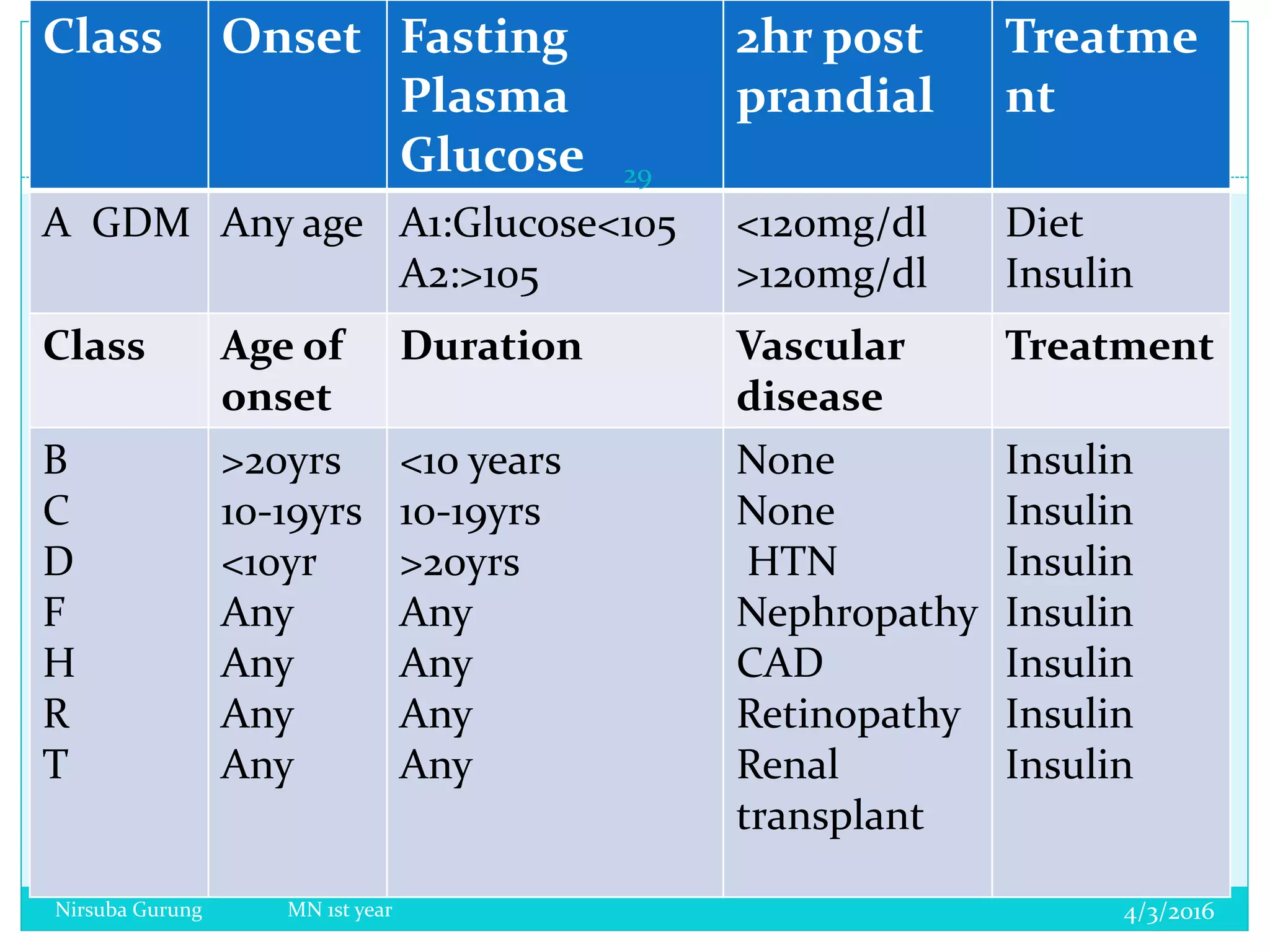
This document provides information on a presentation about diabetes in pregnancy. It begins with objectives of defining diabetes, explaining metabolic changes in pregnancy, classifying diabetes types in pregnancy, and outlining maternal and fetal risks and diagnosis/screening. It then covers topics like the definition of diabetes mellitus, gestational diabetes prevalence, carbohydrate and insulin metabolism changes, types of diabetes, maternal/fetal complications, diagnosis criteria, symptoms, and testing for gestational diabetes.