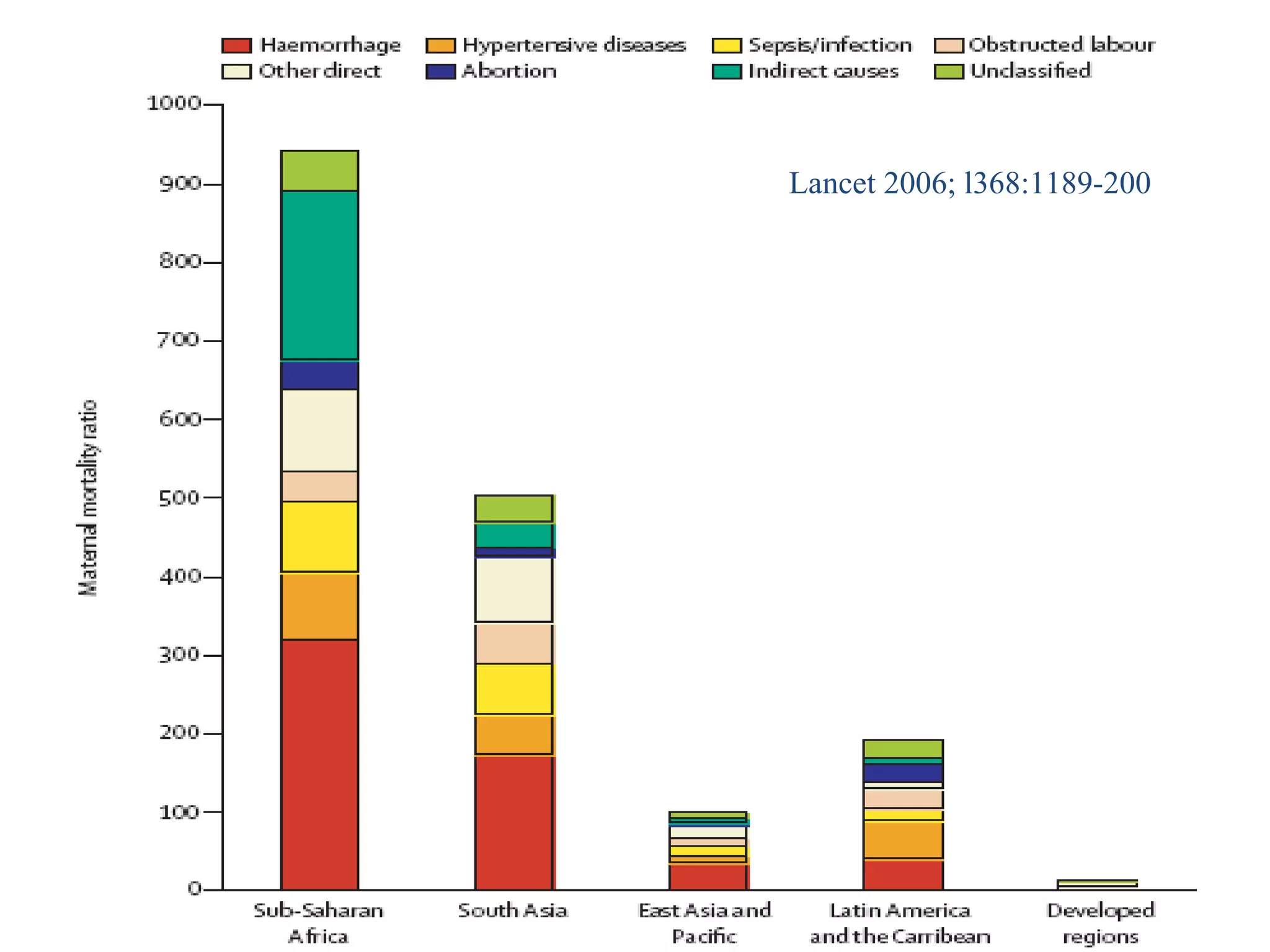
