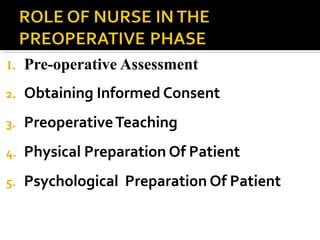
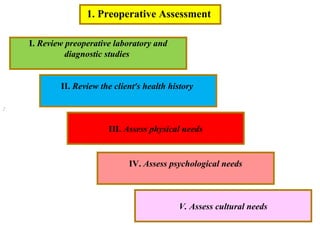
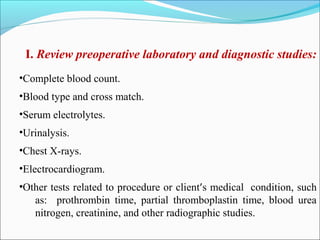
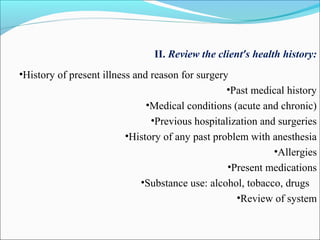
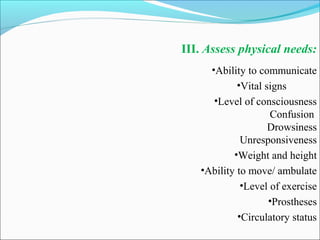
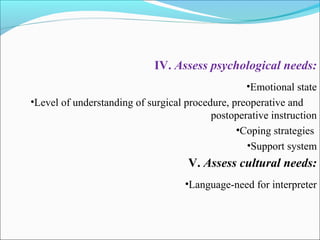
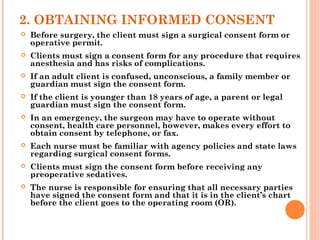
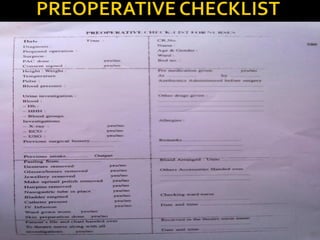
The document discusses pre-operative nursing care which includes: assessing the patient's health history and needs, obtaining informed consent, providing pre-operative teaching to the patient, and preparing the patient physically and psychologically for surgery. The pre-operative phase preparation involves ensuring adequate nutrition, elimination, hygiene, medications, sleep, storage of valuables, removal of prosthetics, following special orders, preparing the surgical site, safety protocols, monitoring vital signs, and applying anti-embolism stockings.