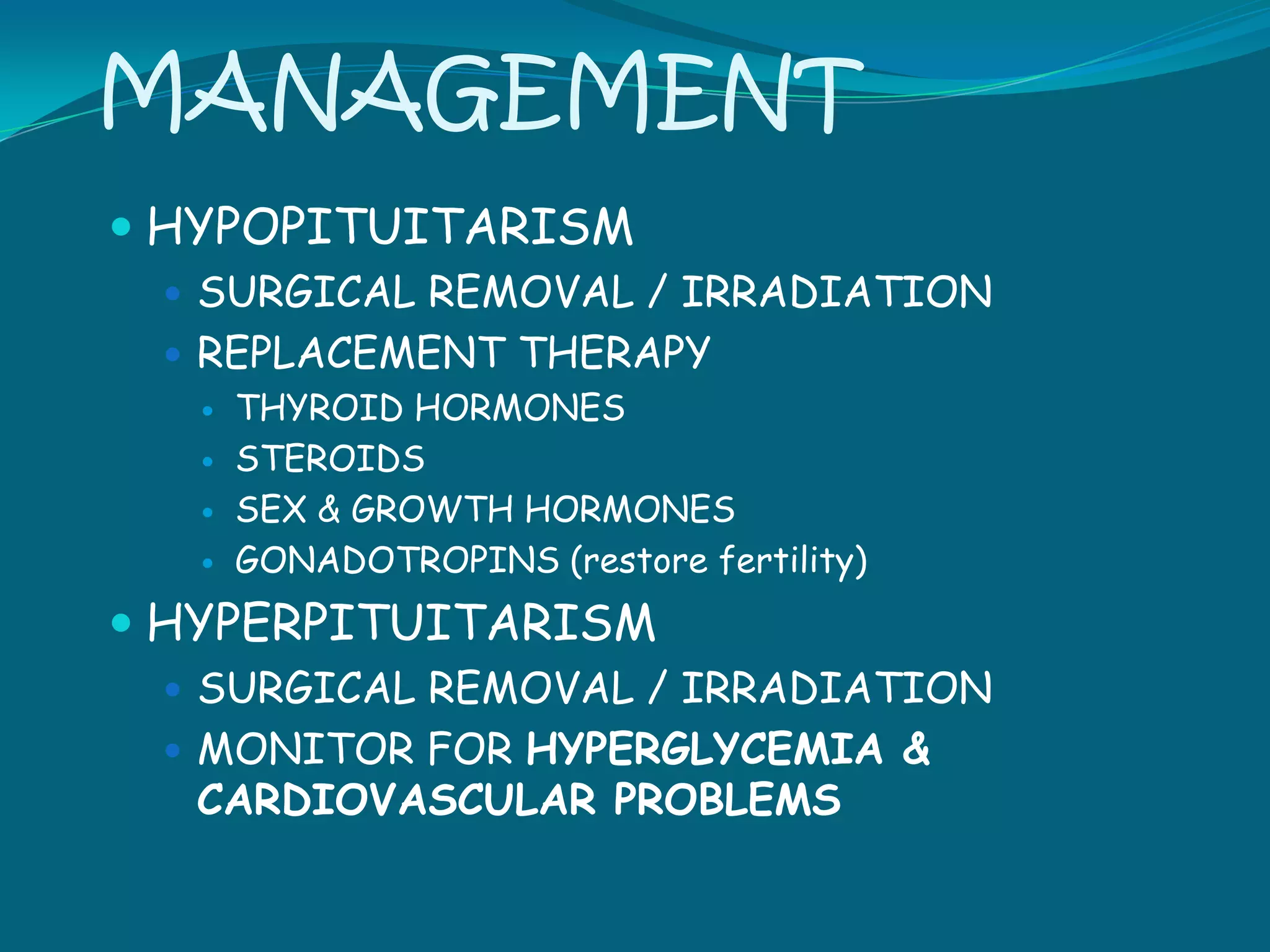
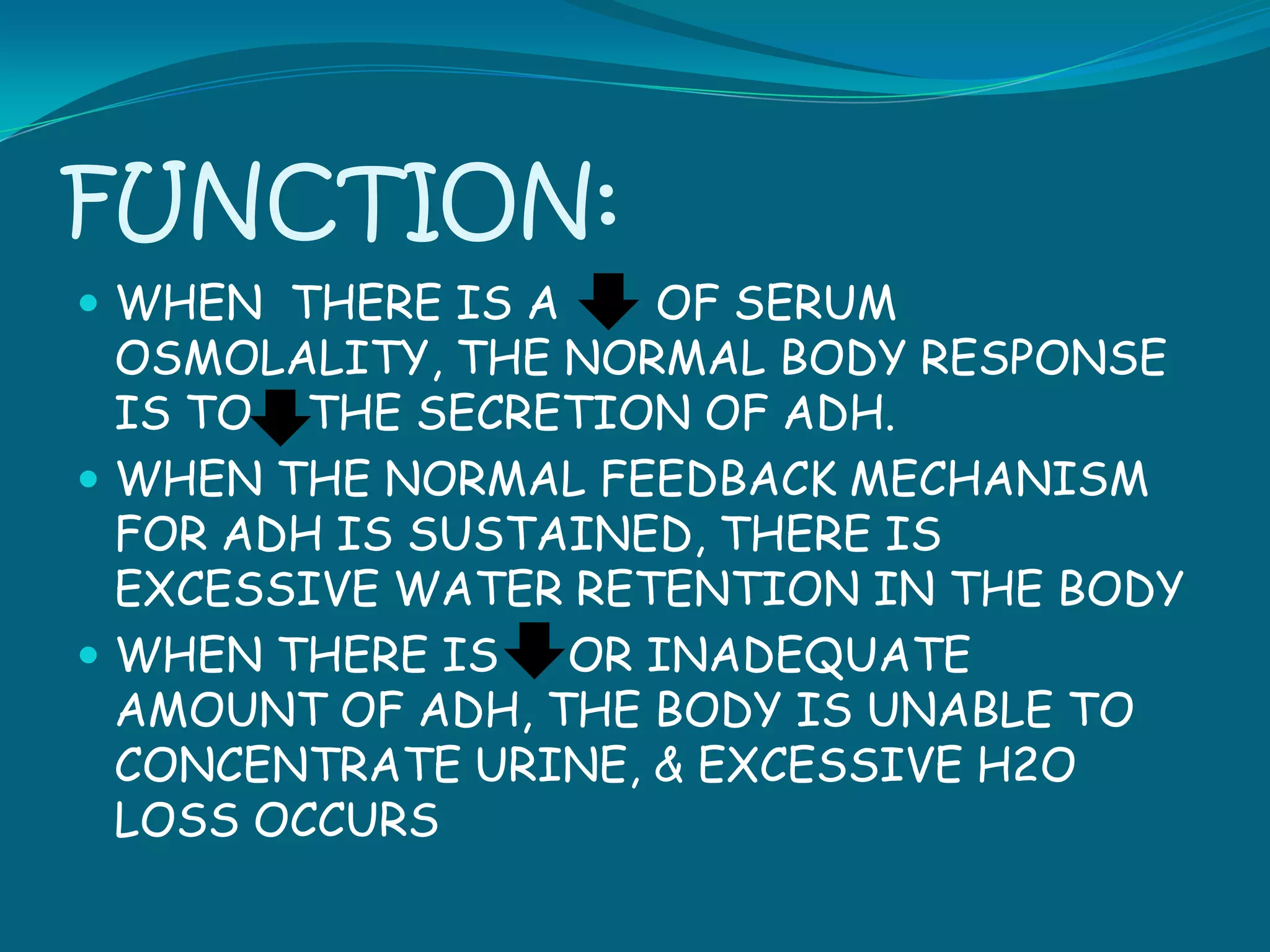
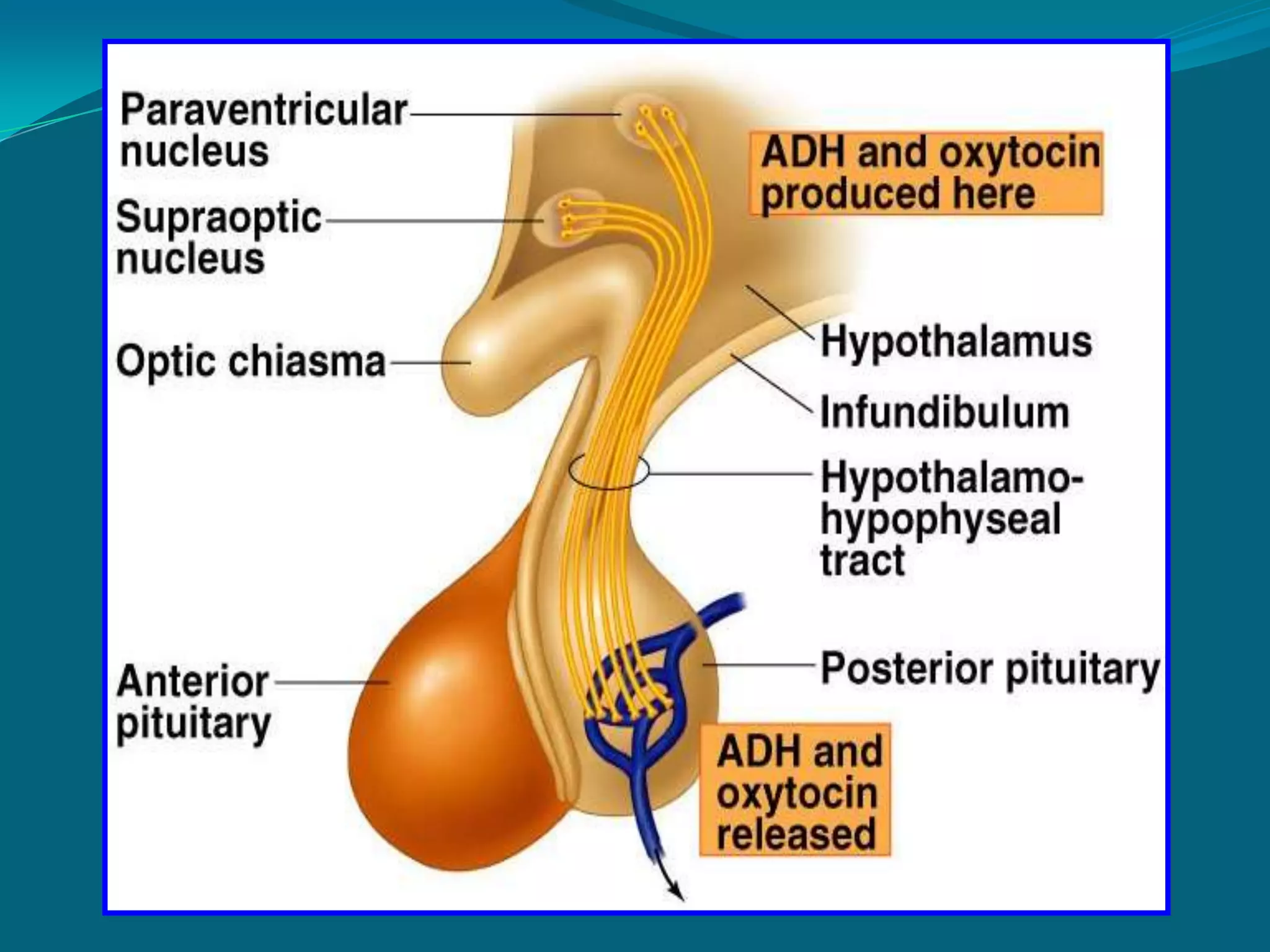
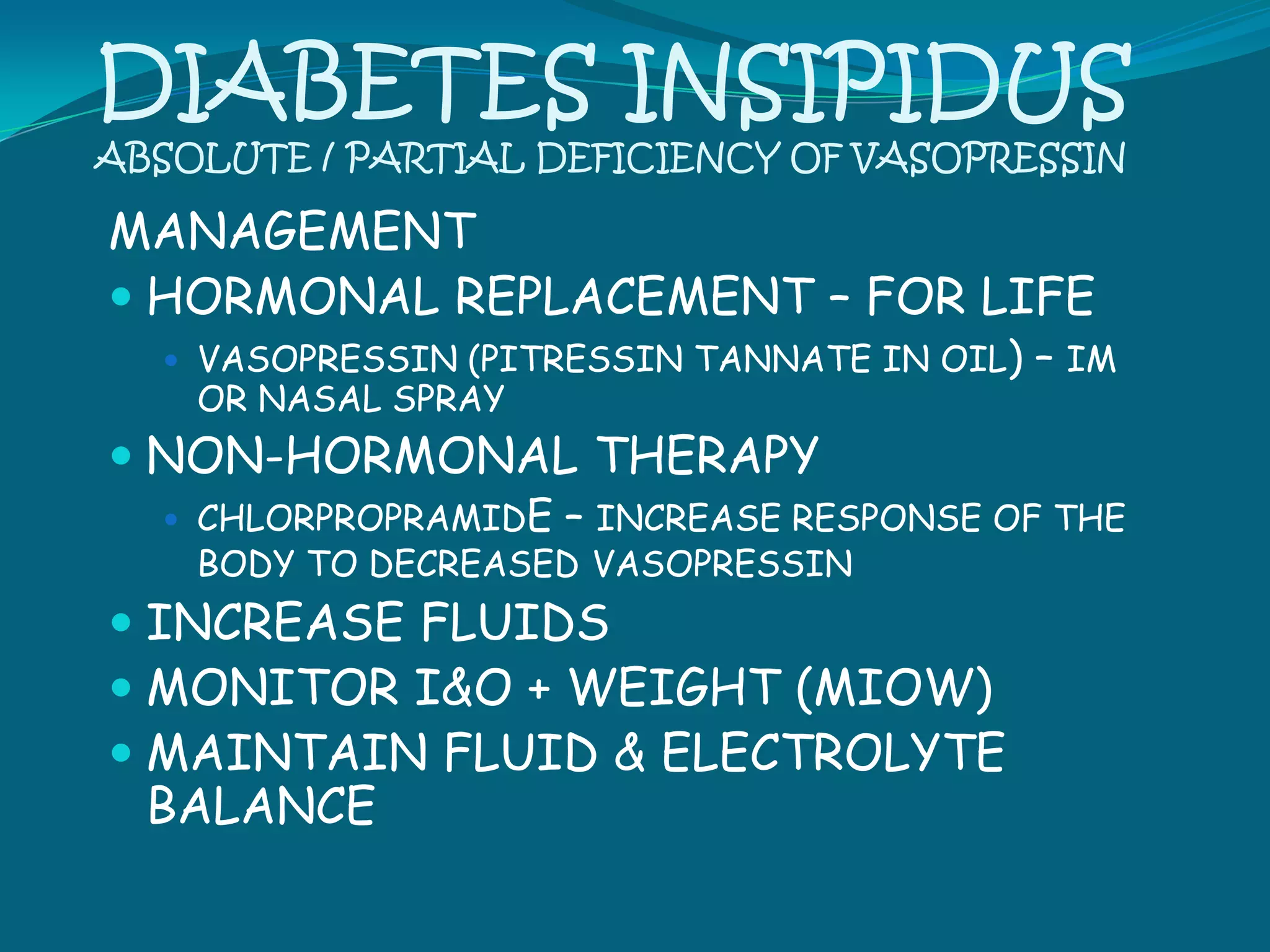
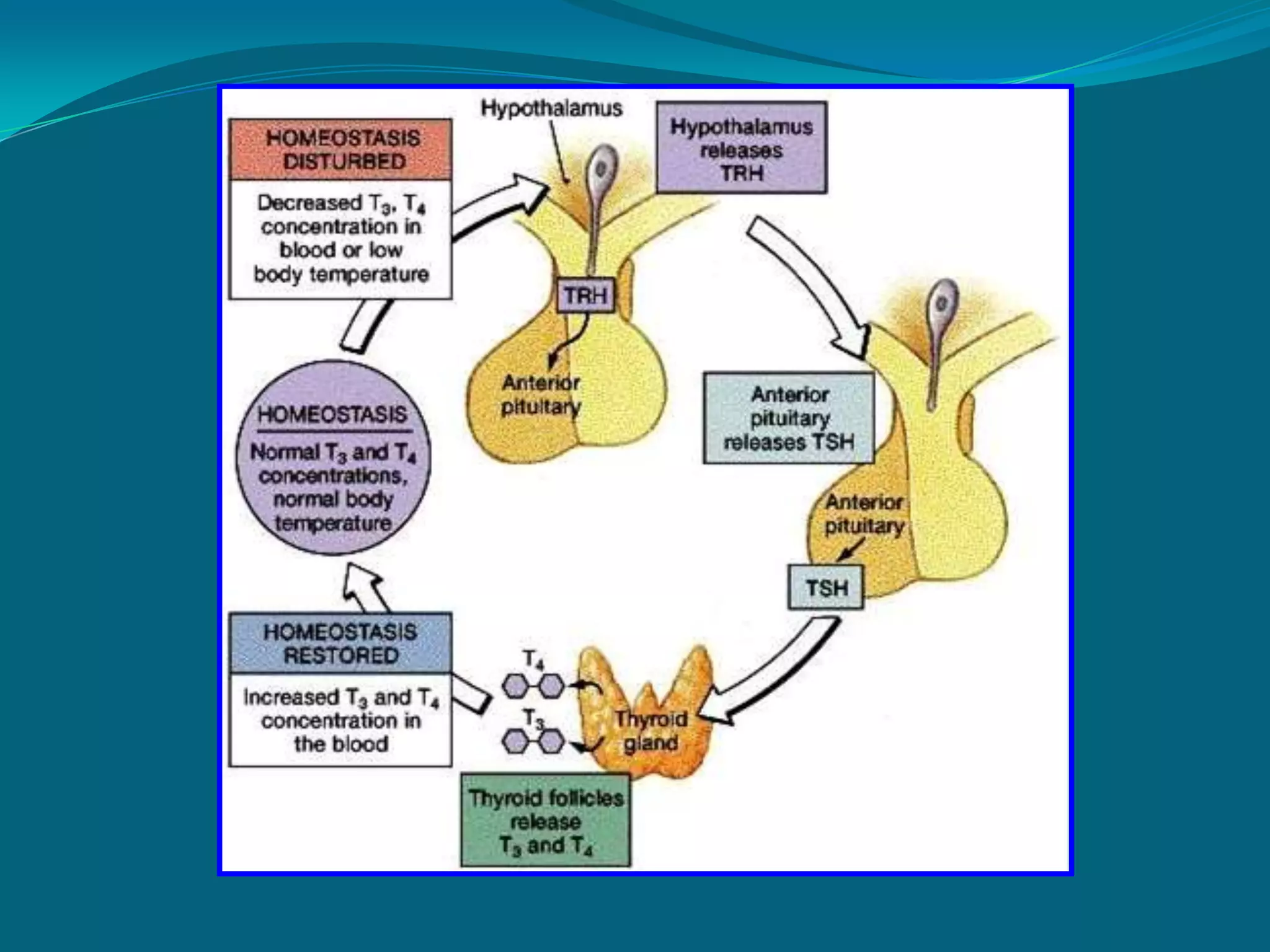
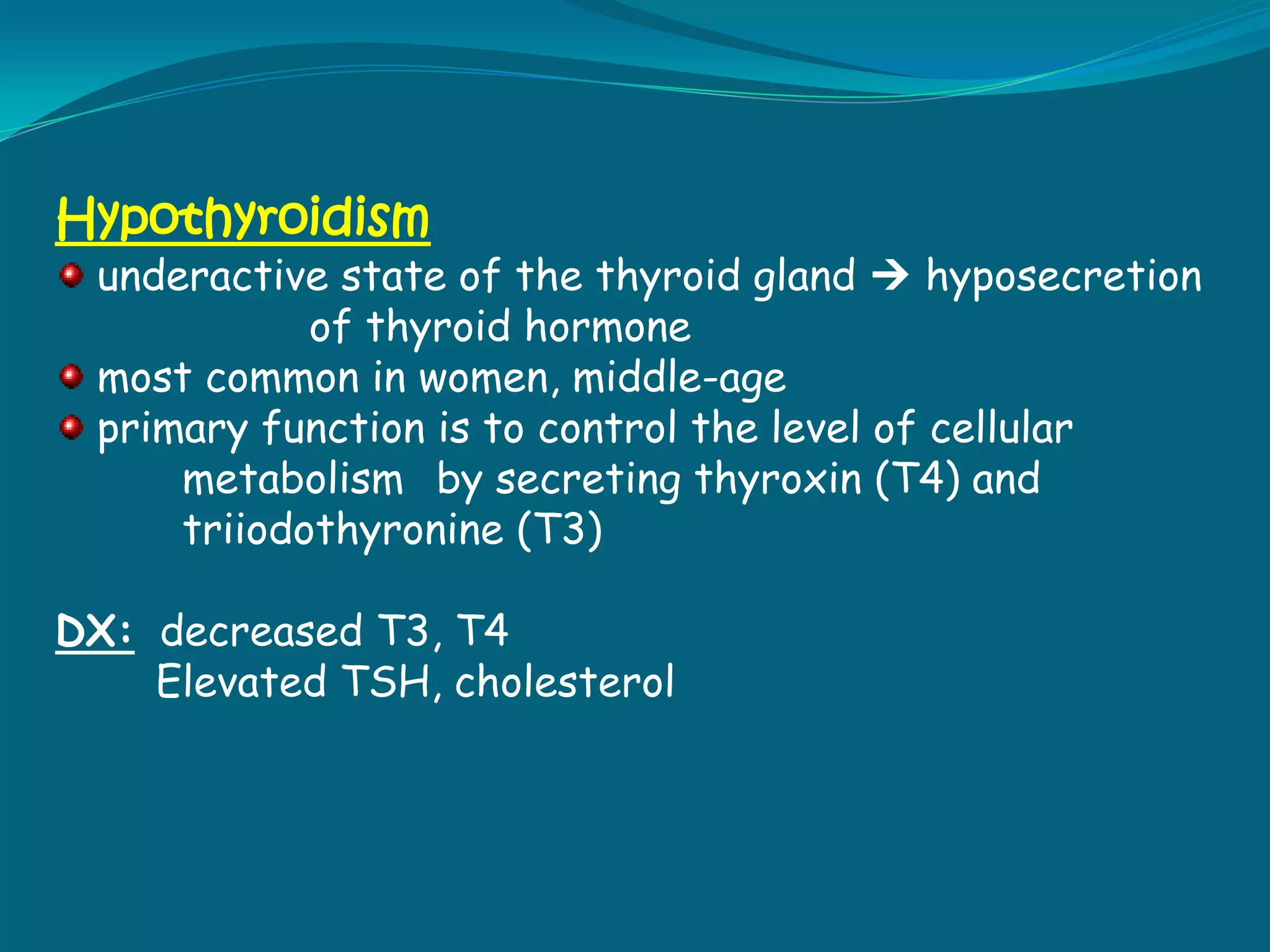
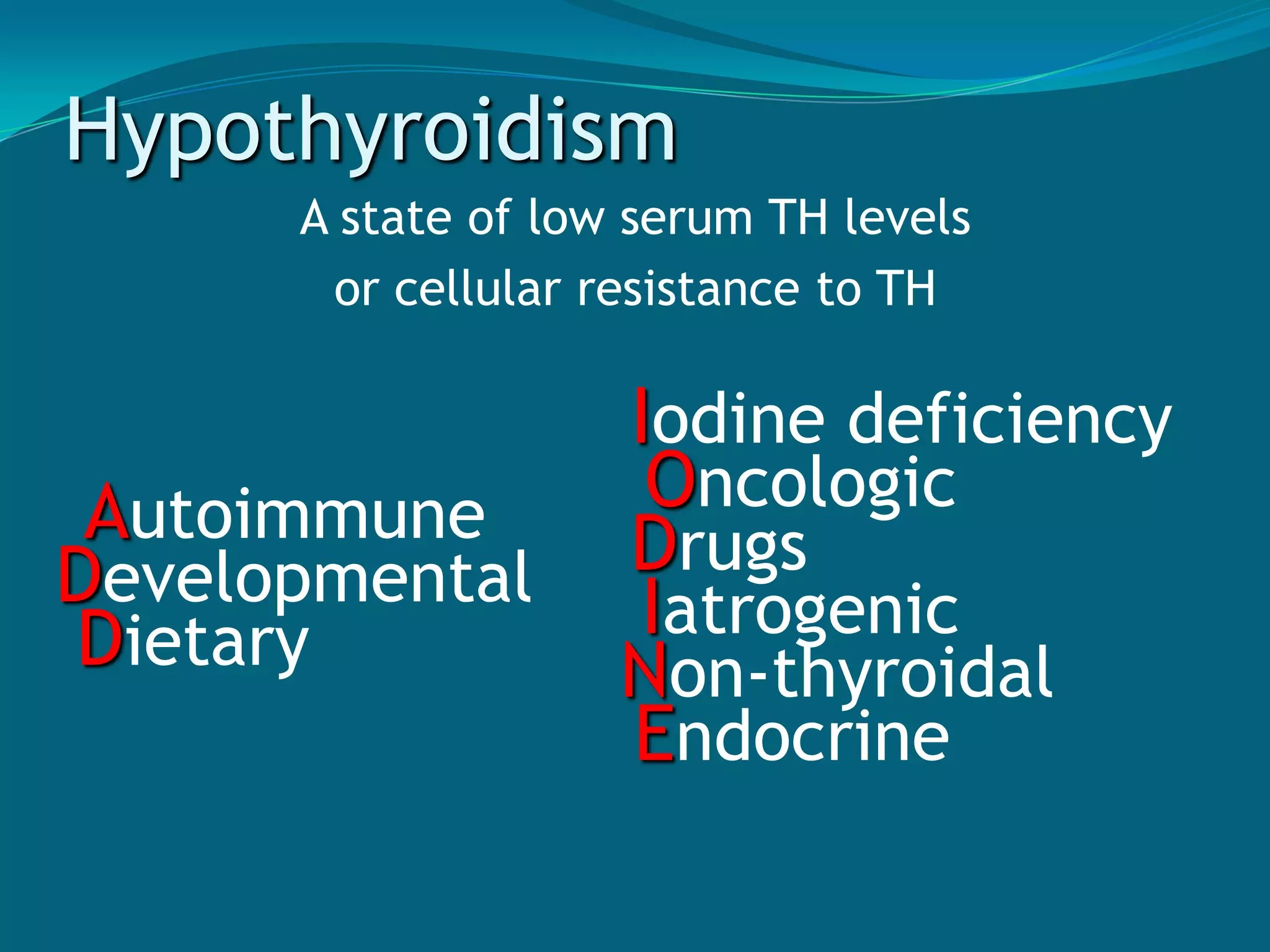
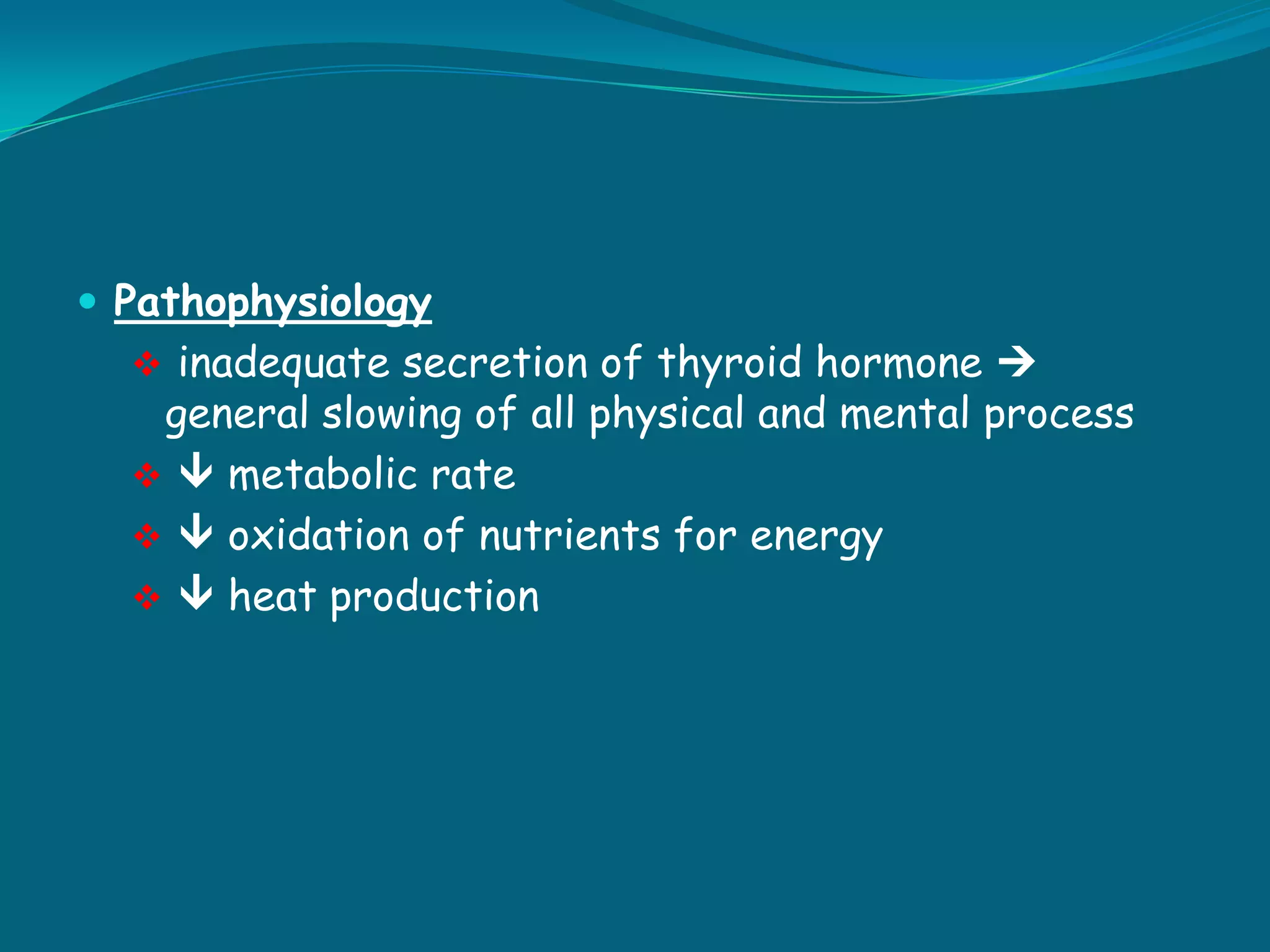