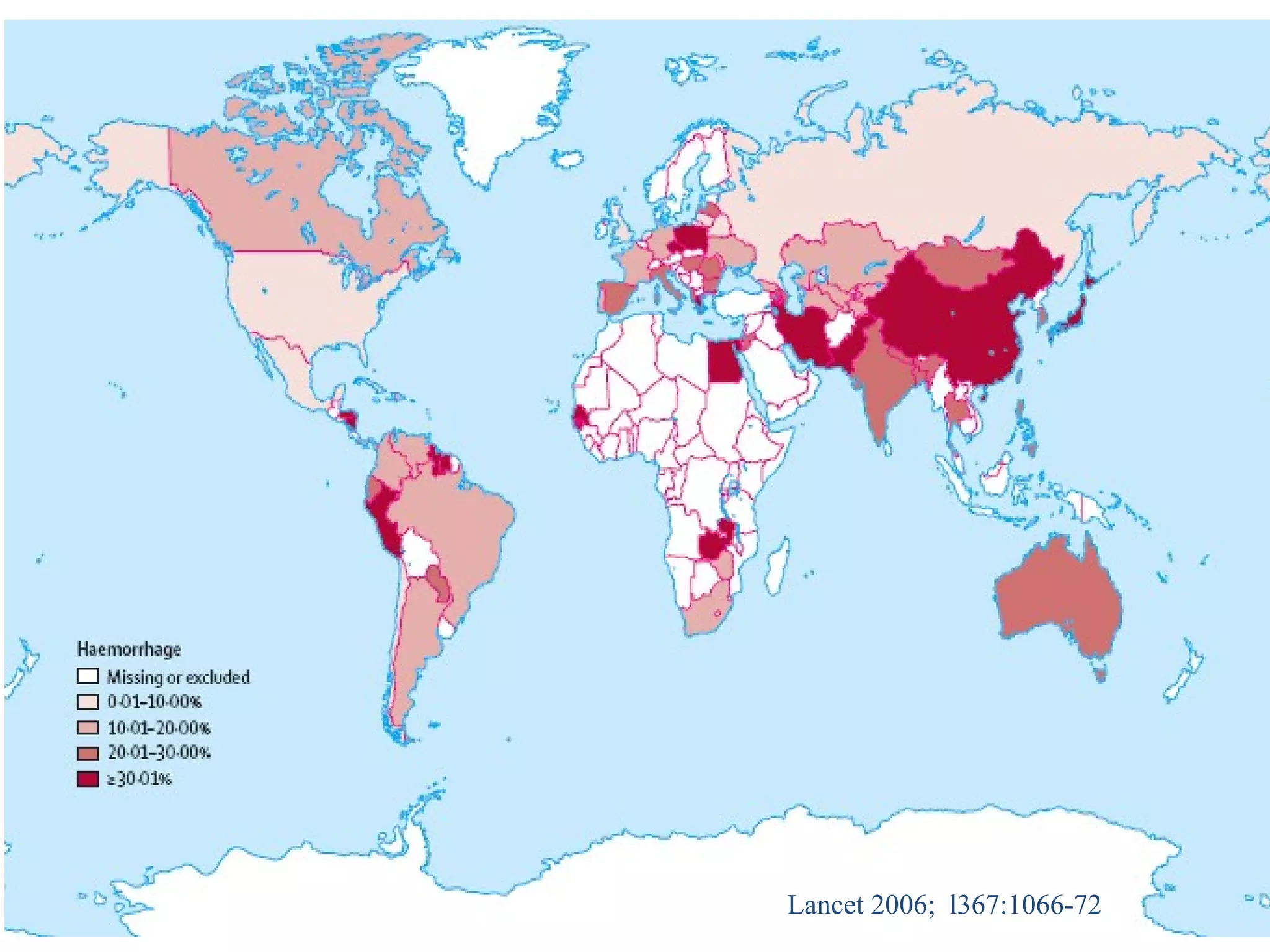
