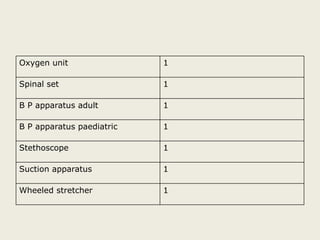
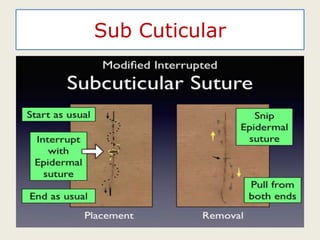
The document outlines essential considerations for operating theater (OT) design and operation including location, size, staffing, and waste management. It highlights parameters for ensuring efficiency and sterility, the roles of various staff, and classifications of surgical procedures. Additionally, the document details protocols for managing biomedical waste and the importance of maintaining aseptic techniques within the OT environment.