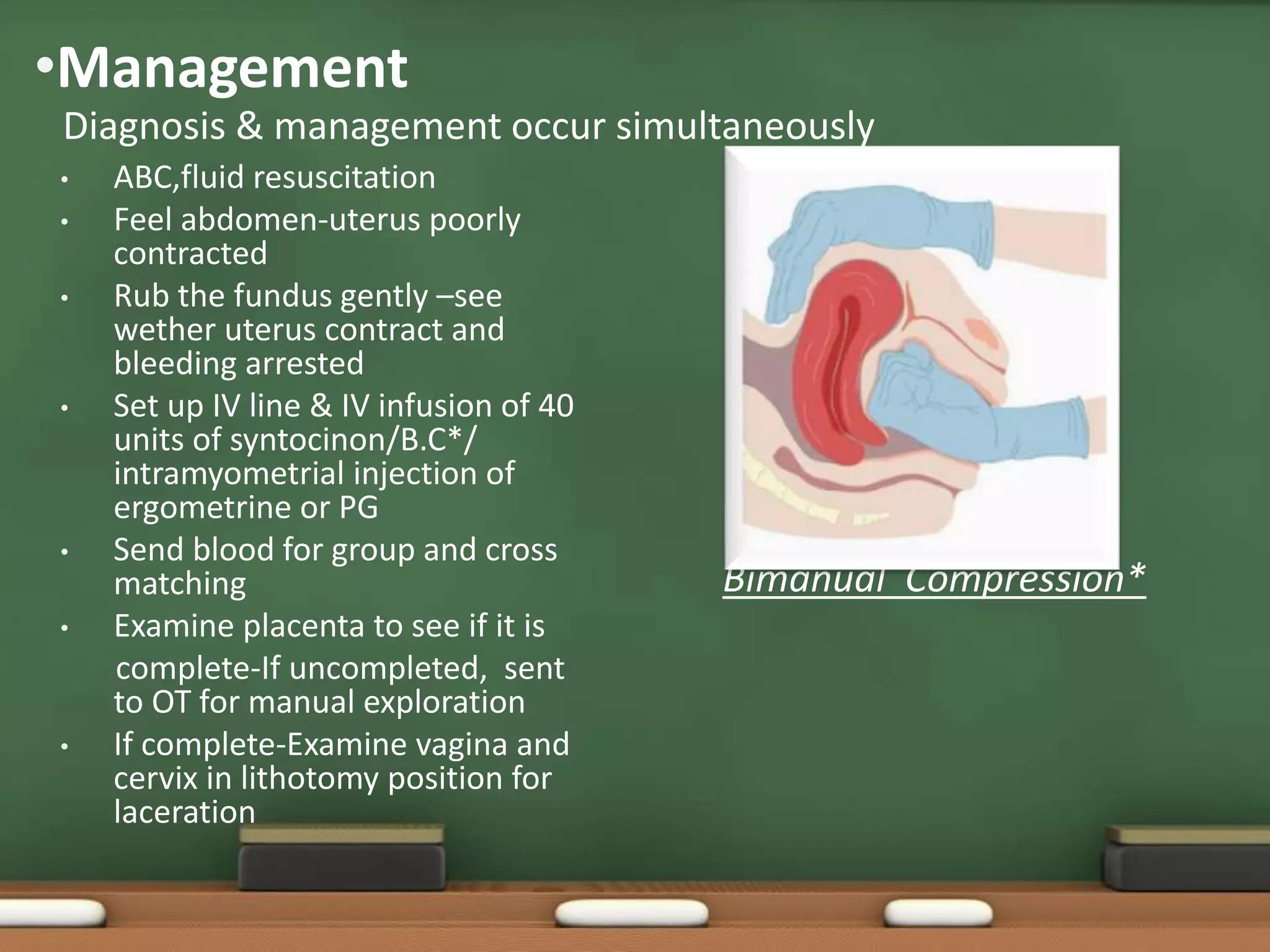
This document defines and describes postpartum haemorrhage (PPH). PPH is classified as primary (occurring within 24 hours of delivery) or secondary (occurring between 24 hours and 12 weeks post delivery). The main causes of PPH are uterine atony, retained placenta, genital tract lacerations, coagulation disorders, and acute inversion of the uterus. Risk factors include multiparity, overdistension of the uterus, prolonged labour, and uterine fibroids. Management involves ABCs, fluid resuscitation, uterotonic drugs, bimanual compression, exploration for retained tissue, and in severe cases surgical interventions like hysterectomy. Secondary PPH is usually caused by retained products of conception or