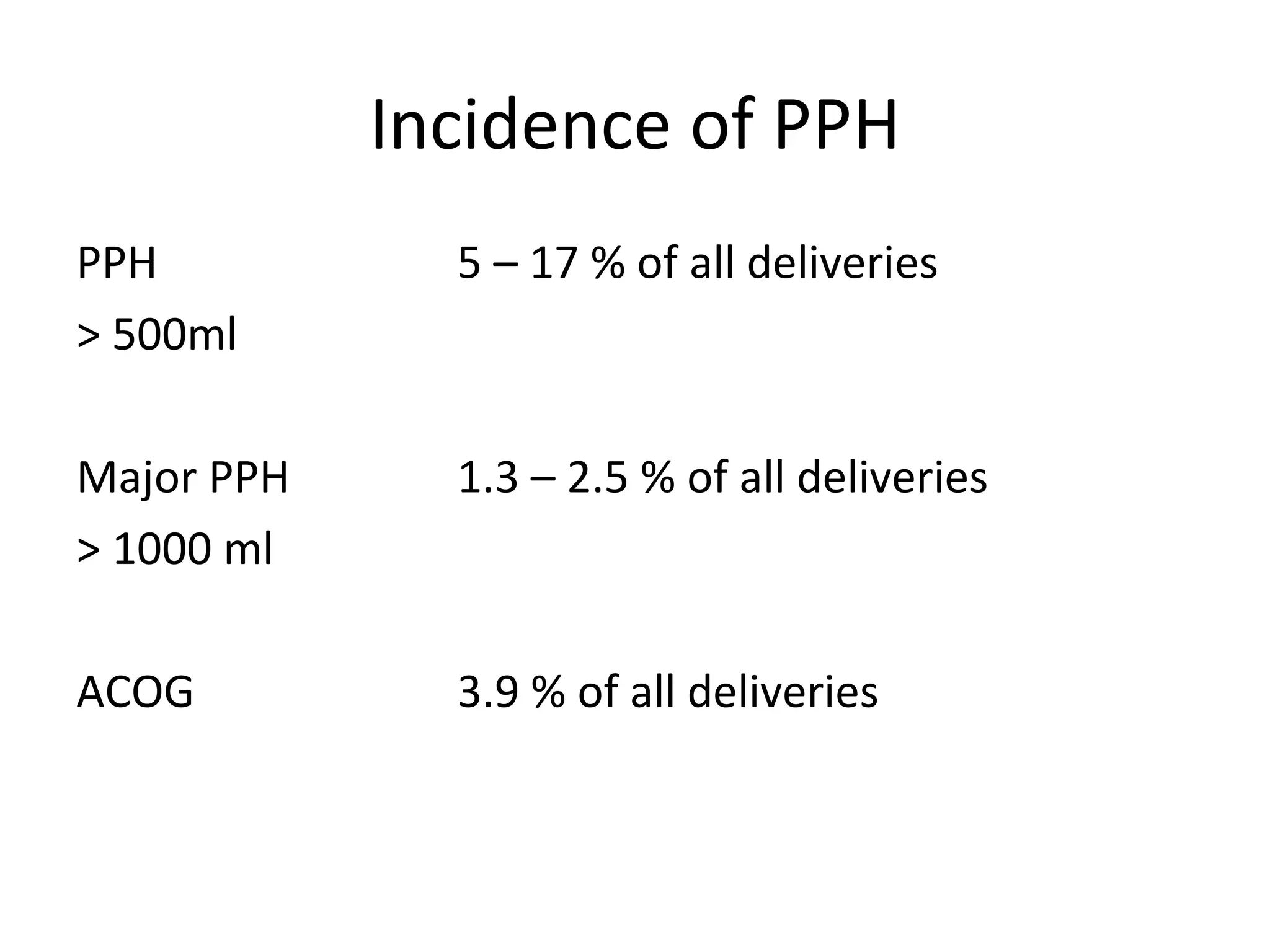