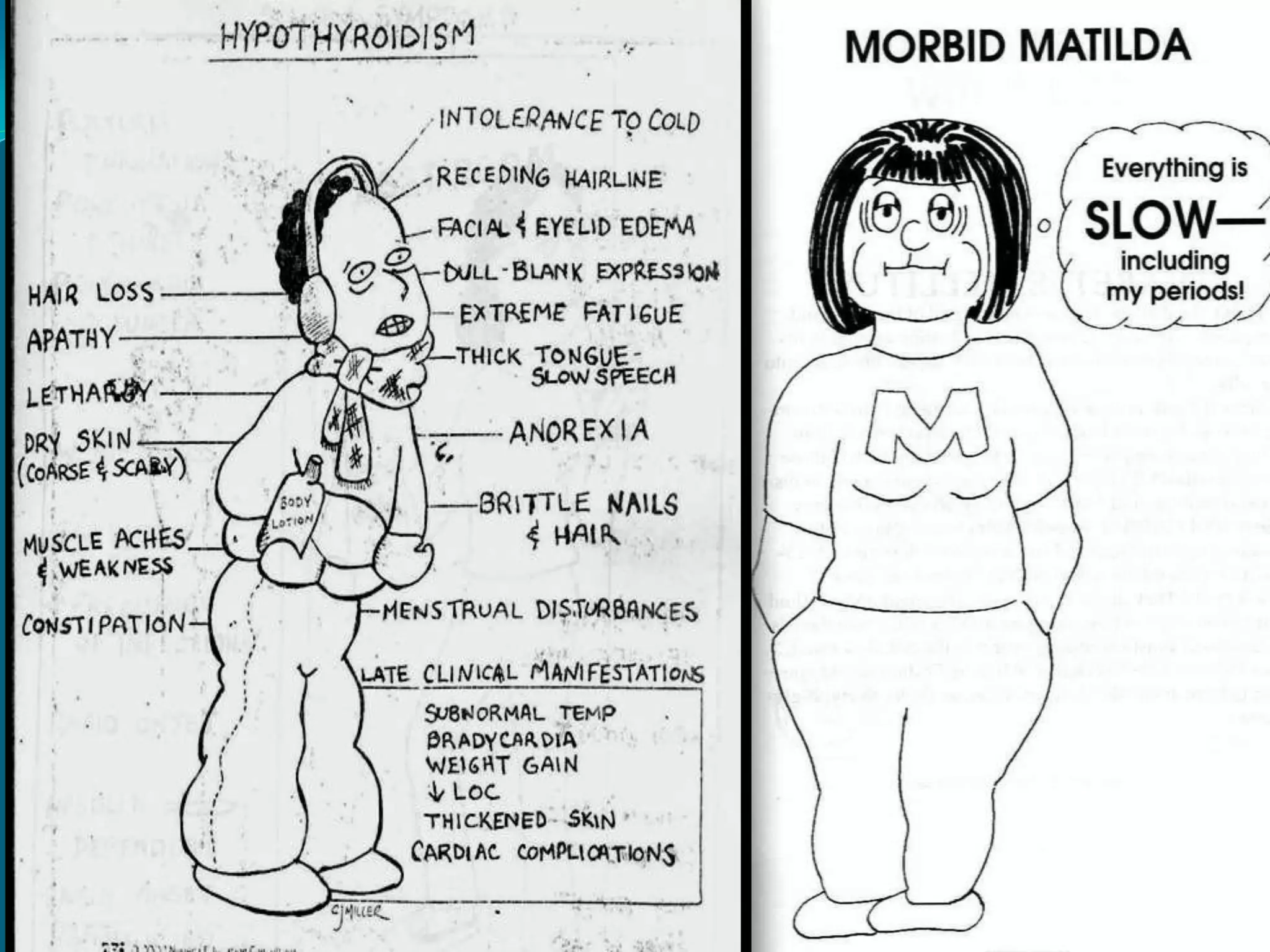
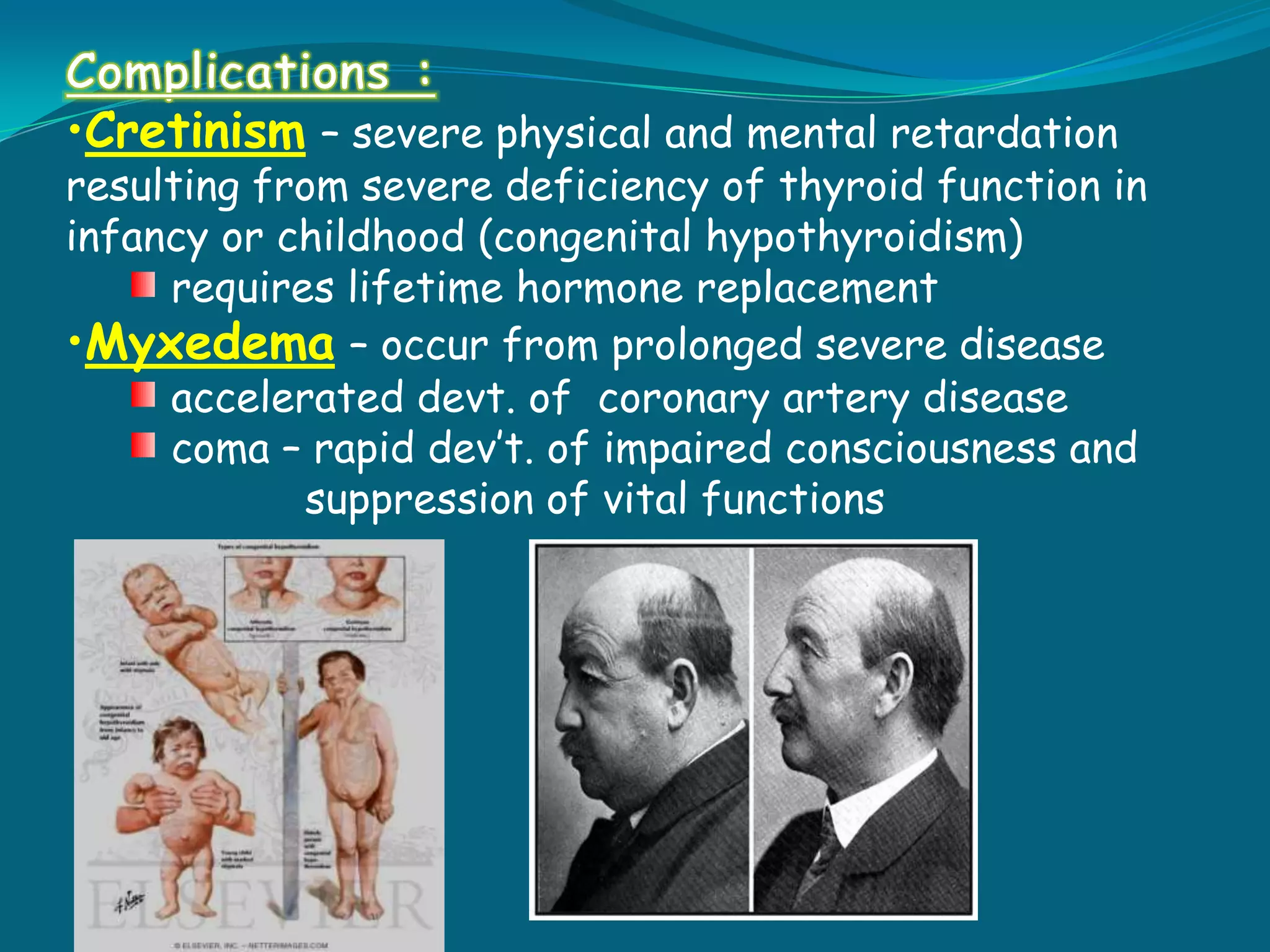
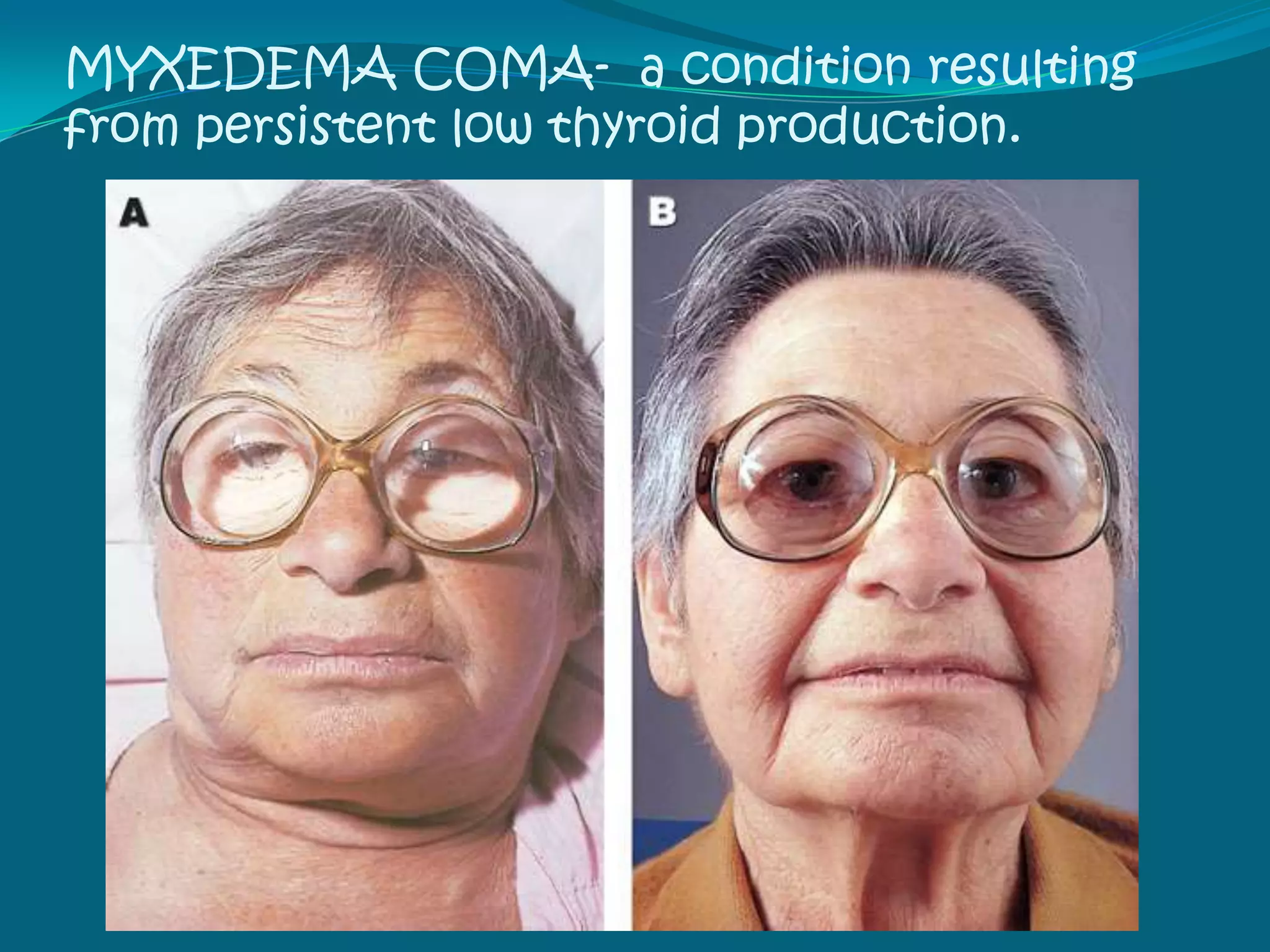
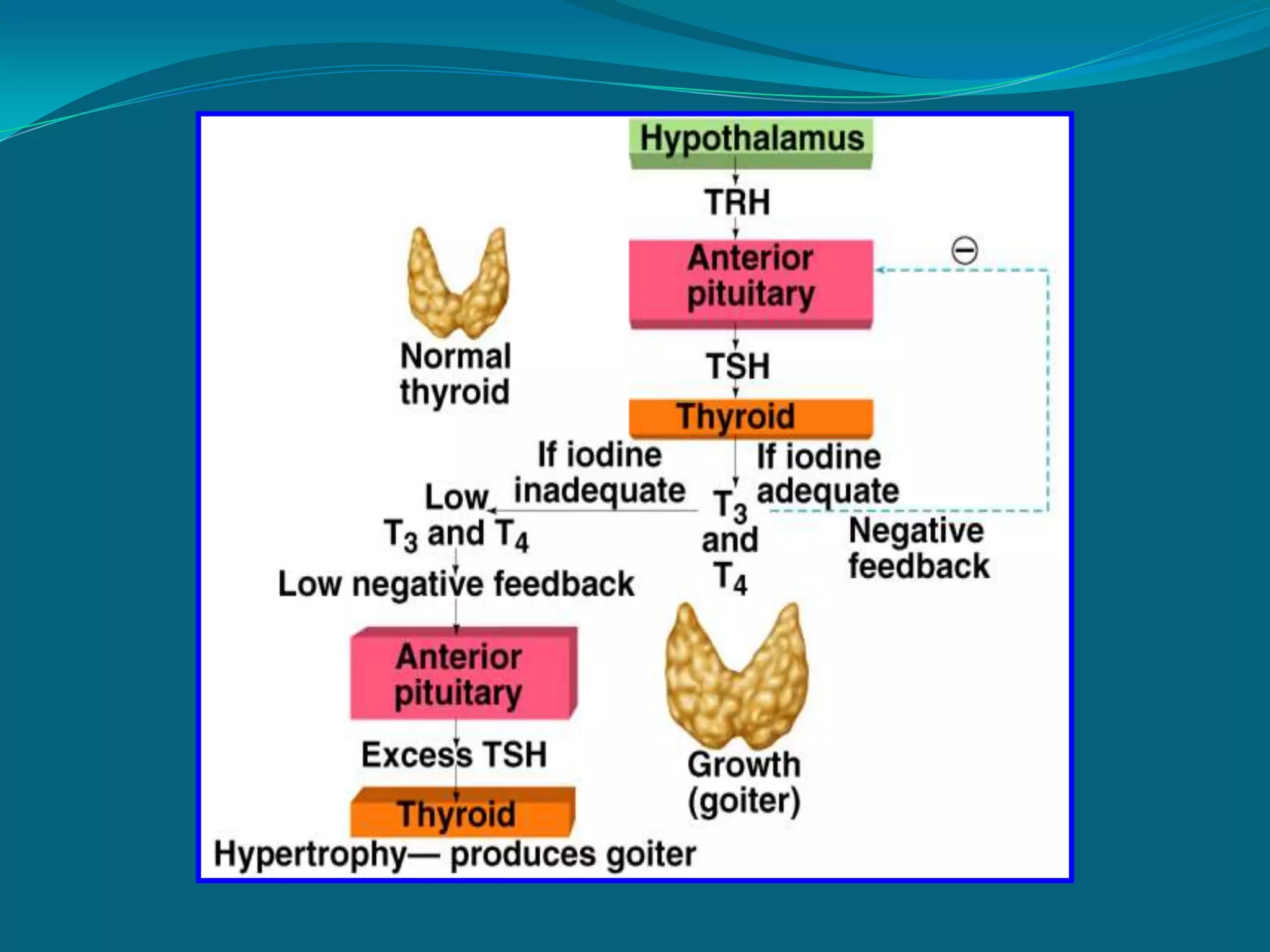
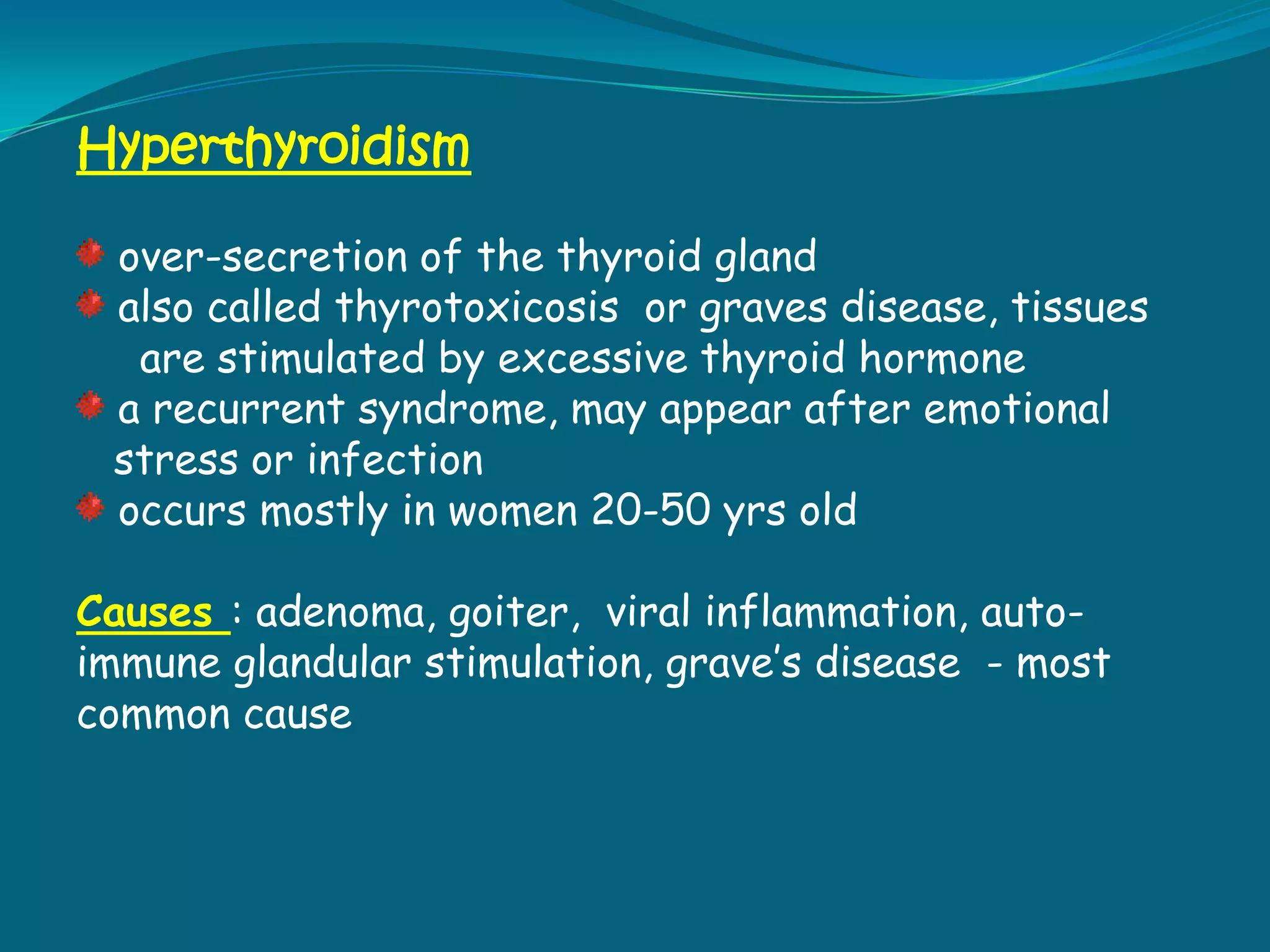
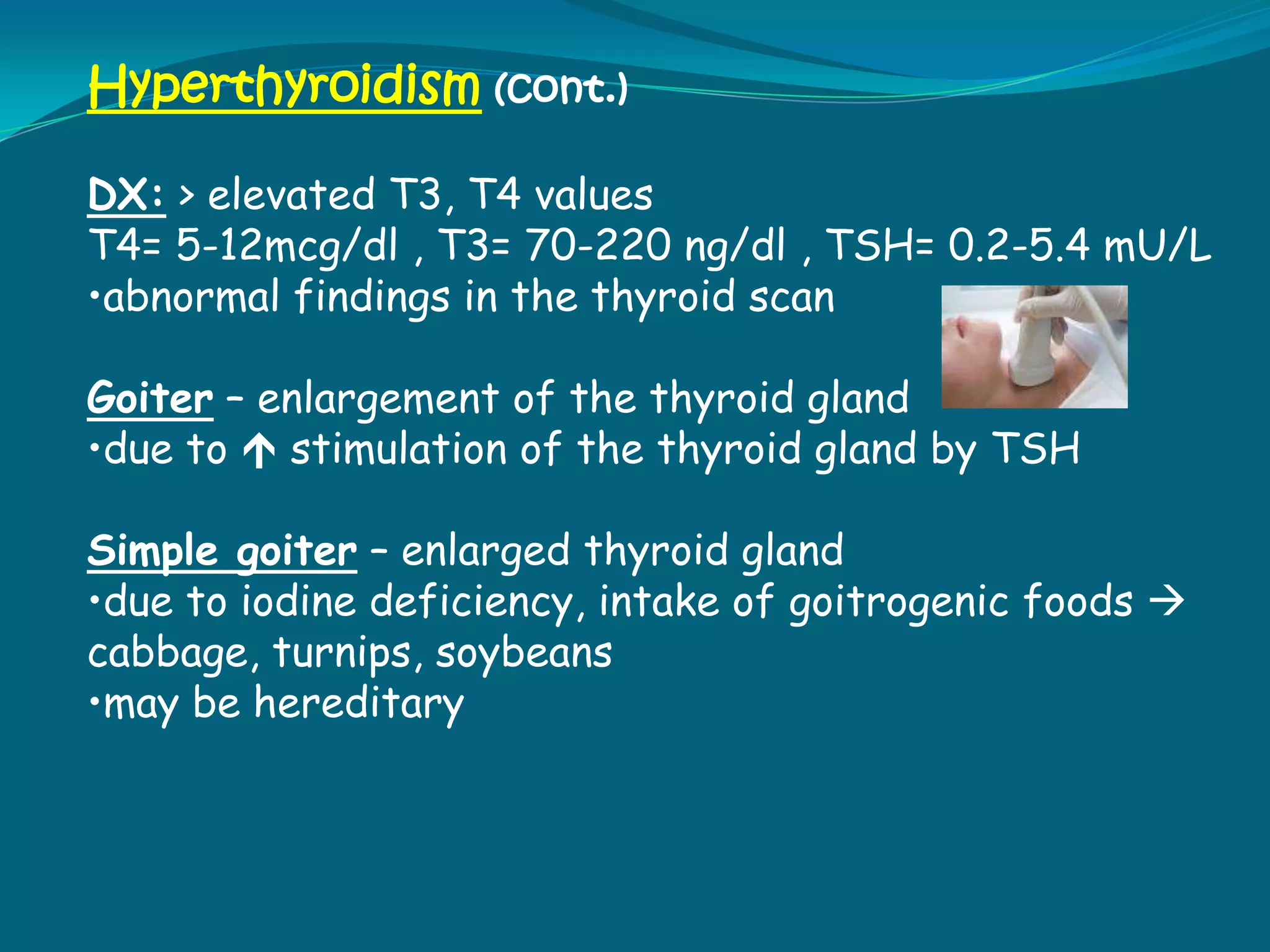
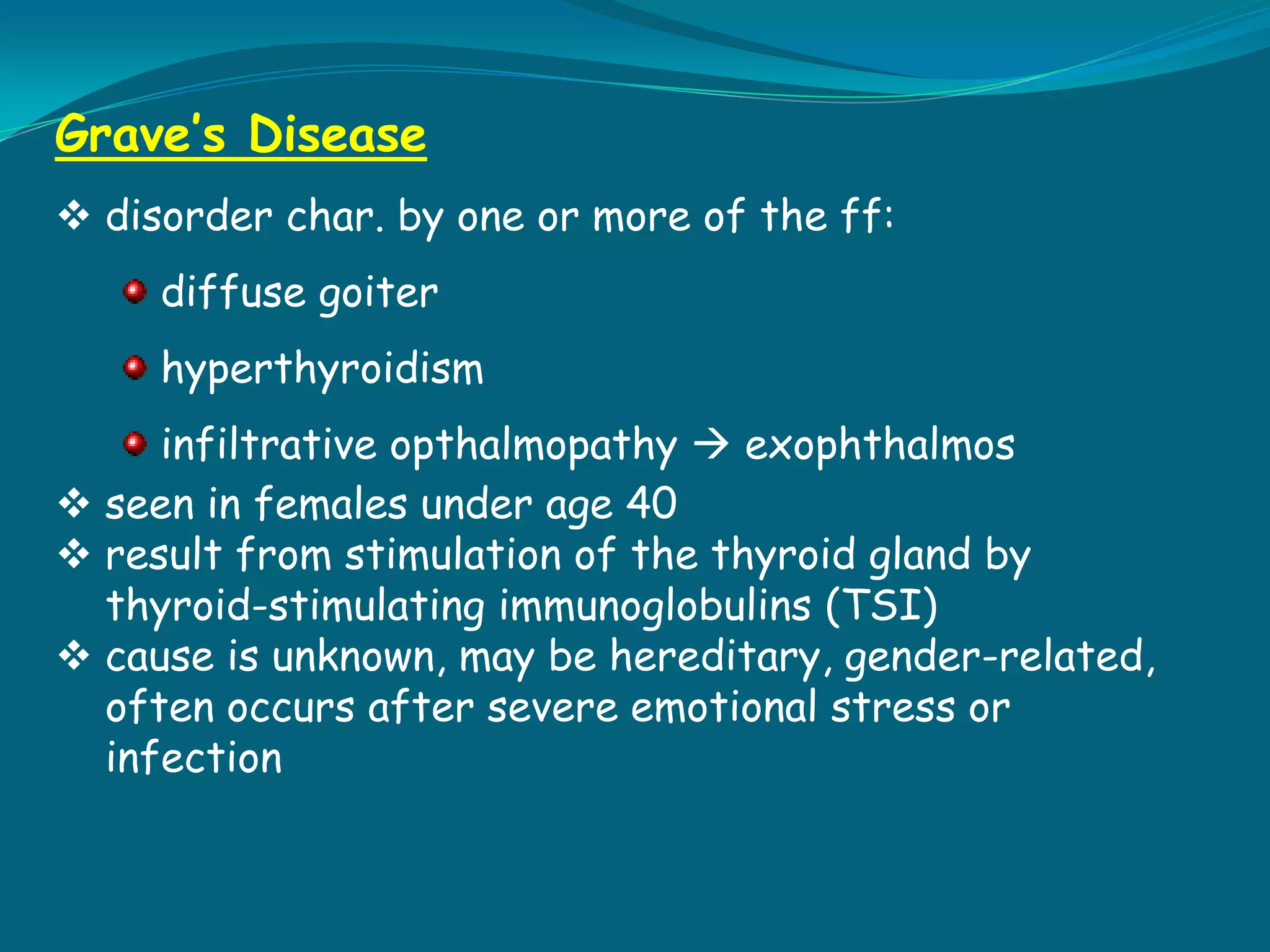
