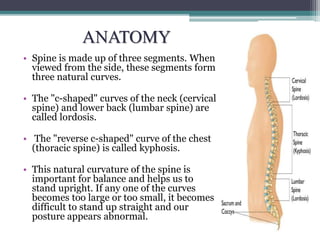
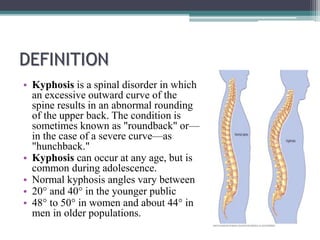
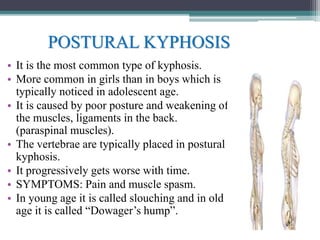
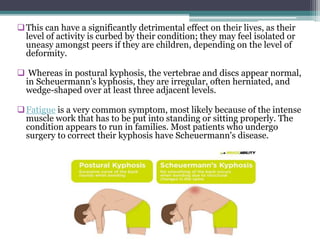
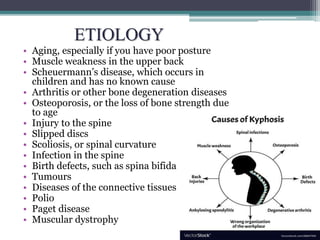
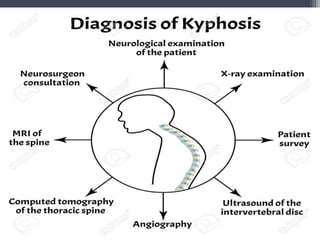
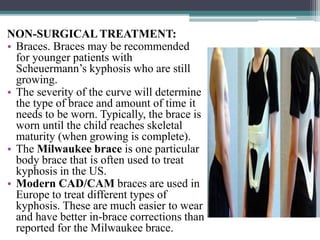
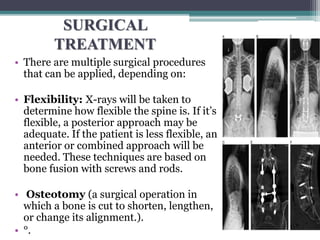
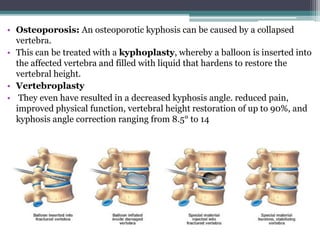
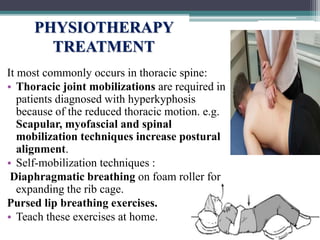
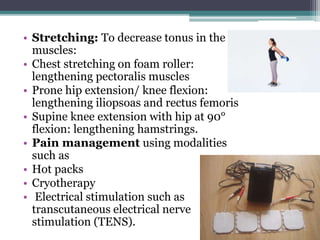
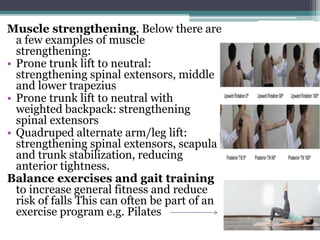
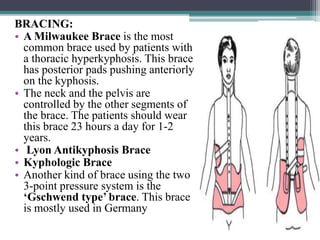
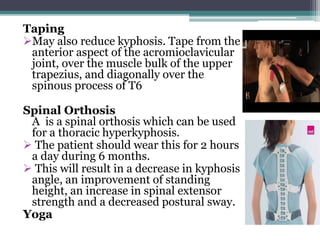
Kyphosis is an excessive outward curvature of the spine that results in an abnormal rounding of the upper back. There are several types of kyphosis, with the most common being postural kyphosis caused by poor posture and weak back muscles. Symptoms may include back pain and muscle spasms. Treatment options include exercises to improve posture and strengthen back muscles, bracing, and in severe cases, surgery to correct the spinal curvature. Physiotherapy focuses on stretching tight muscles and strengthening weak back muscles to improve posture and reduce pain.