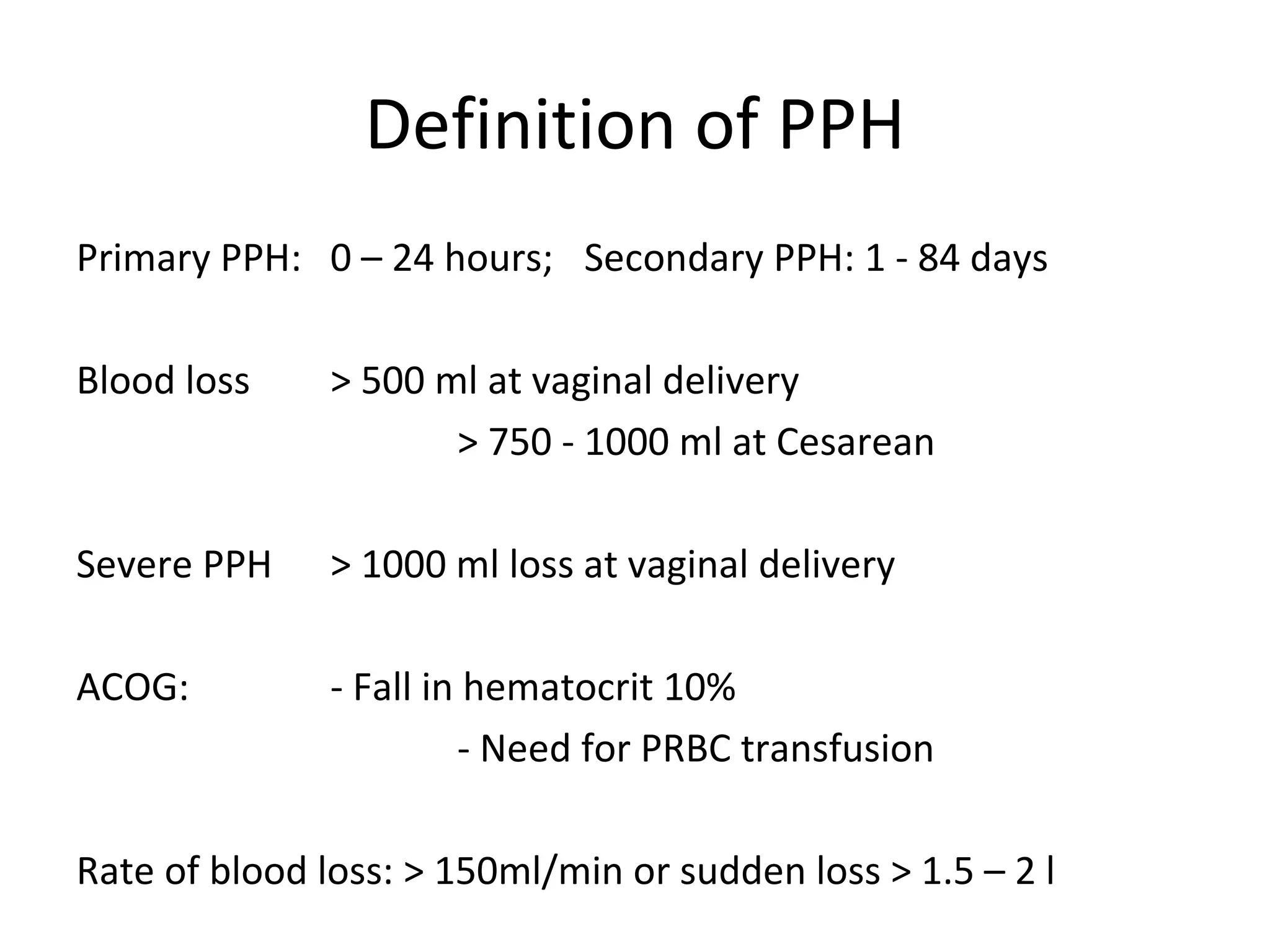