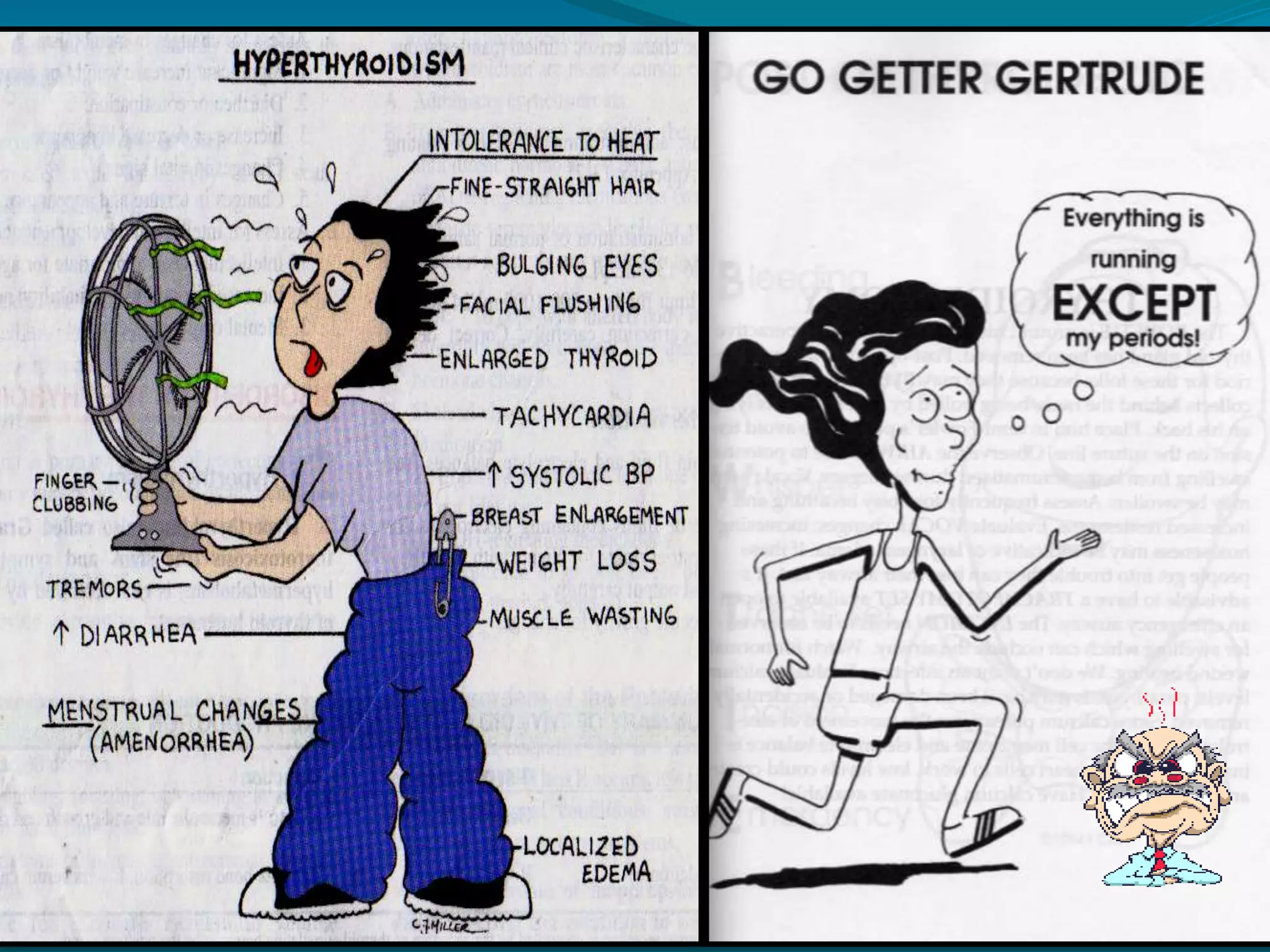
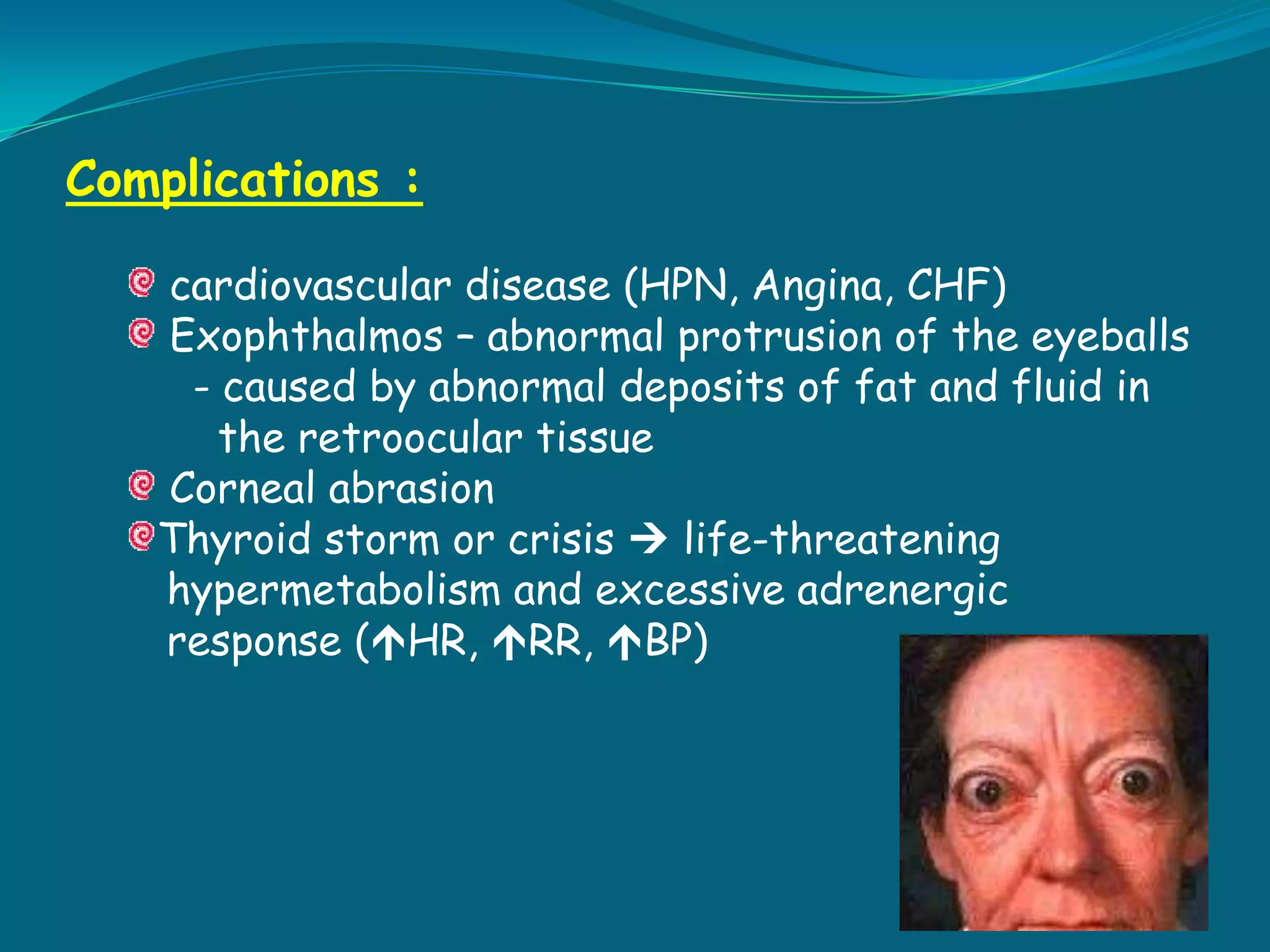
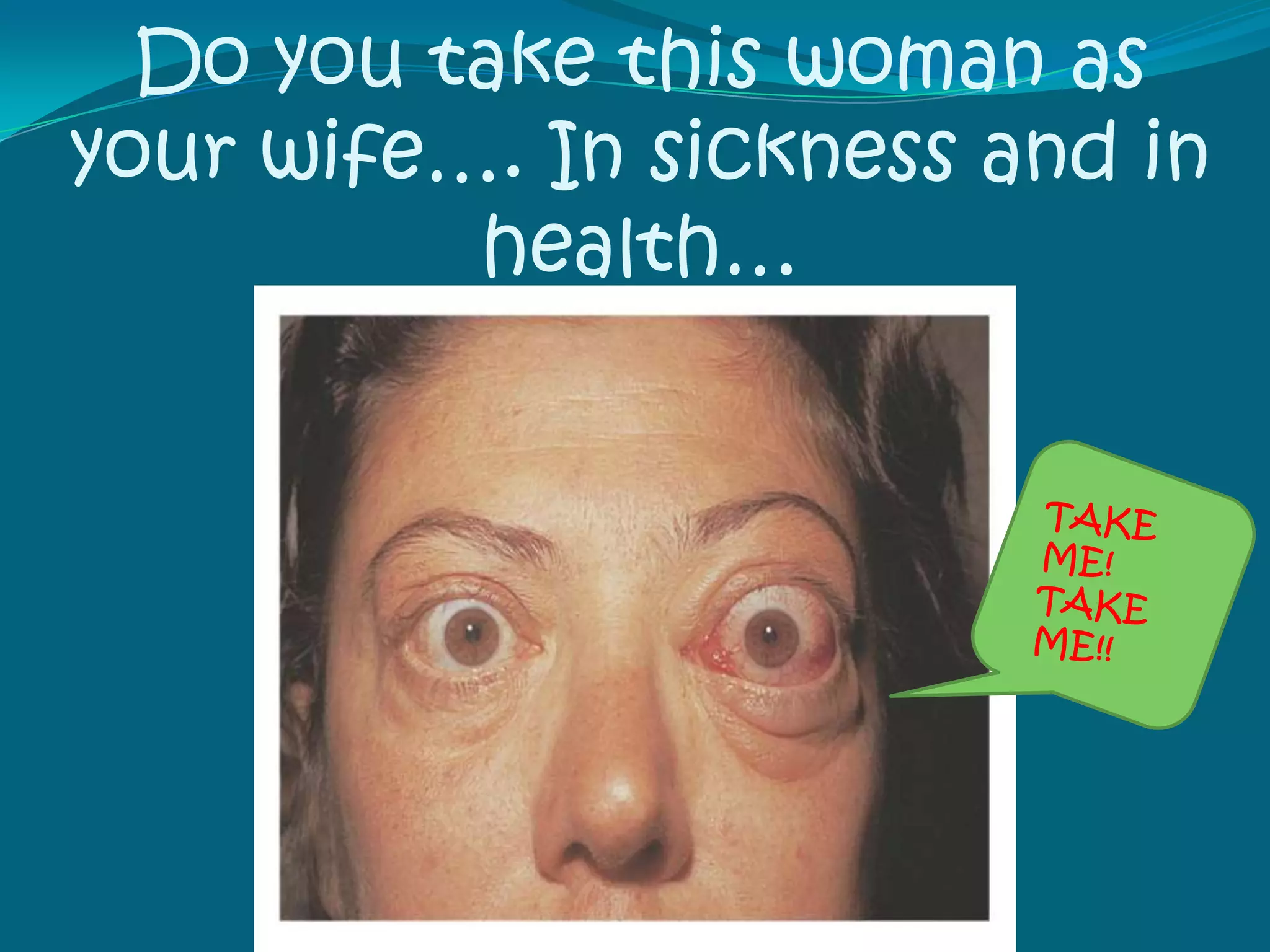
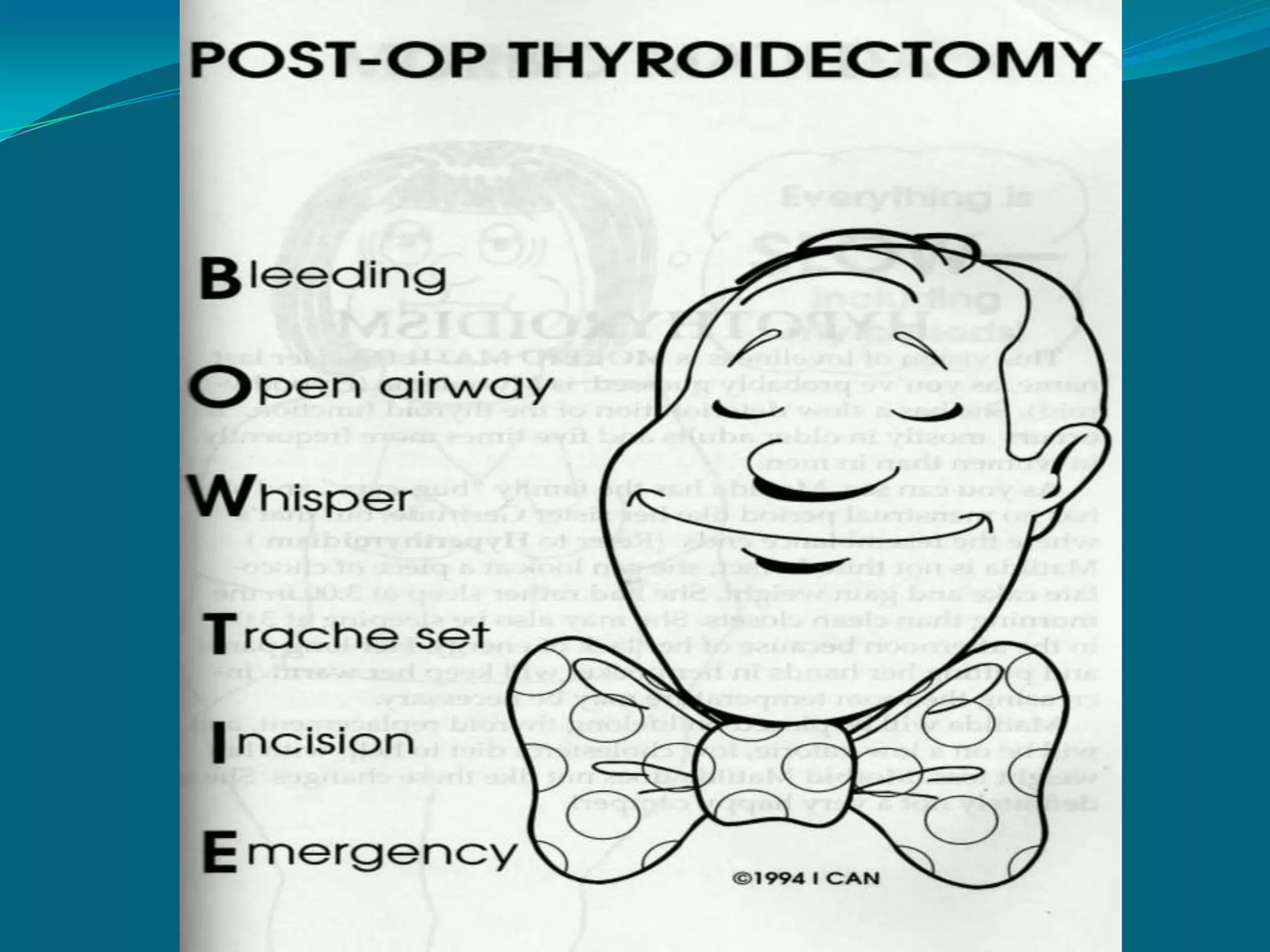
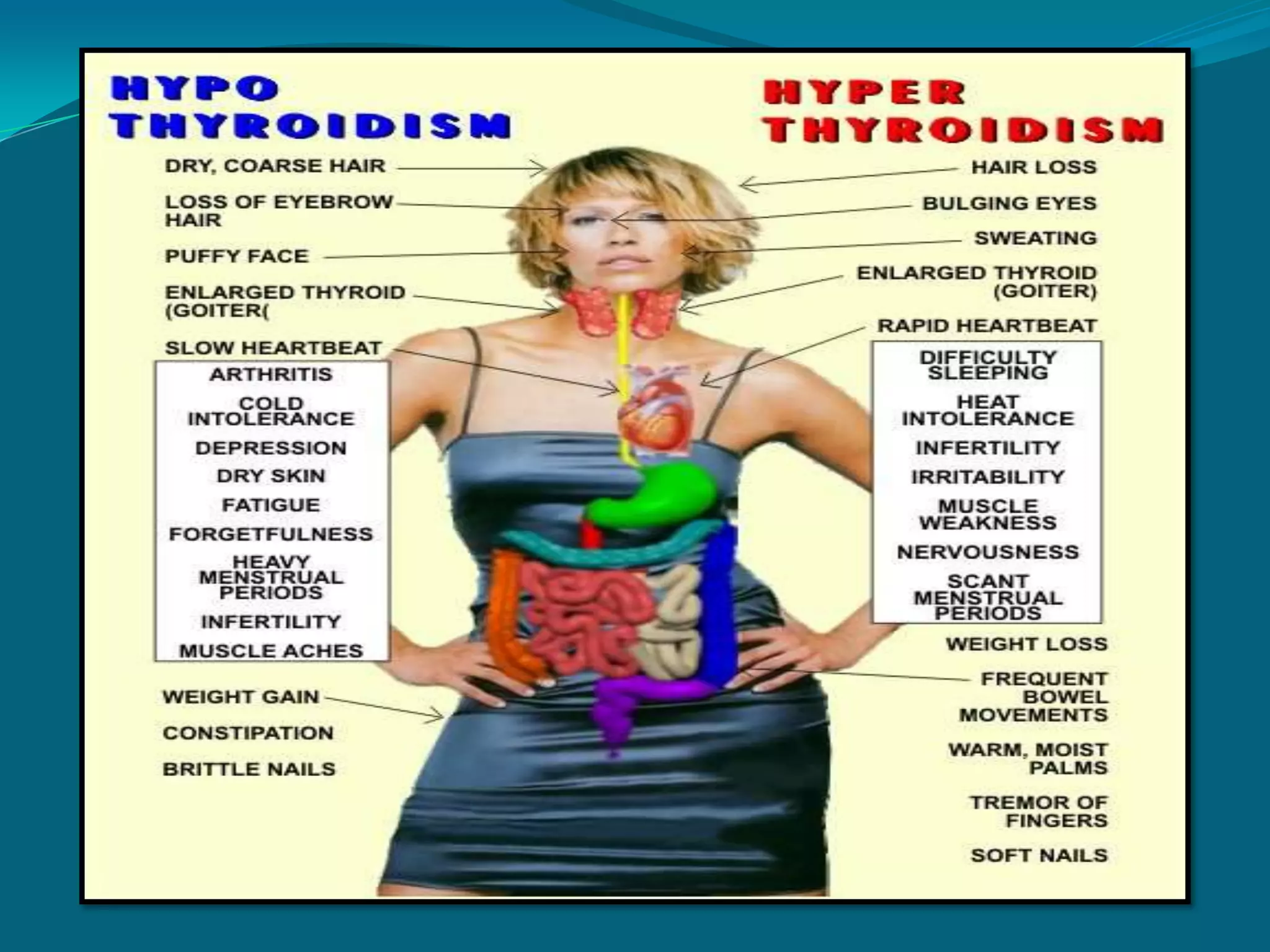
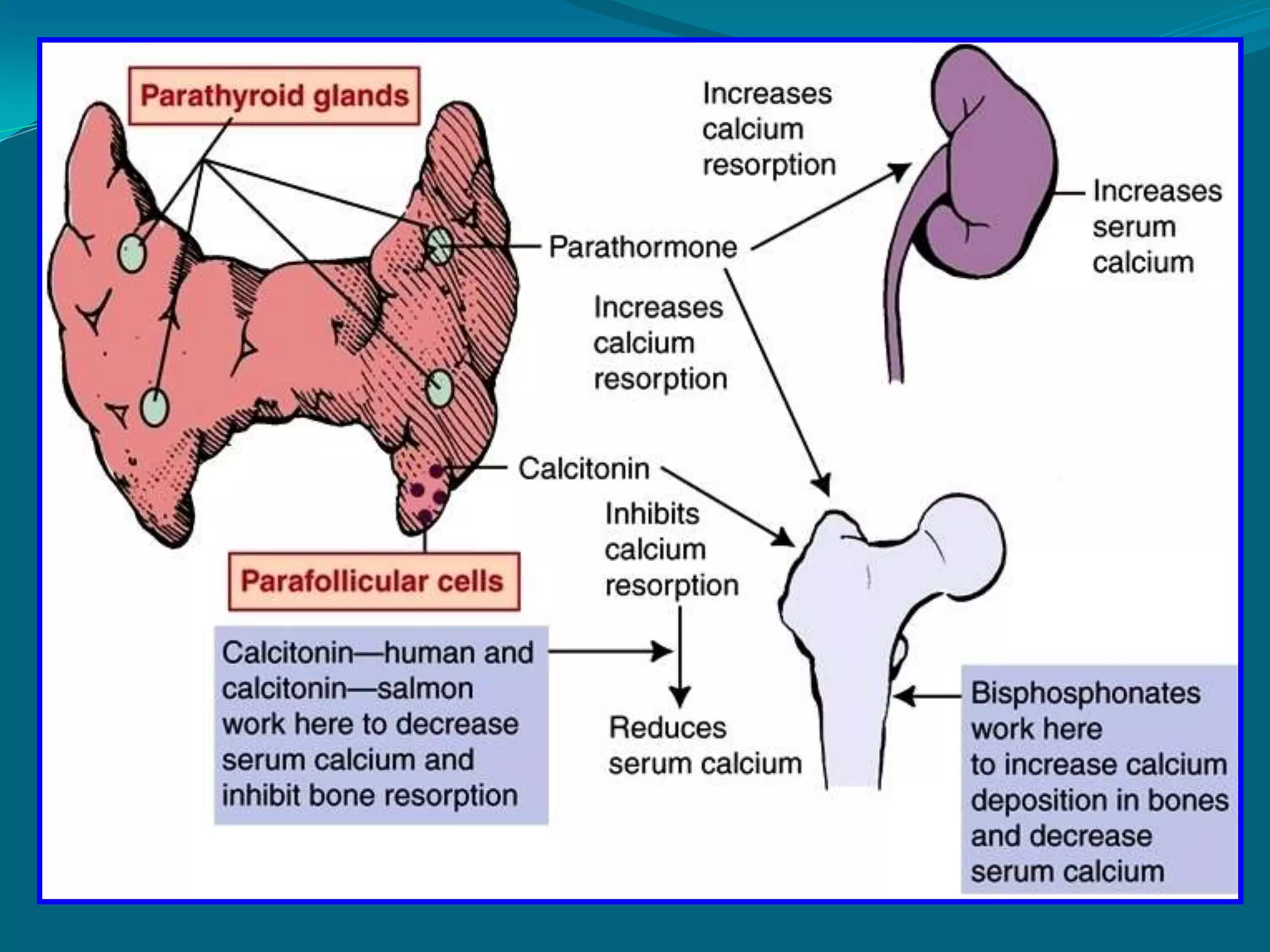
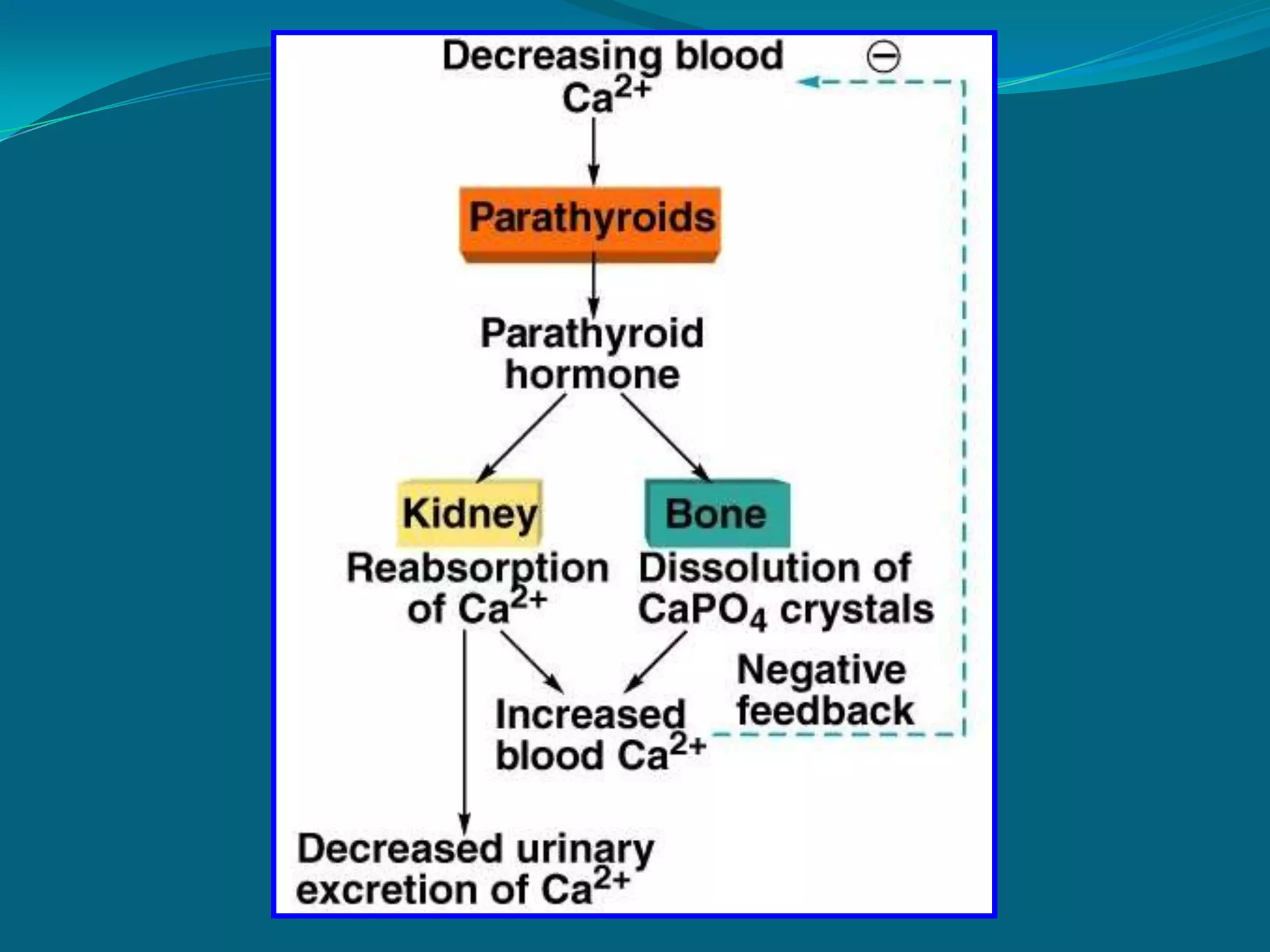
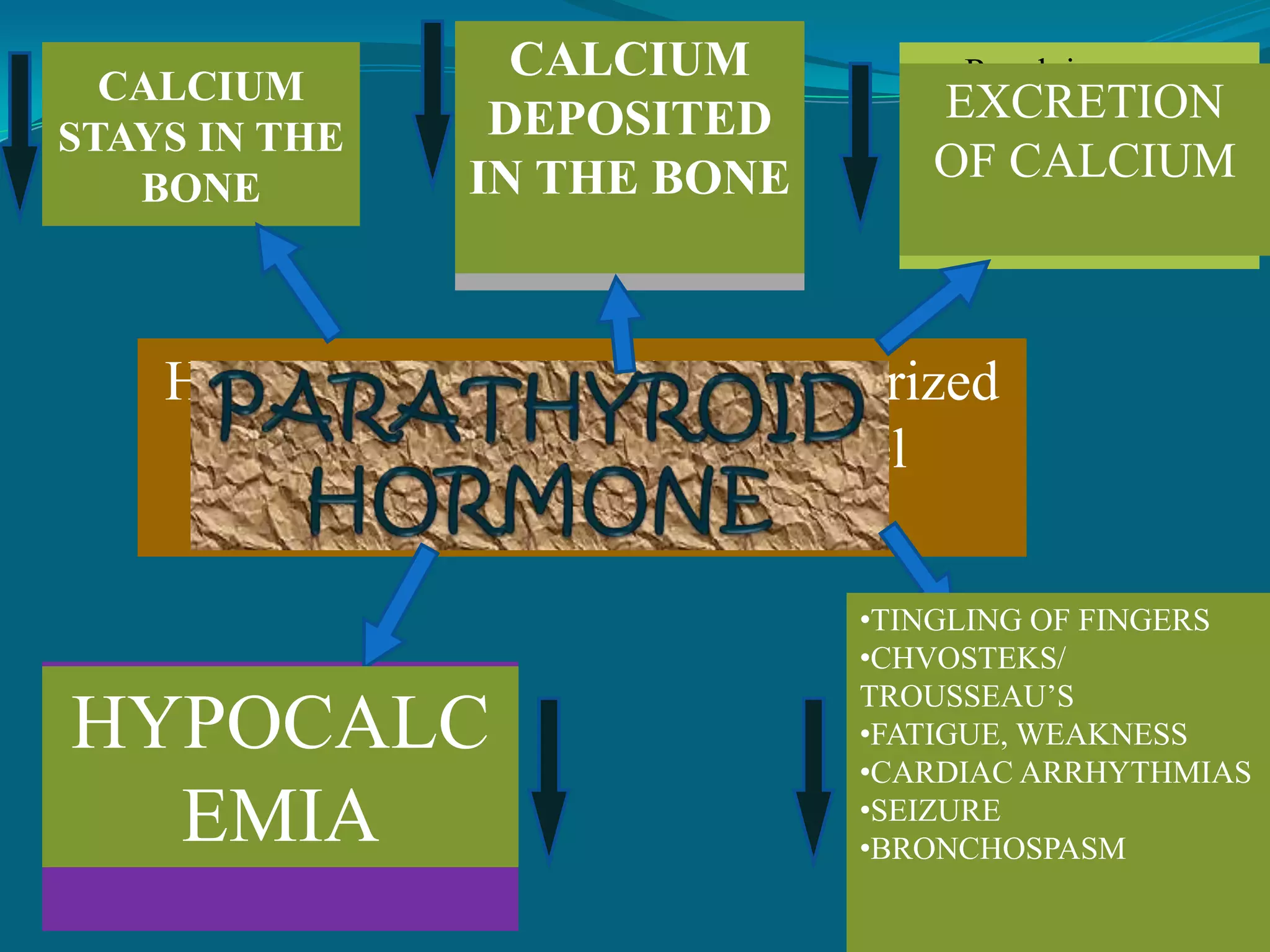
