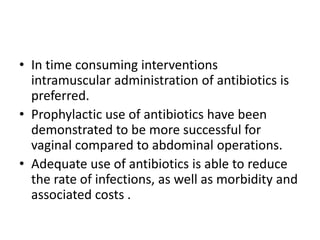
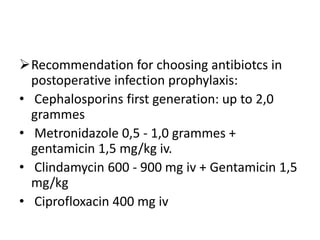
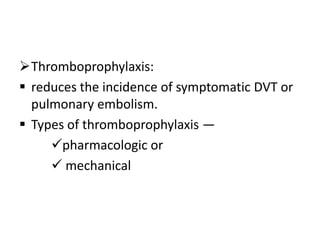
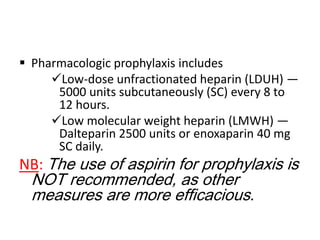
This document outlines preoperative care for gynecologic patients. It discusses preoperative evaluation including obtaining a comprehensive medical history, physical examination, anesthesiology examination, and necessary investigations. Preoperative preparation is also covered, such as correcting anemia, smoking cessation, medical consultation, bowel preparation, use of antibiotics and thromboprophylaxis. The goal of preoperative care is to avoid or minimize both intra- and postoperative complications and enable a successful surgical outcome.