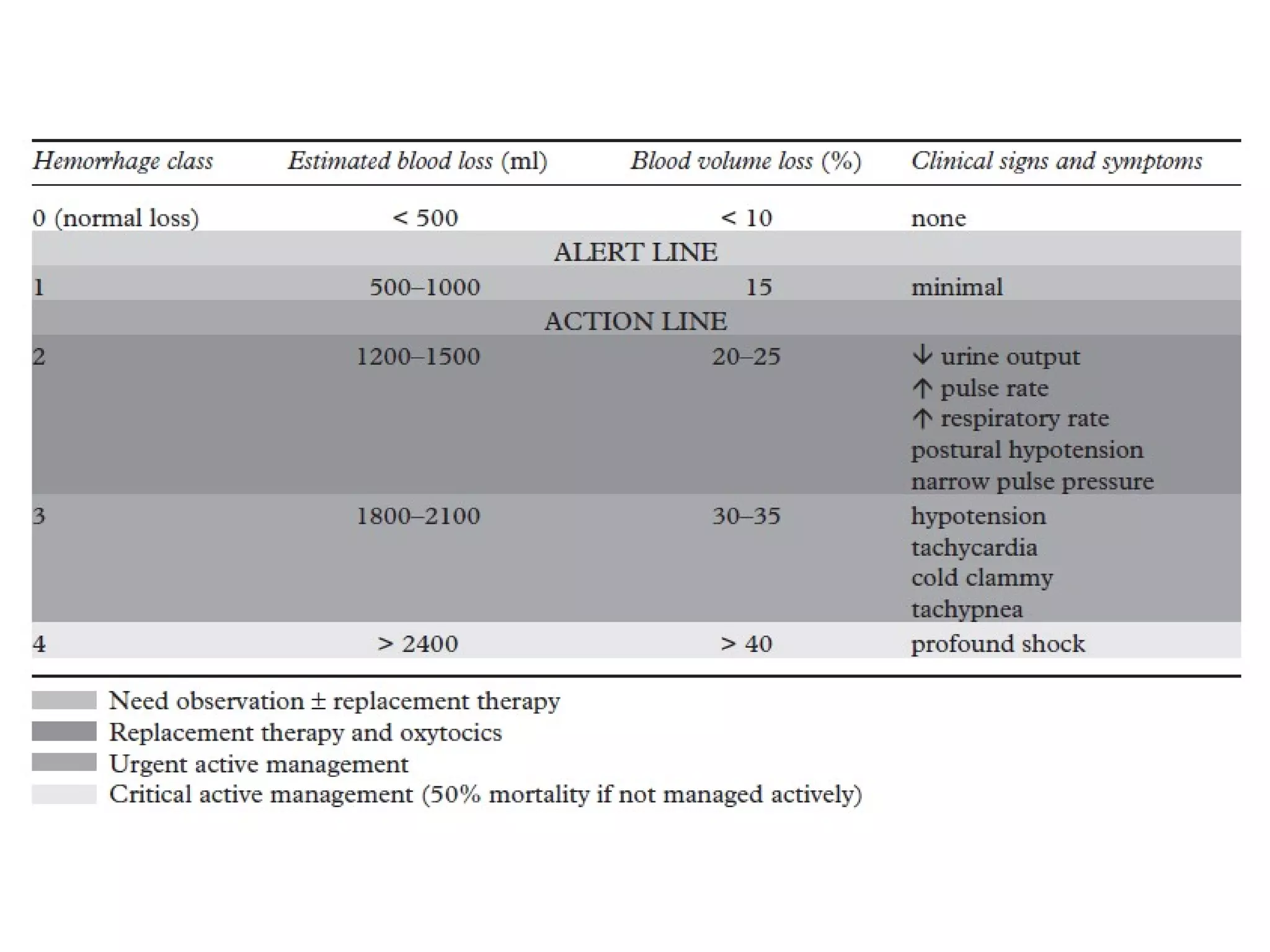
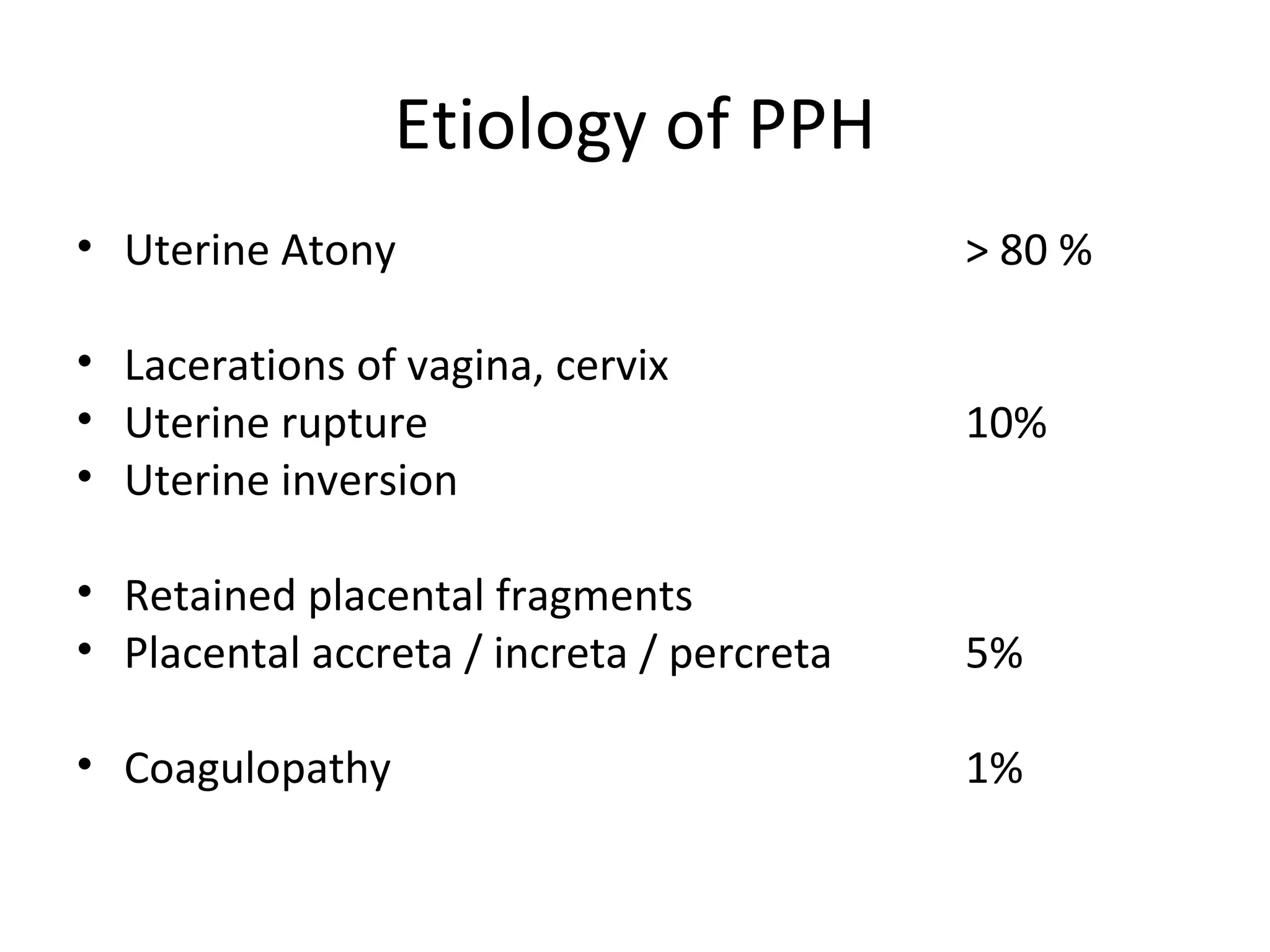