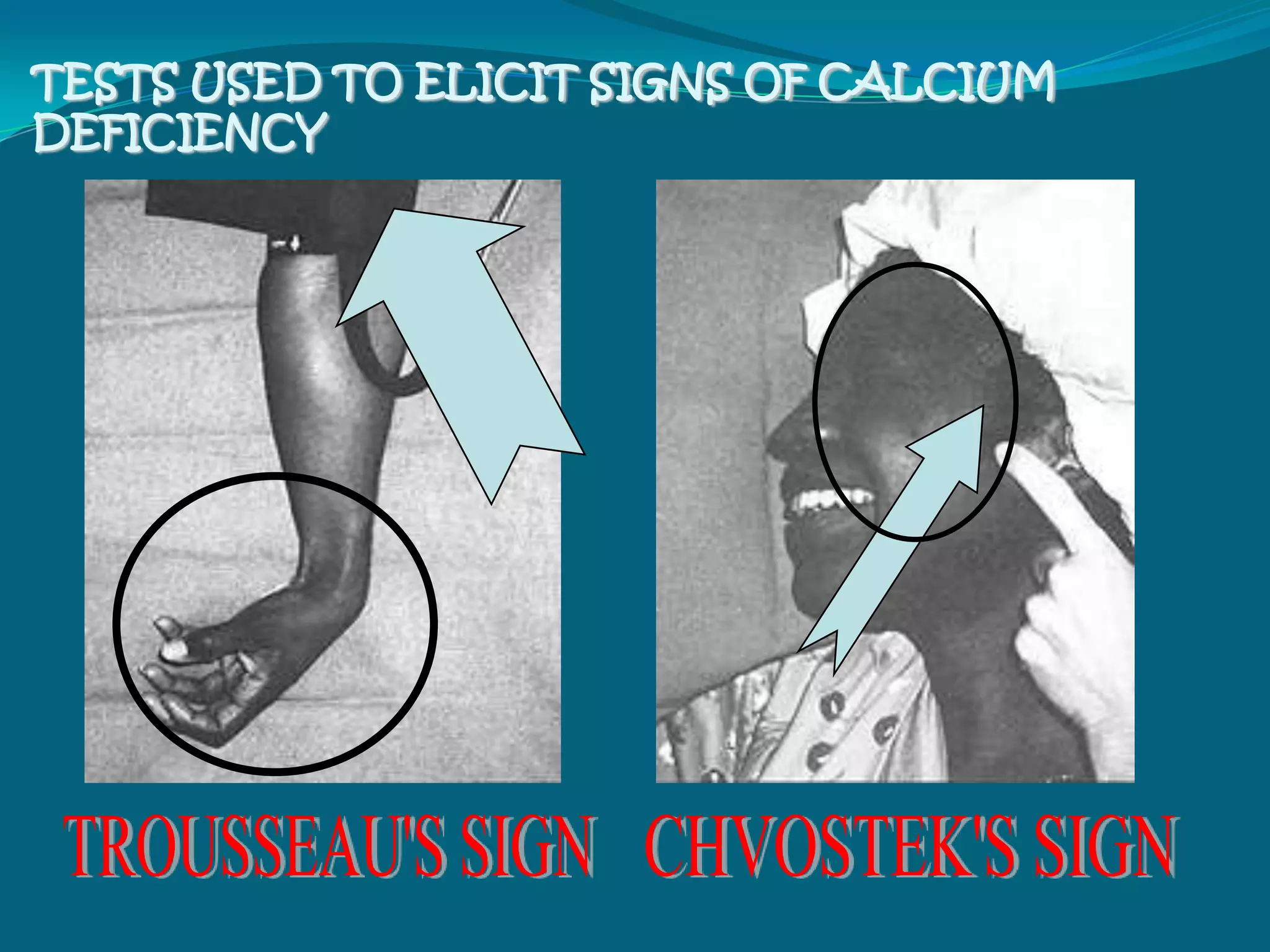
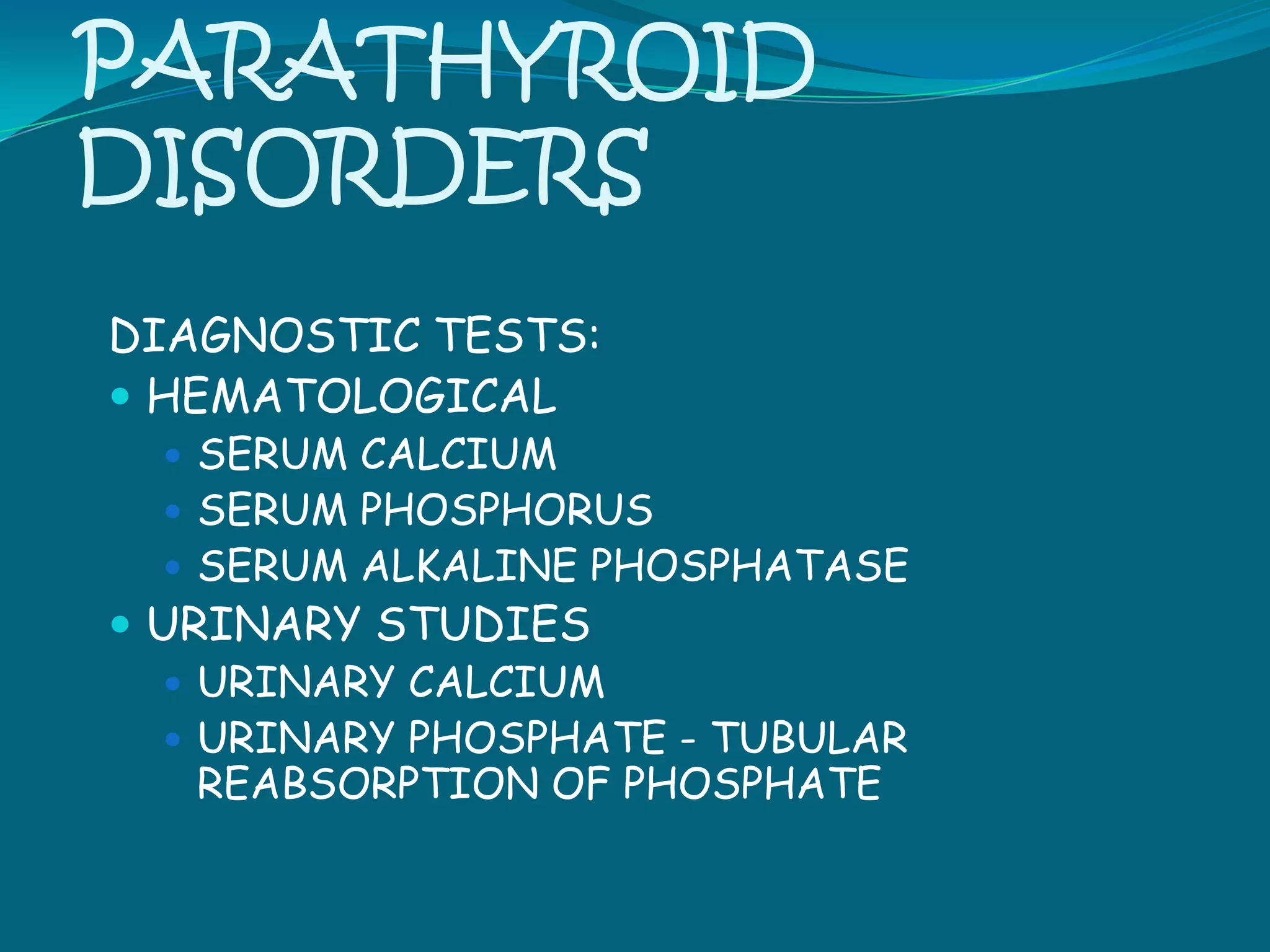
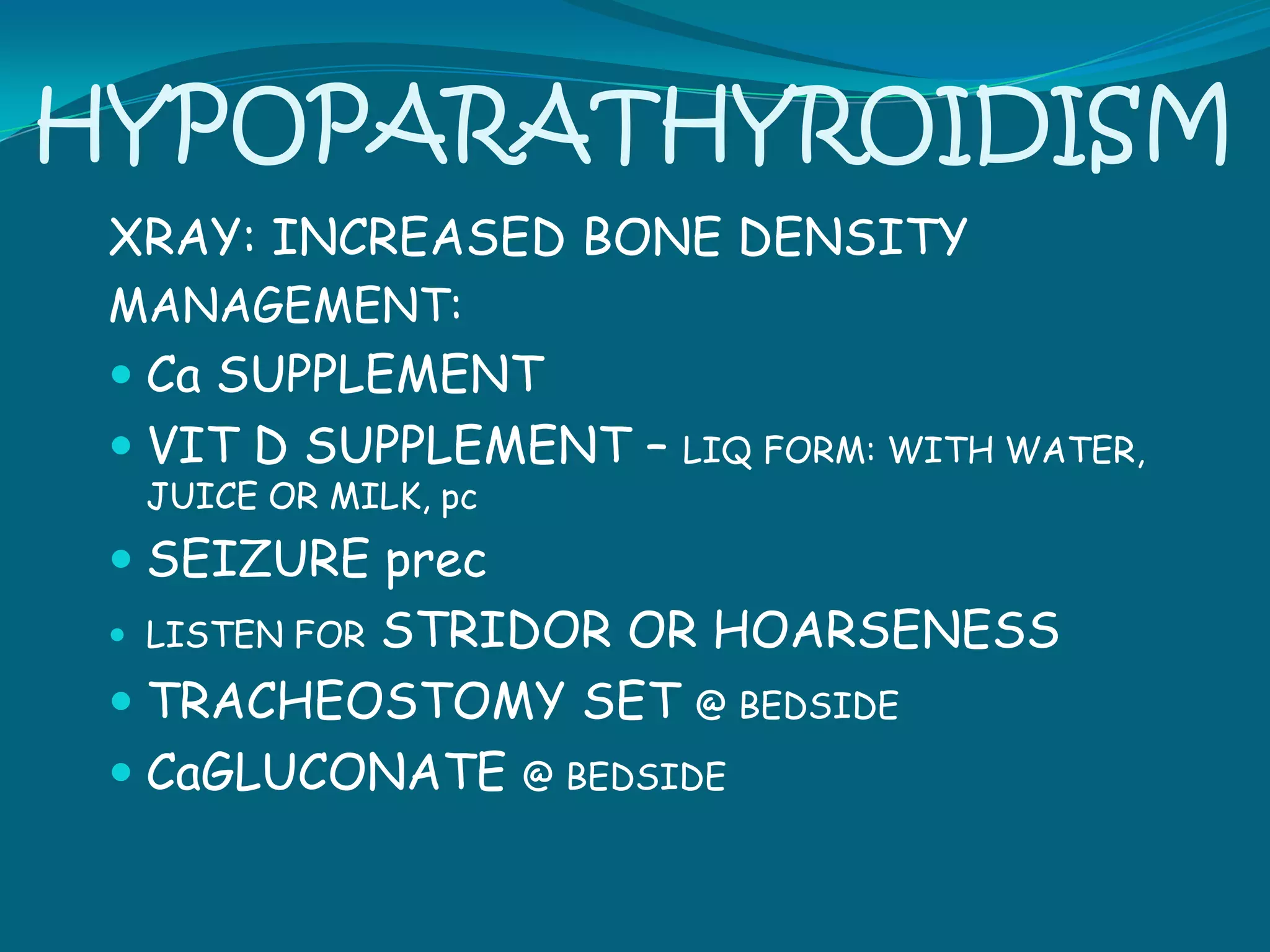
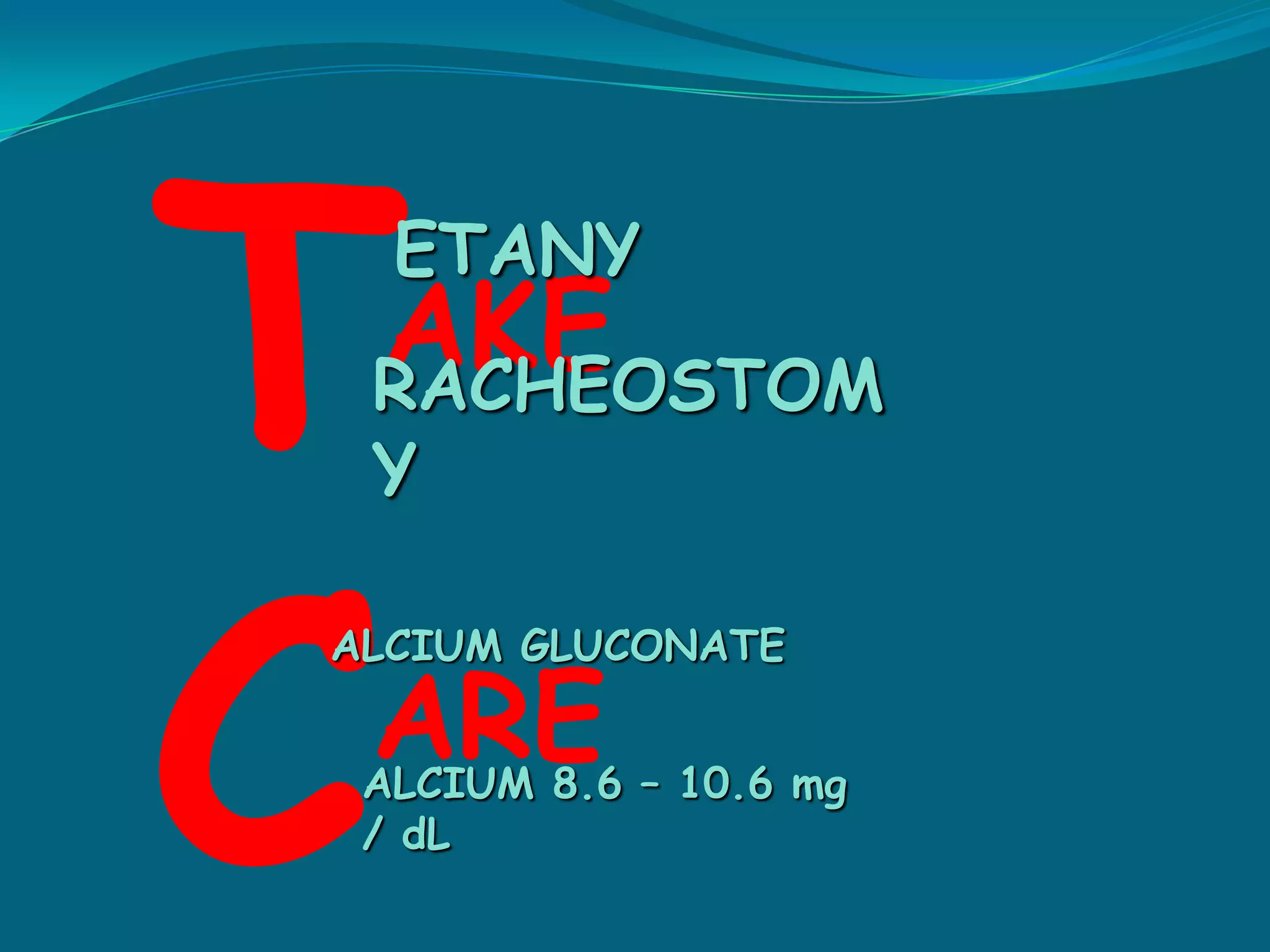
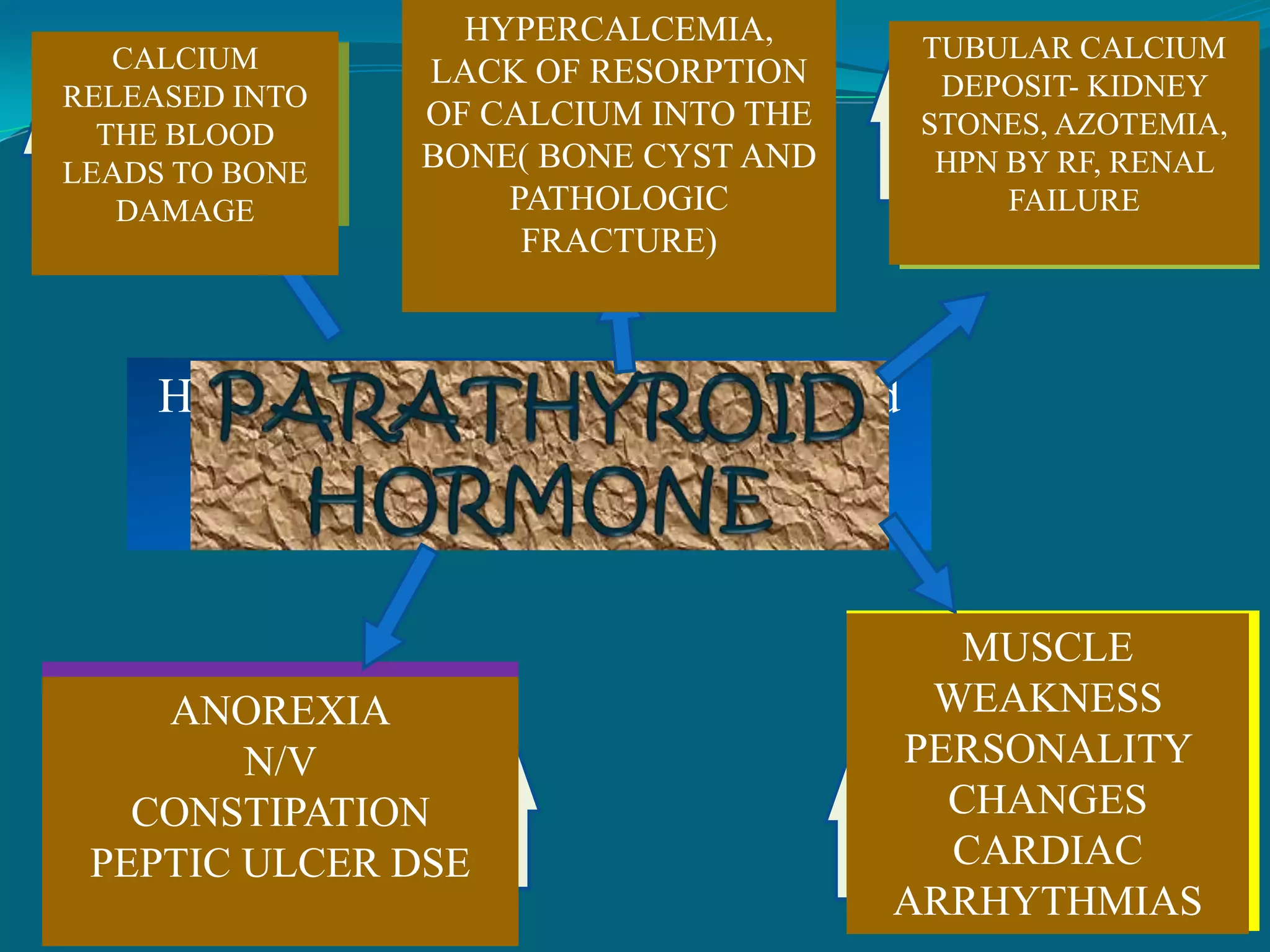
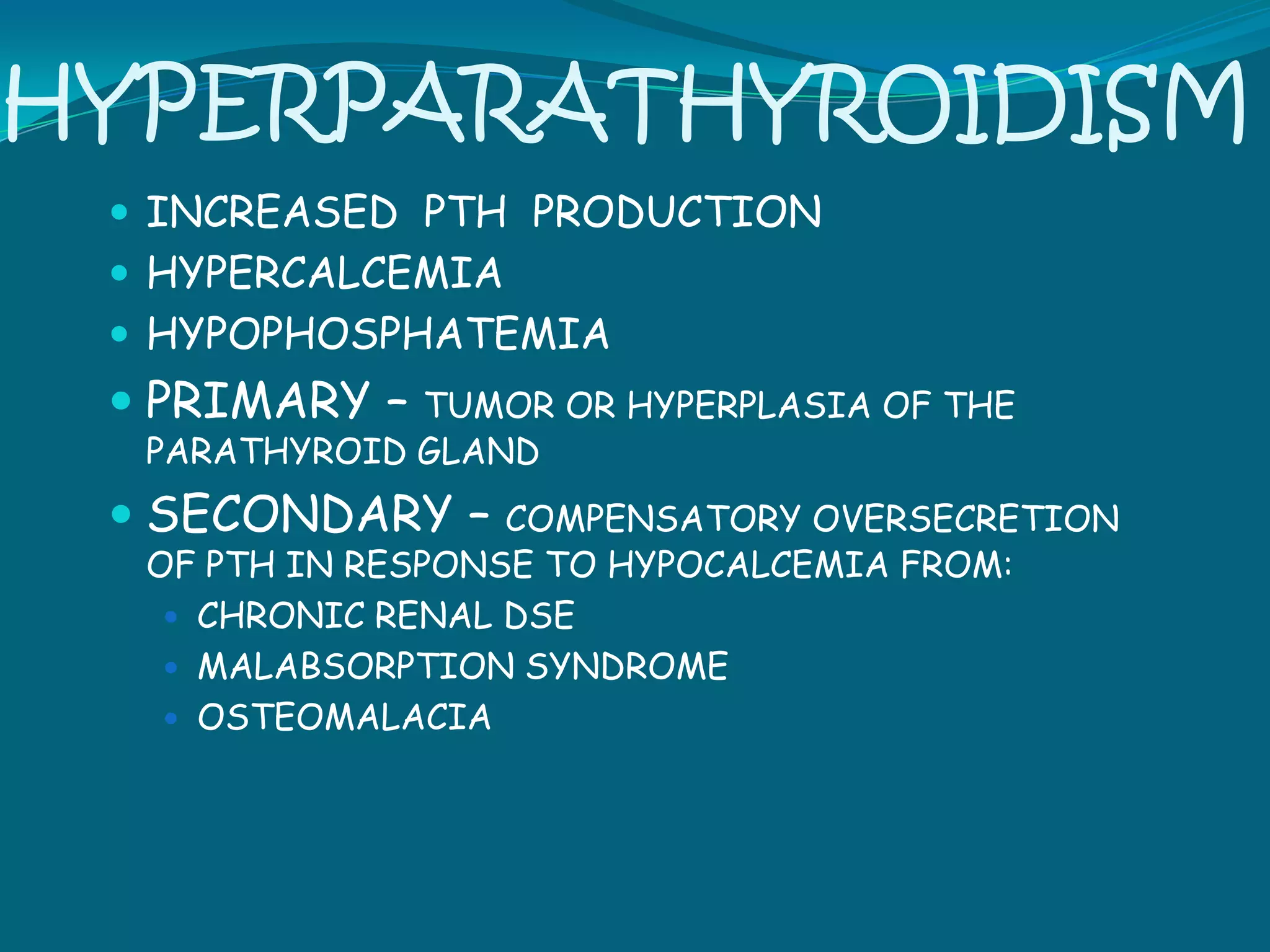
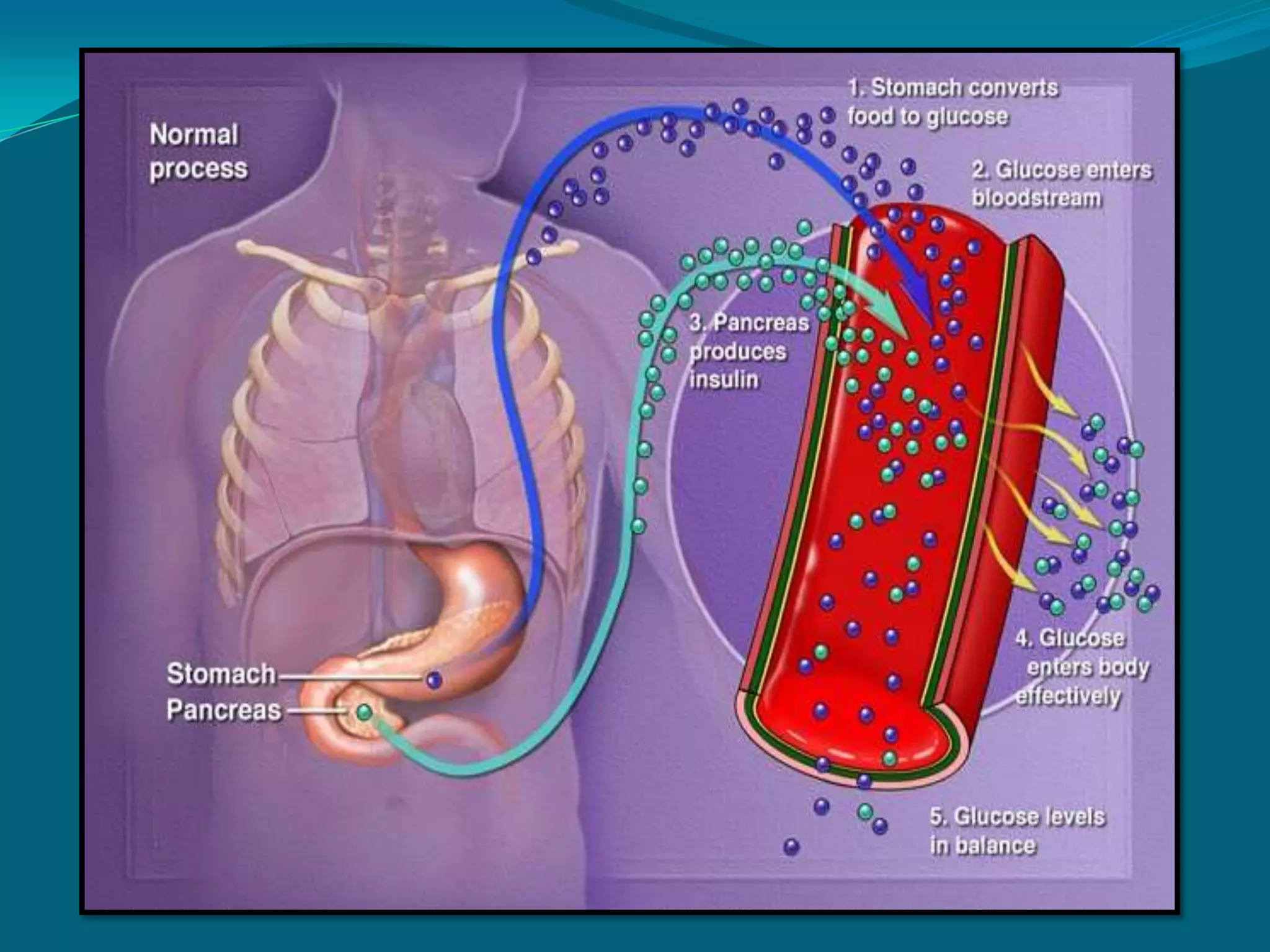
