The document discusses the Pap smear test, including its history, procedure, interpretation, and management of abnormal results. It was developed by Dr. Arivendran to provide guidance on Pap smears. Key points include:
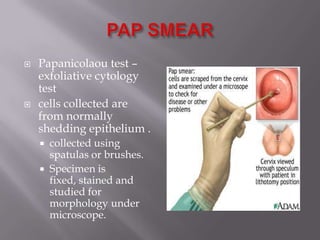
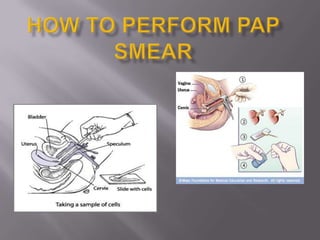
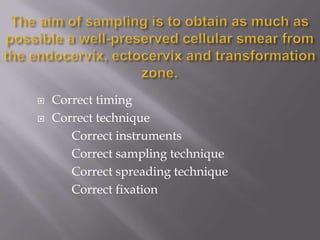
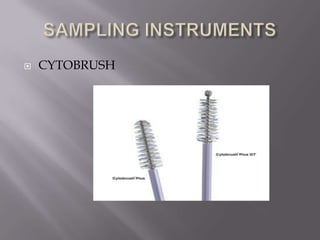
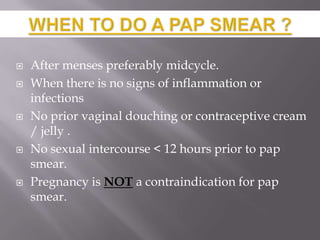
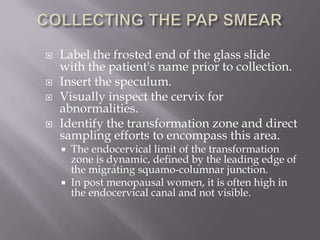
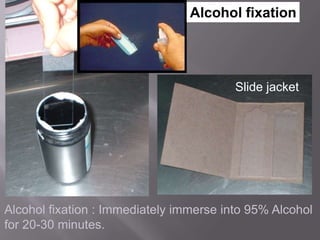
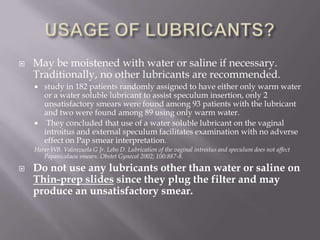
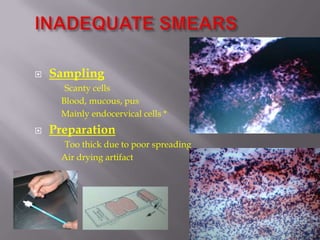
- The Pap test involves collecting cells from the cervix and vagina using spatulas or brushes, fixing and staining the cells, and examining them microscopically.
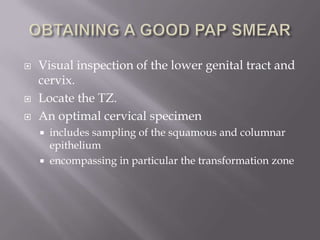
- An optimal sample includes cells from the transformation zone where most cervical abnormalities occur.
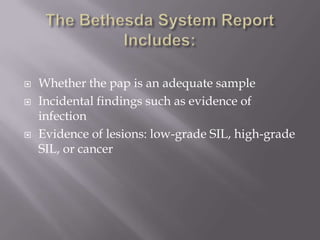
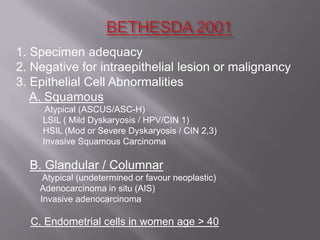
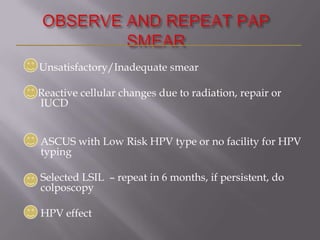
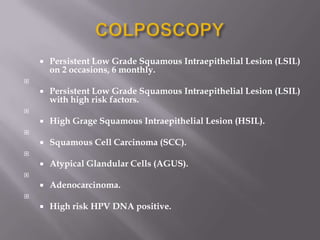
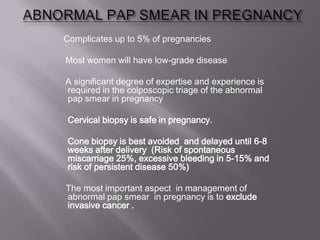
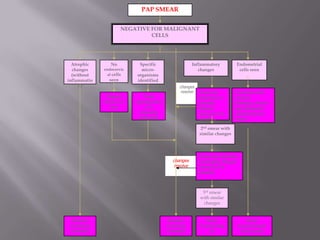
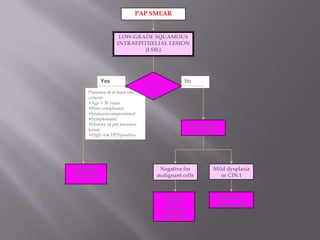
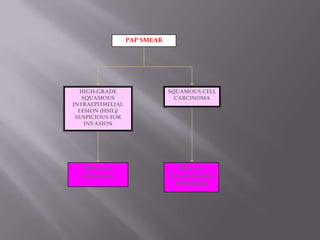
- Abnormal results are categorized using the Bethesda system and may indicate infection, inflammation, dysplasia or cancer.
- Management depends on the abnormality but may include treatment, repeated testing, or colpos