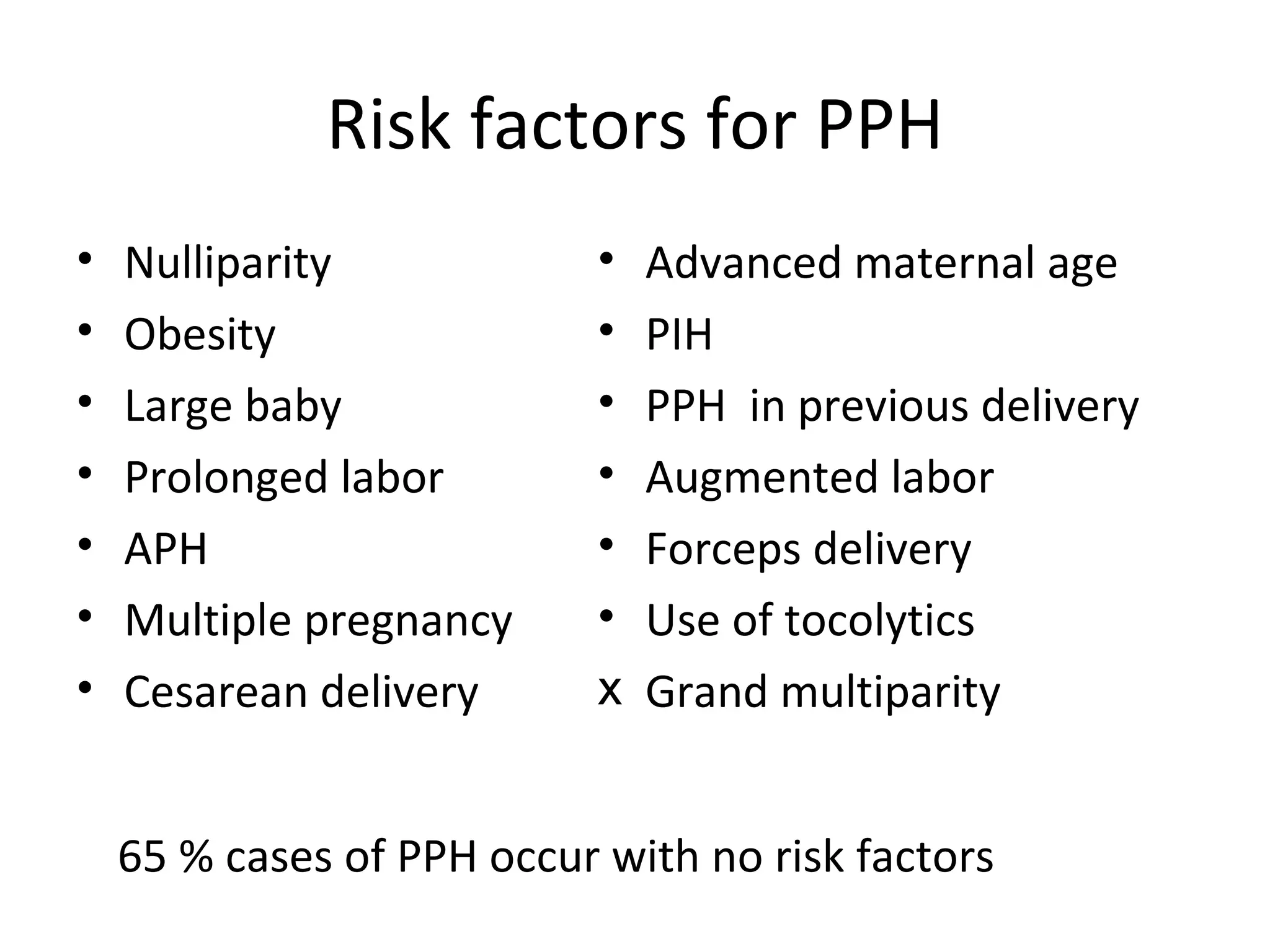