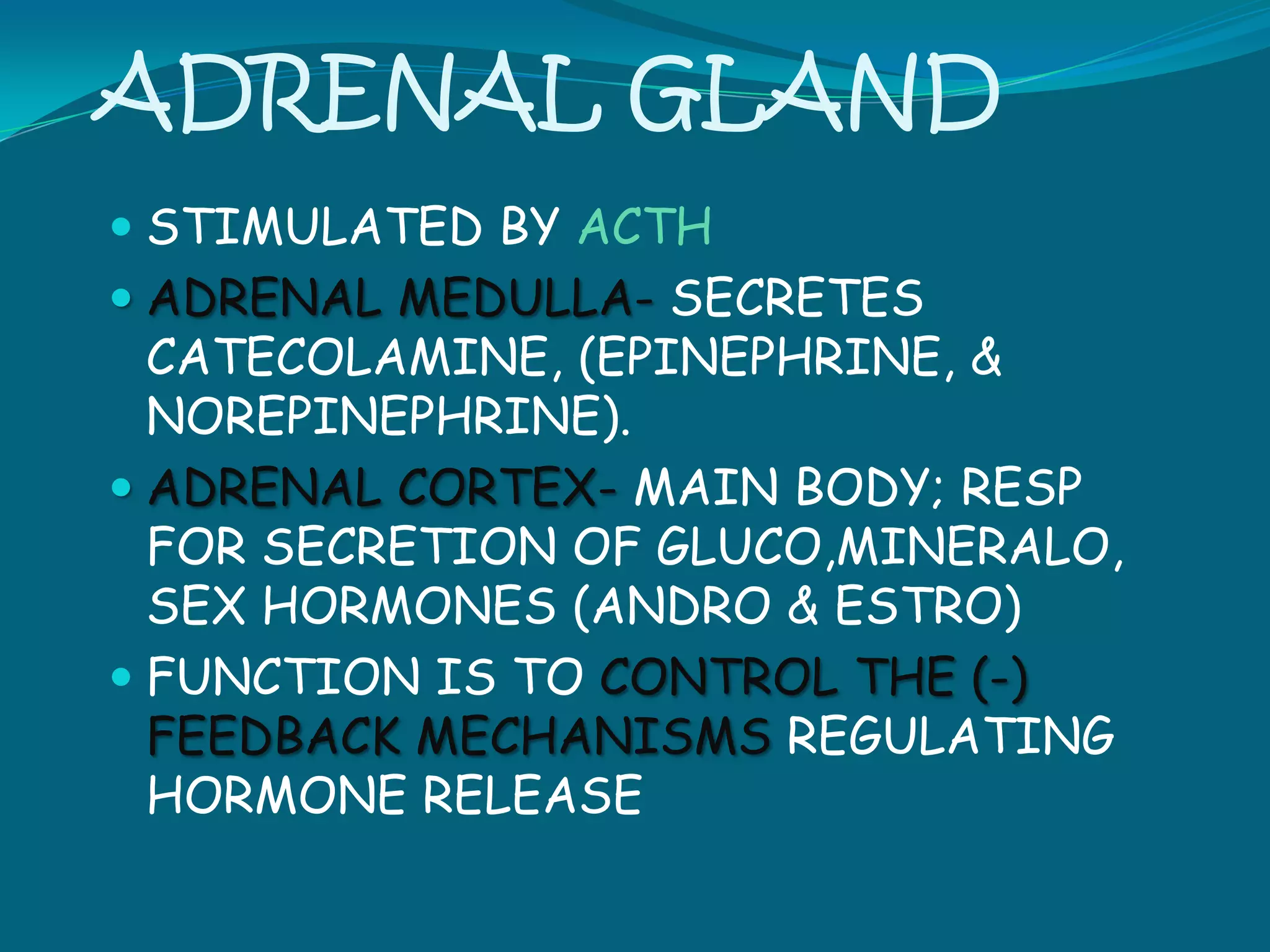
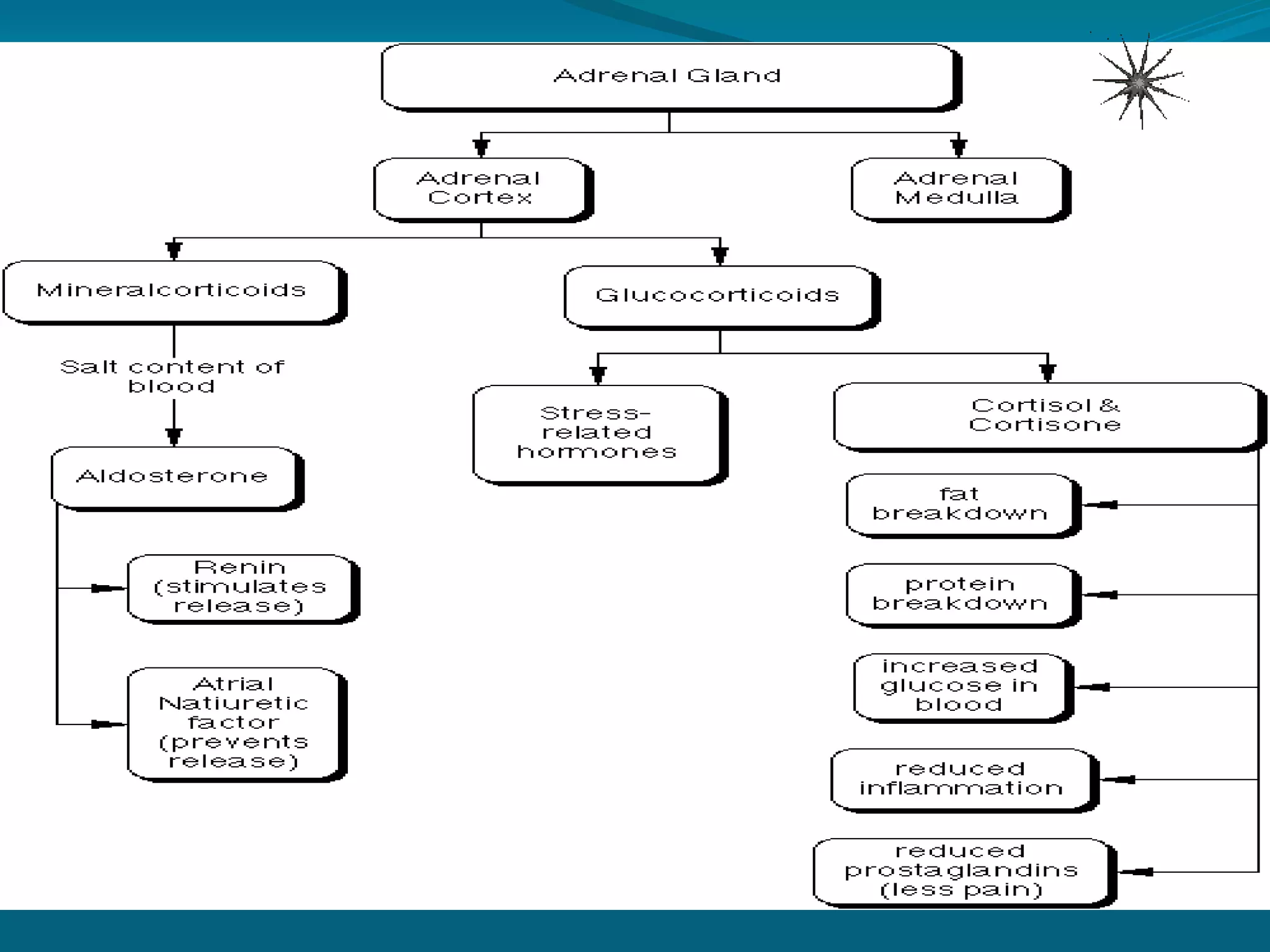
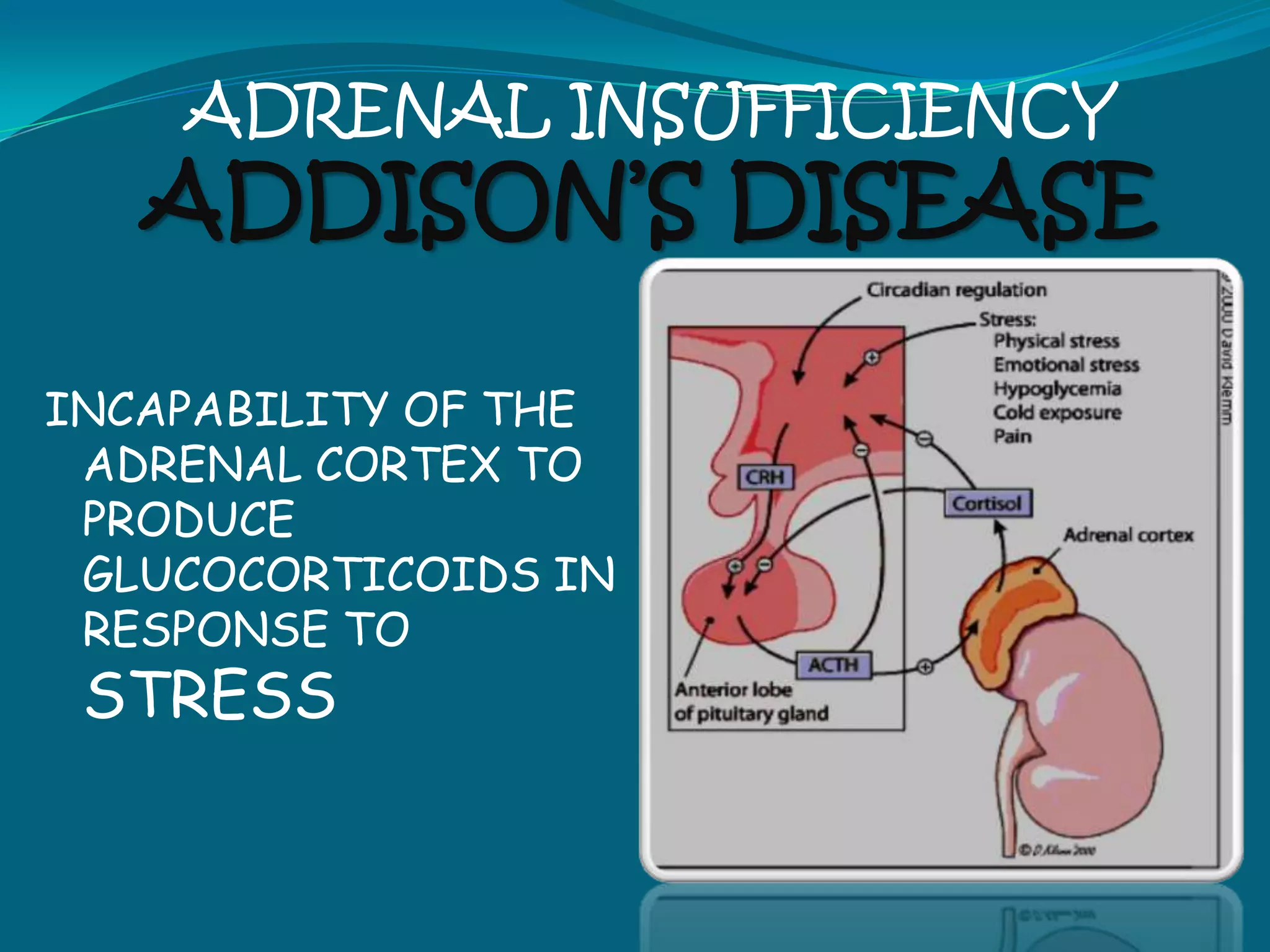
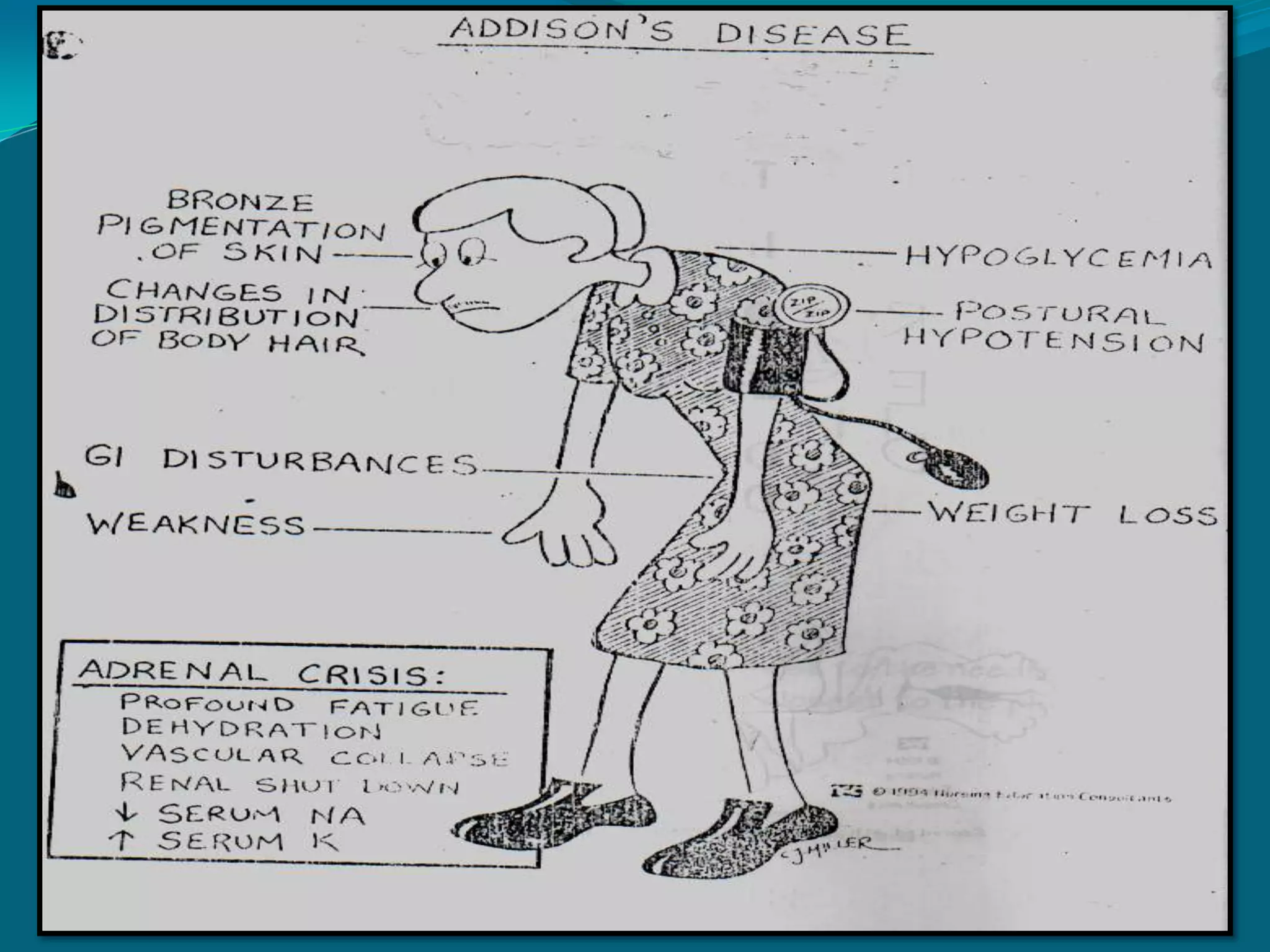
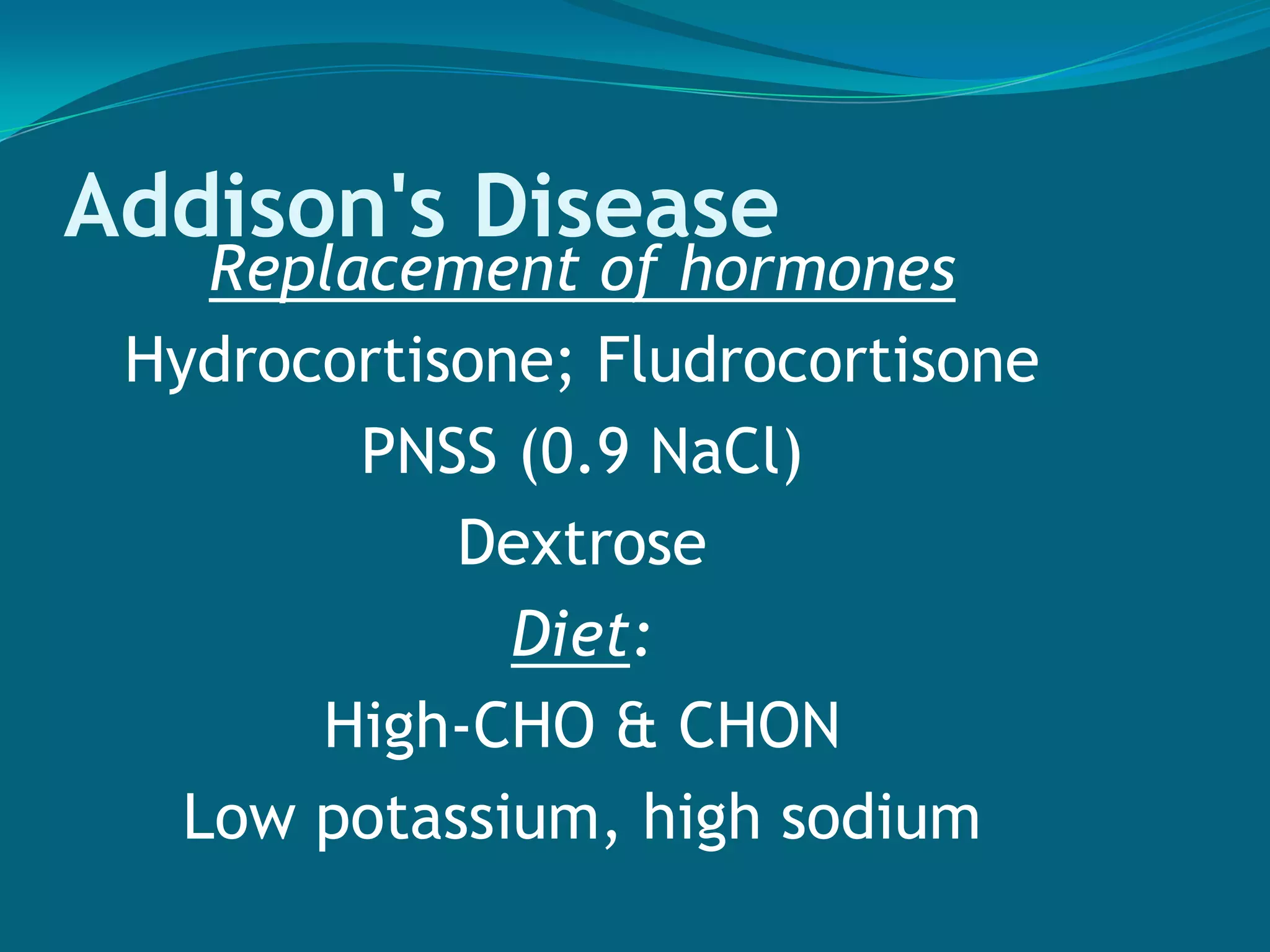
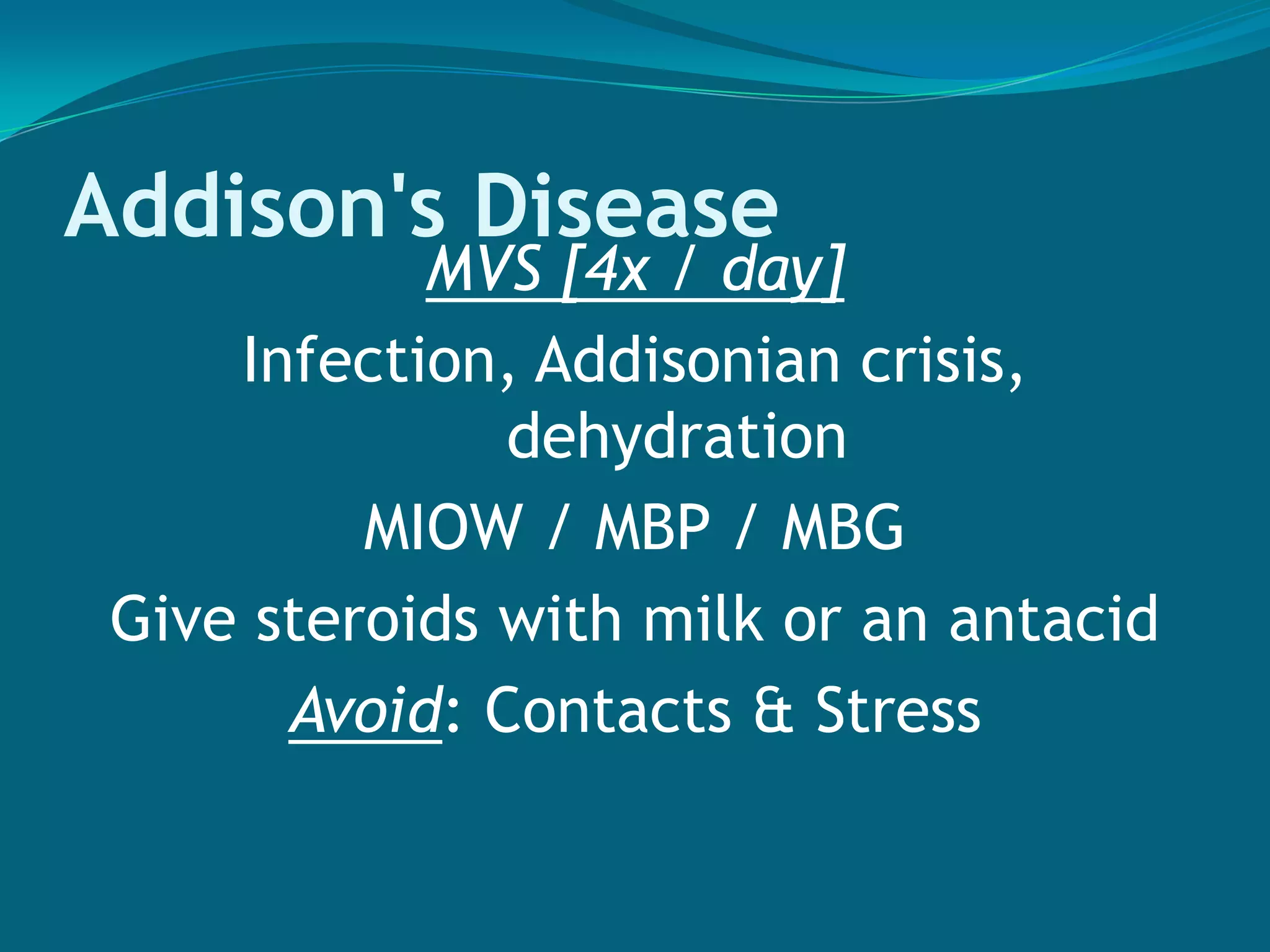
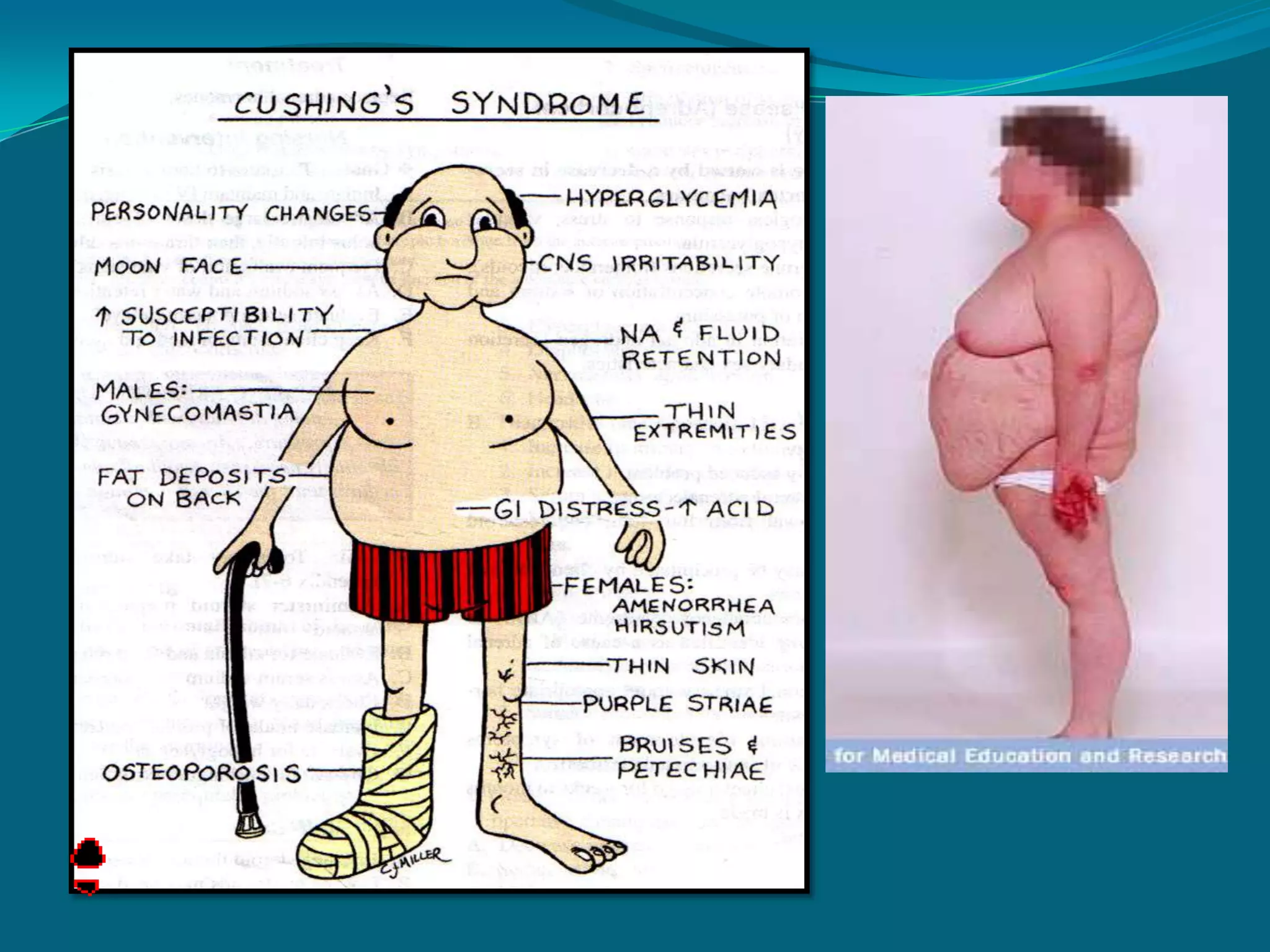
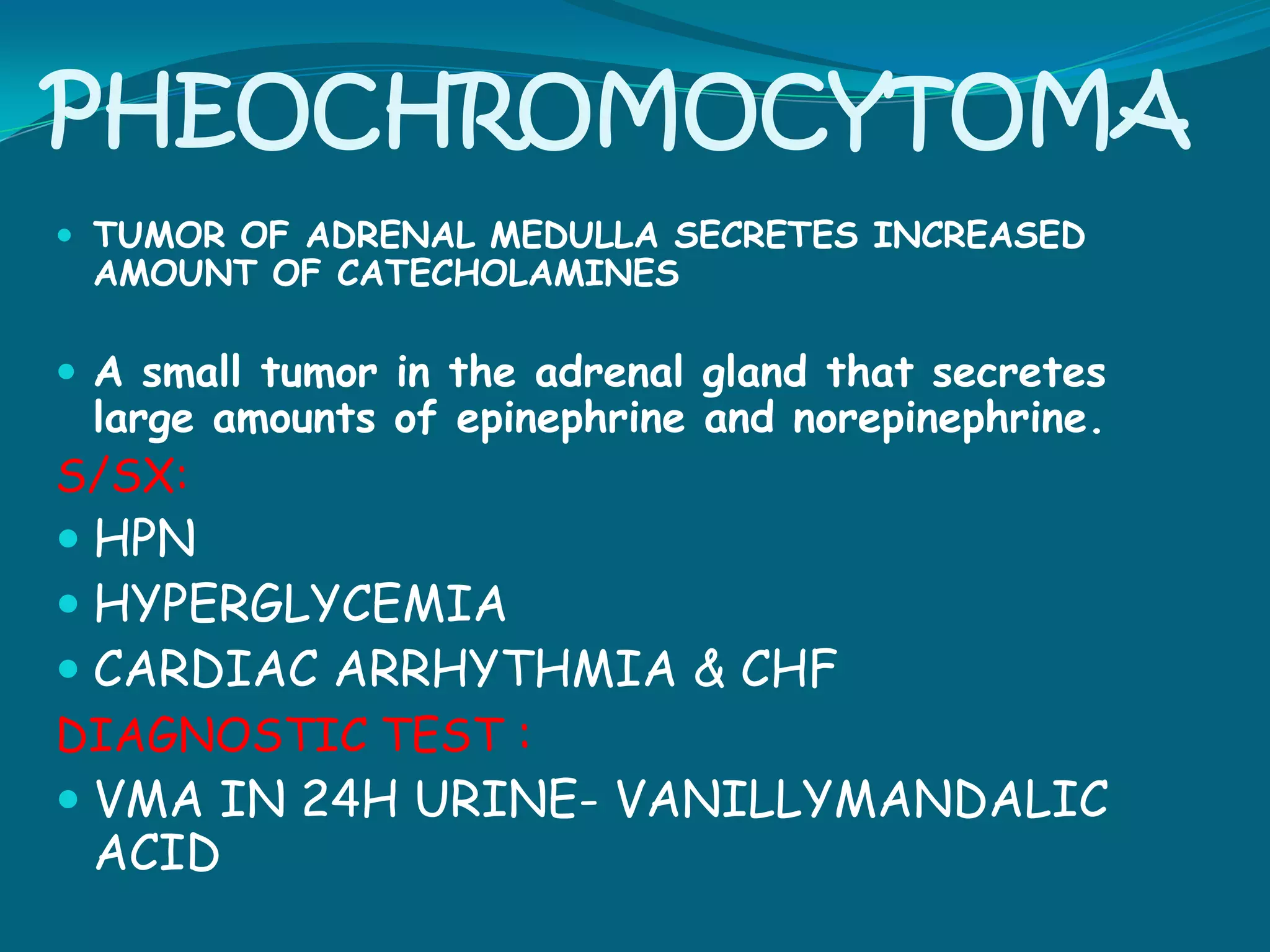