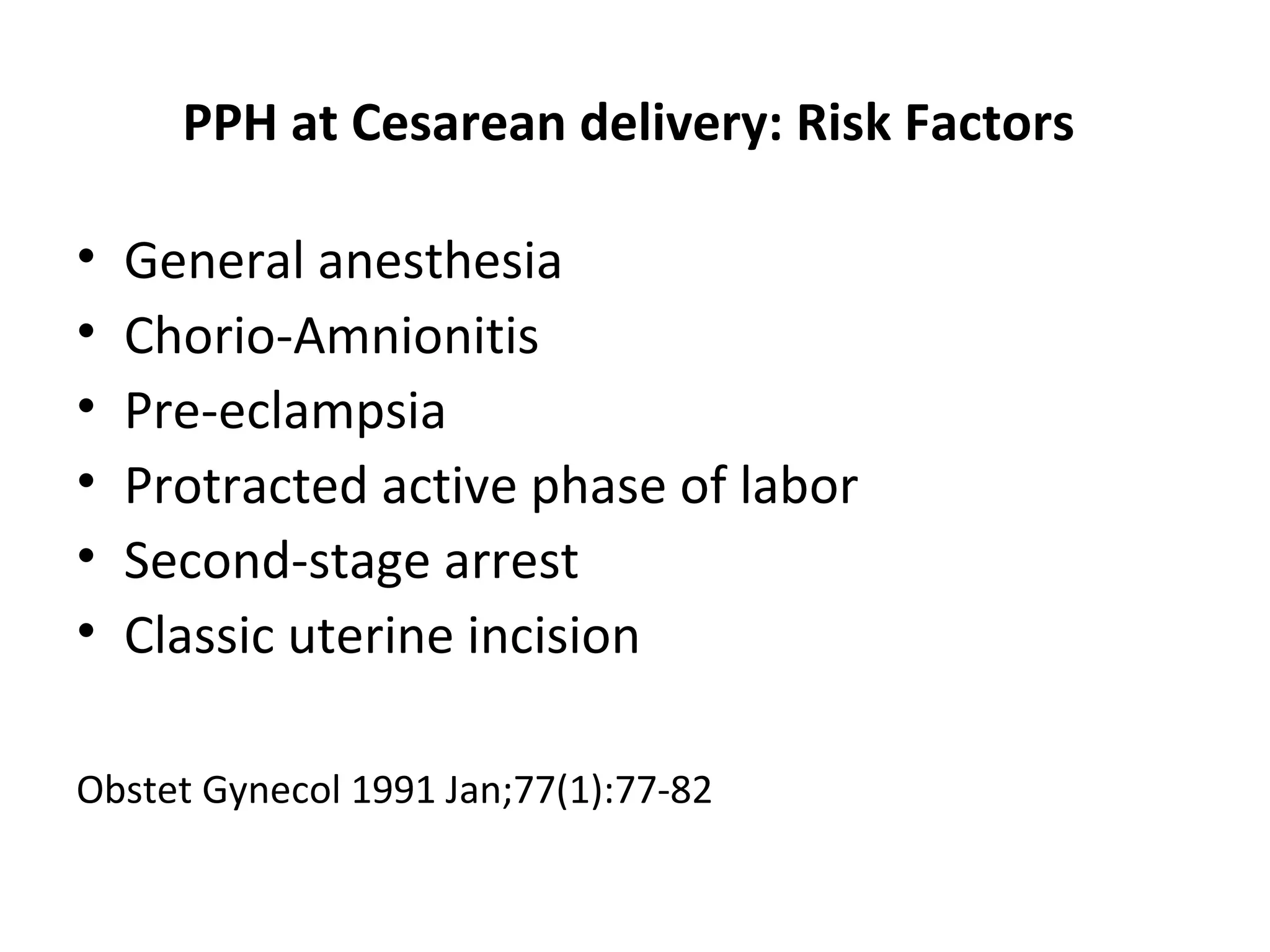