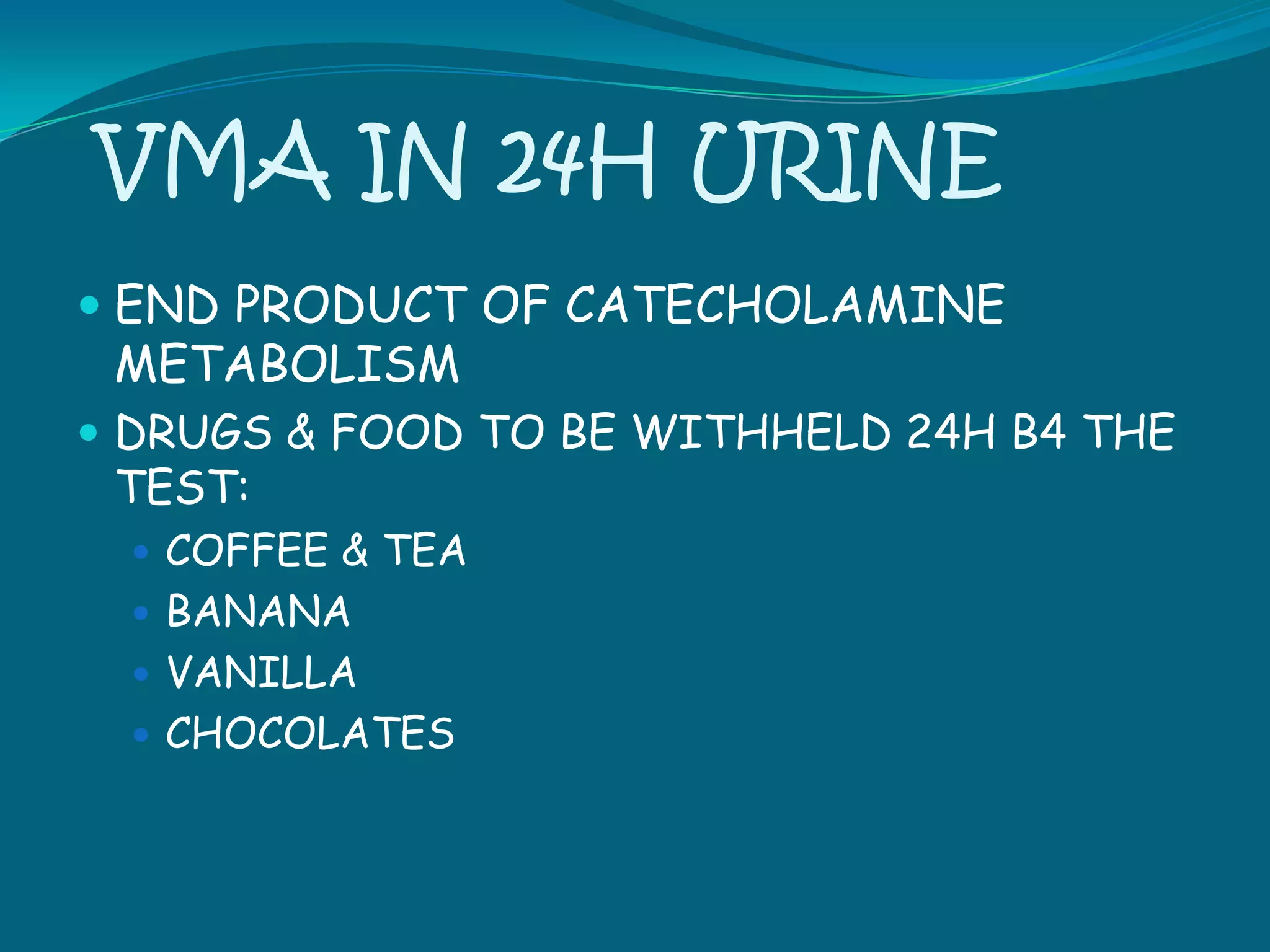
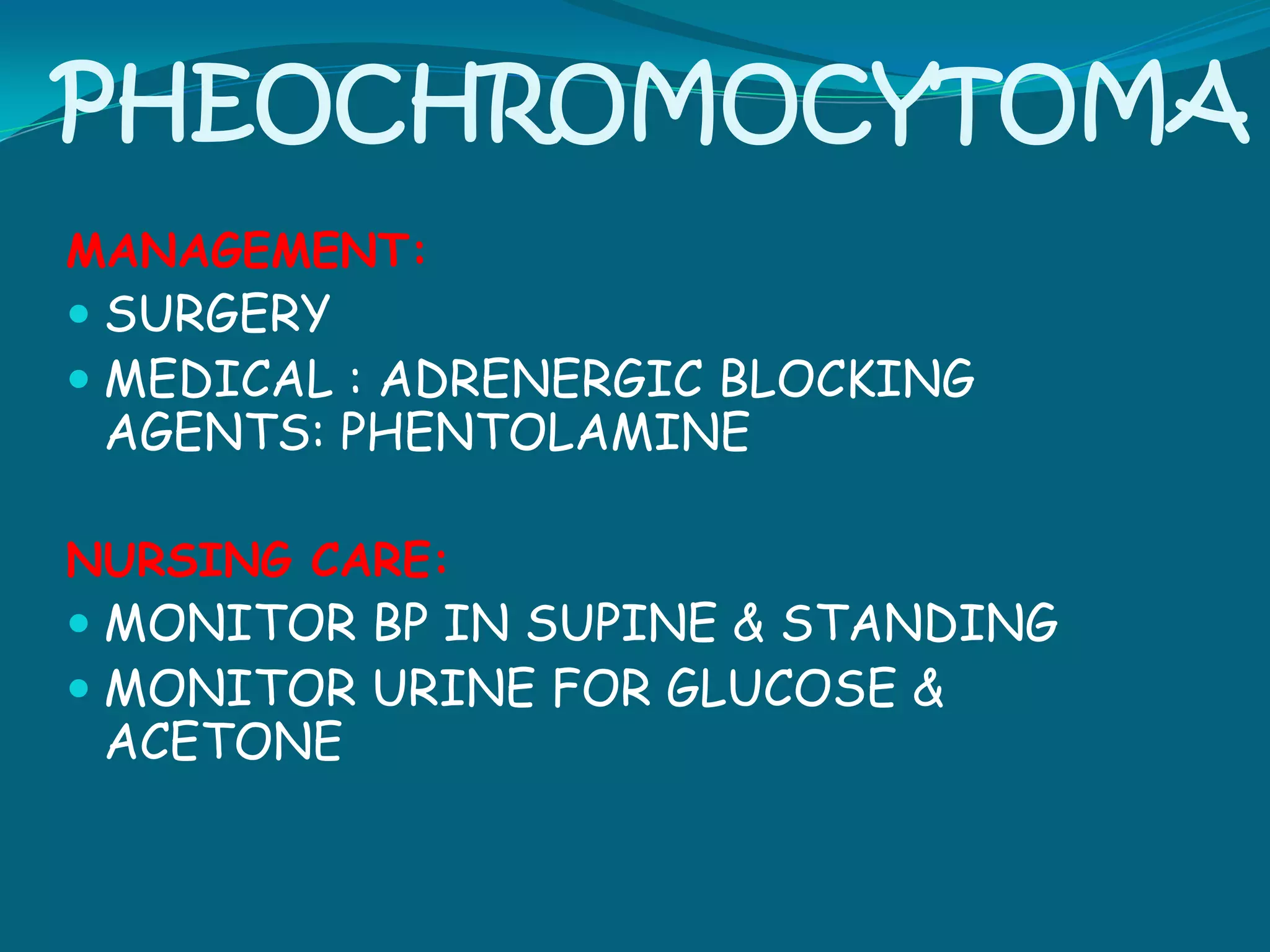
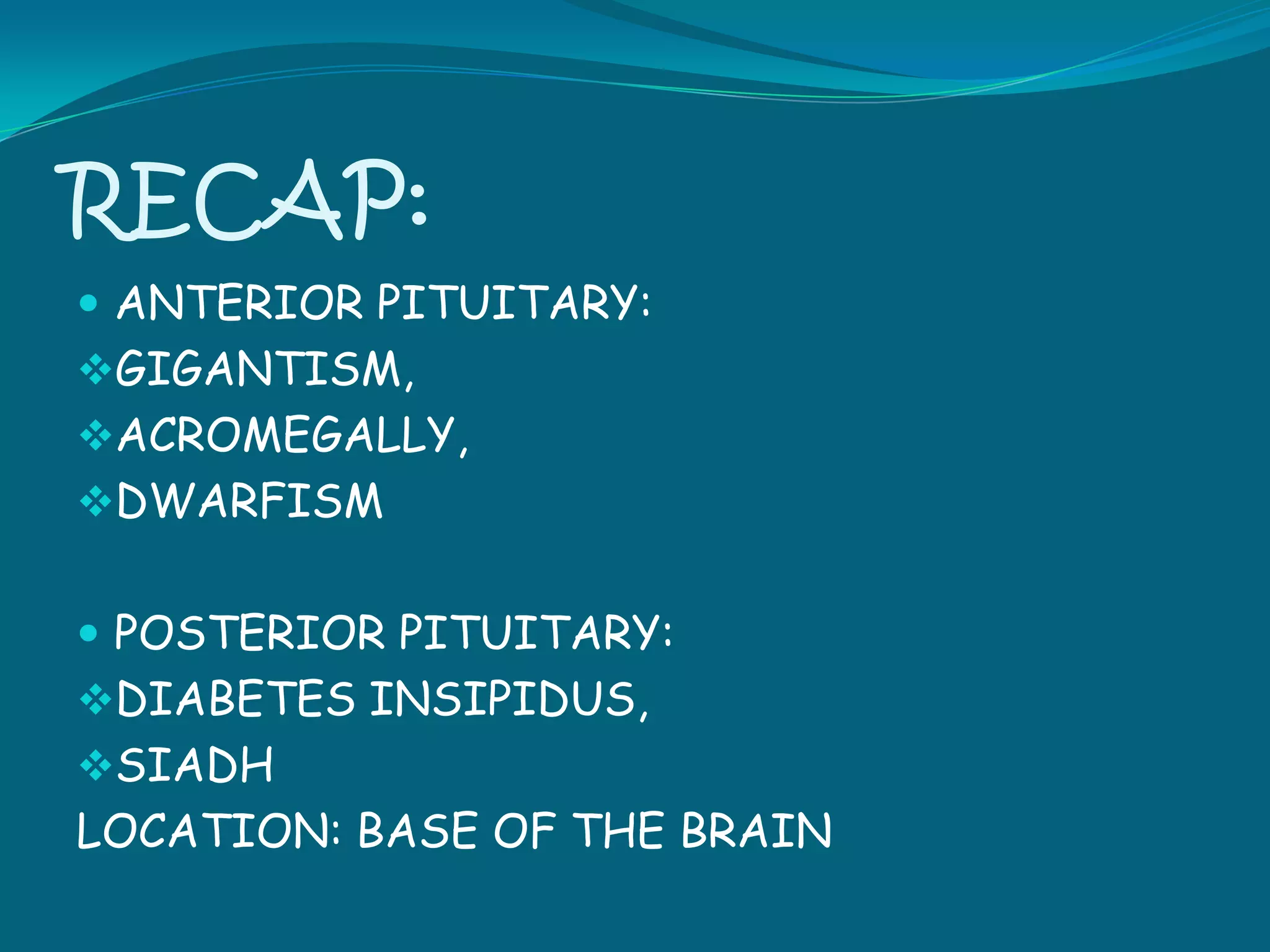
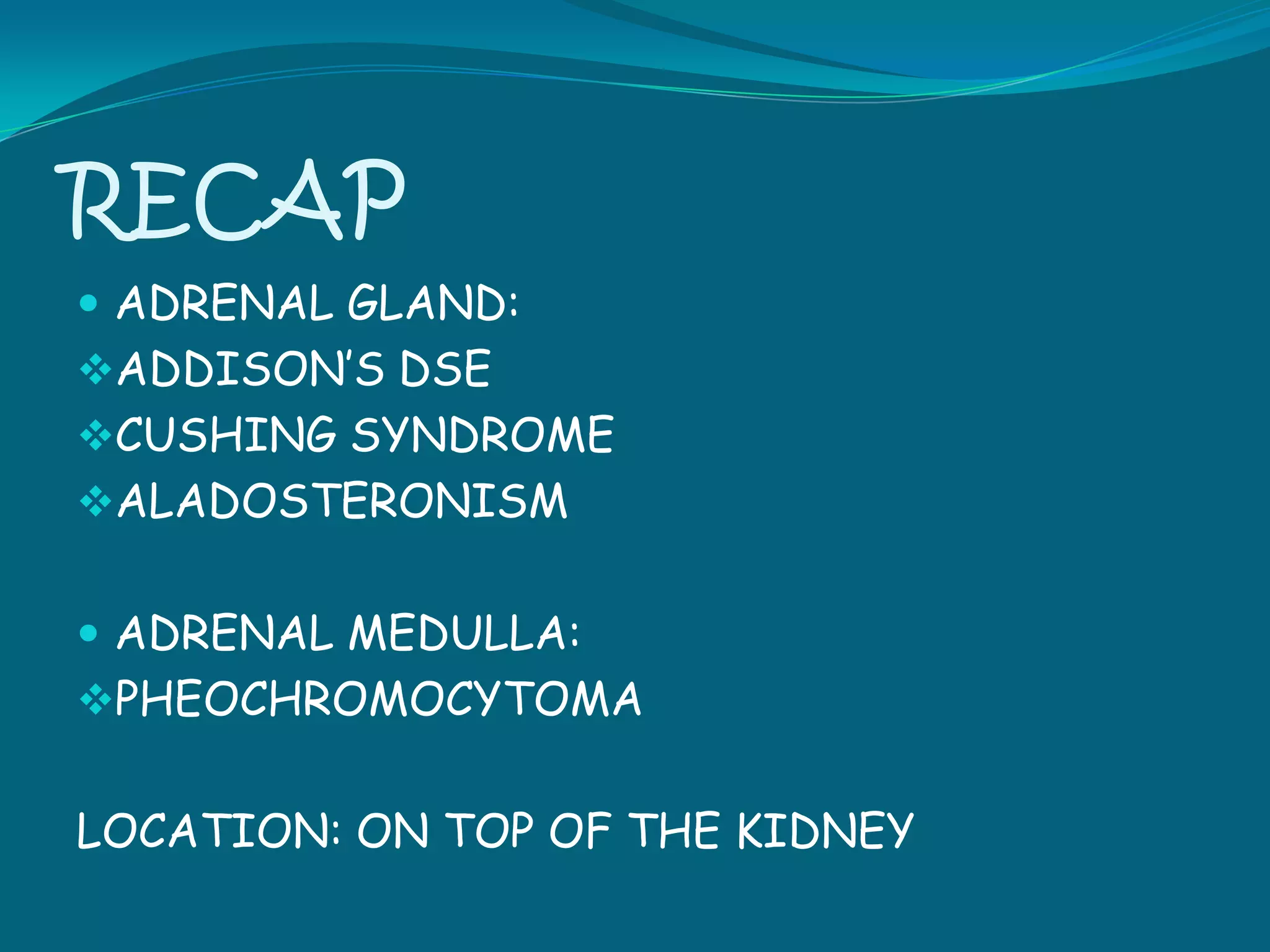
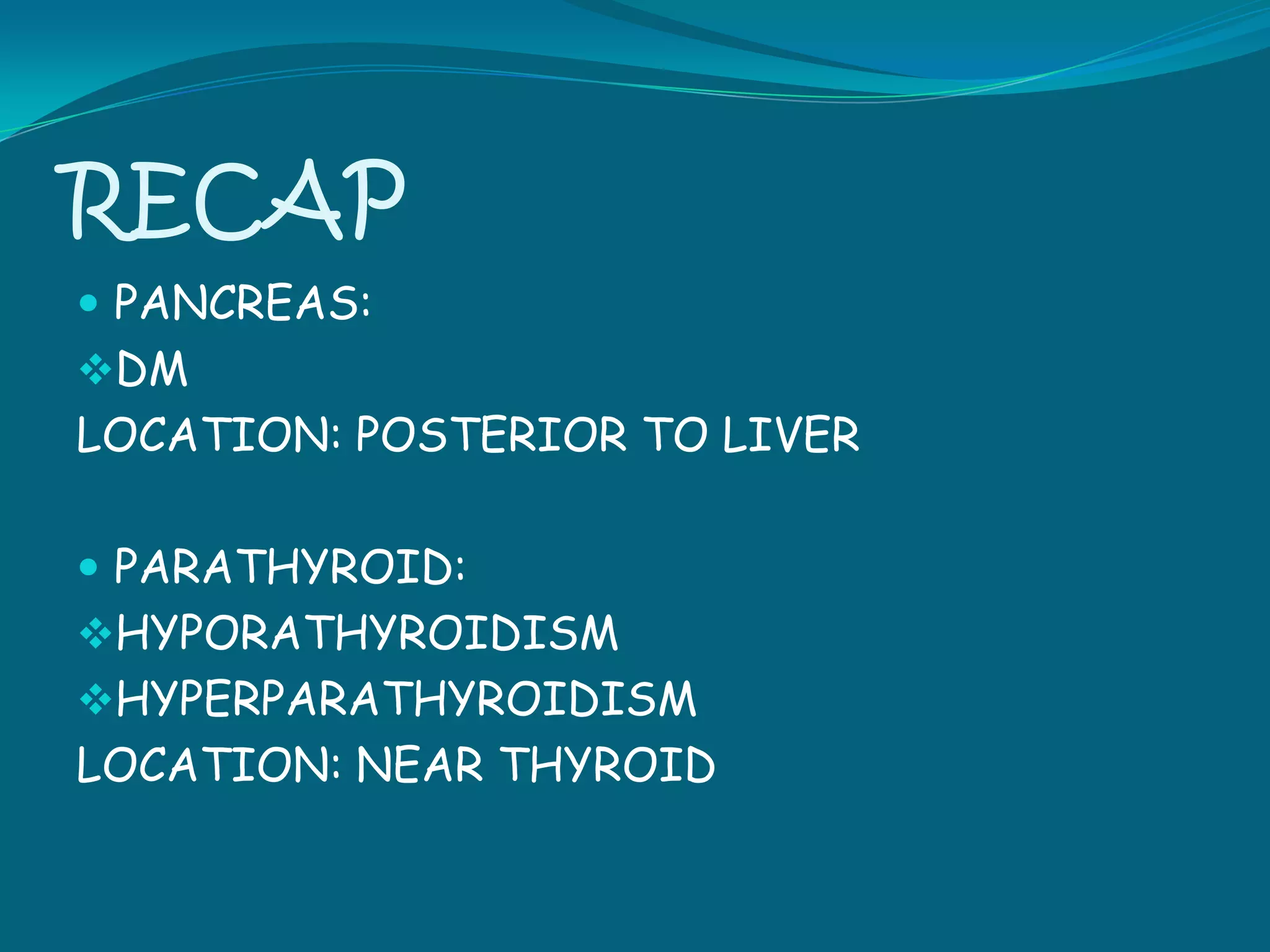
The endocrine system consists of glands that regulate metabolic processes through hormone secretion. Disorders can result from overactivity or underactivity of hormones. Common endocrine disorders include pituitary disorders like hyperpituitarism and hypopituitarism, thyroid disorders like hypothyroidism and hyperthyroidism, and parathyroid disorders like hypoparathyroidism. Symptoms depend on the hormone affected and include fatigue, weight changes, mood issues, and metabolic abnormalities. Treatment involves hormone replacement, medications, surgery, or lifestyle modifications. Nursing care focuses on monitoring for complications, providing support and education, and maintaining fluid and electrolyte balance.