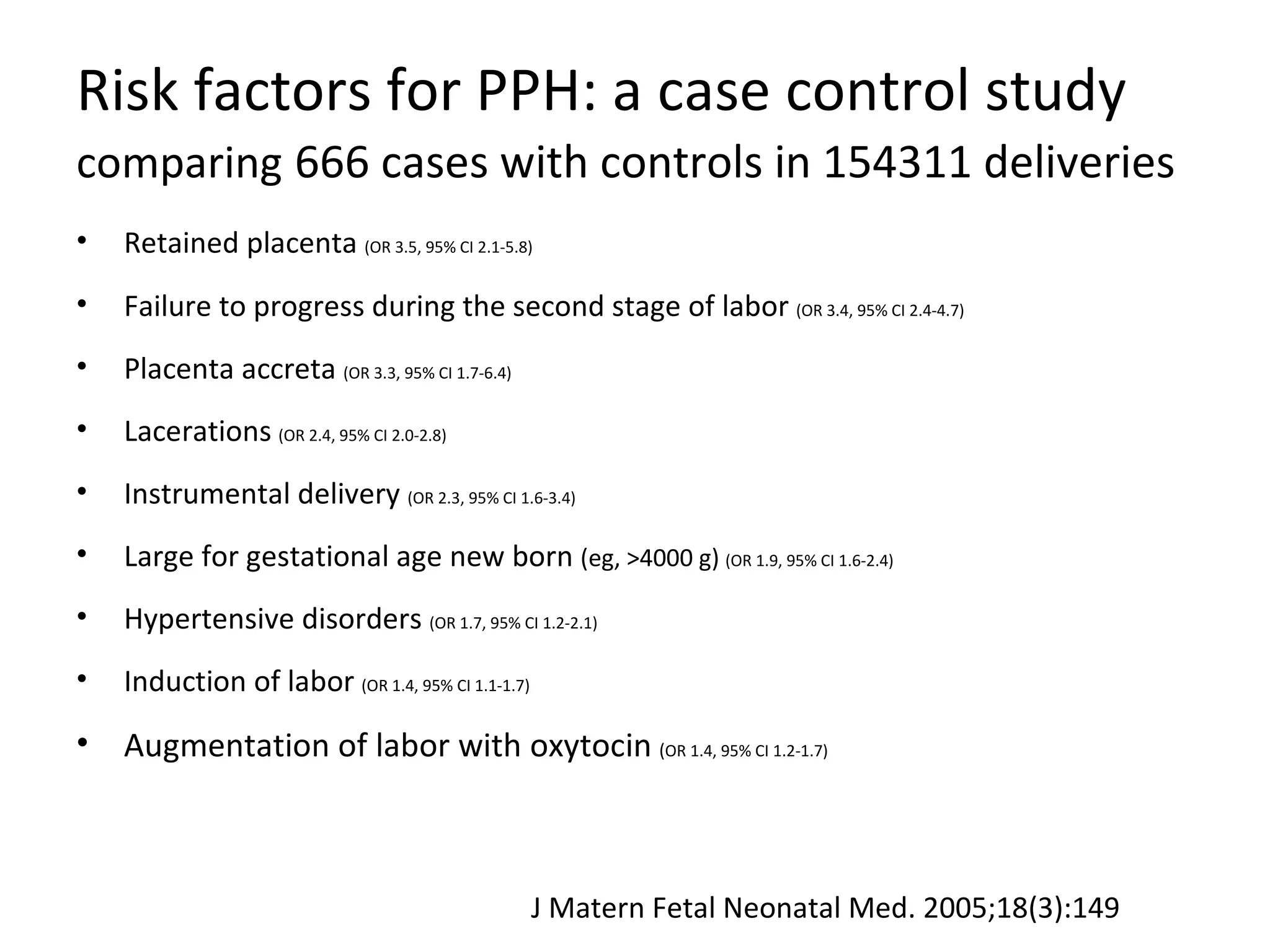
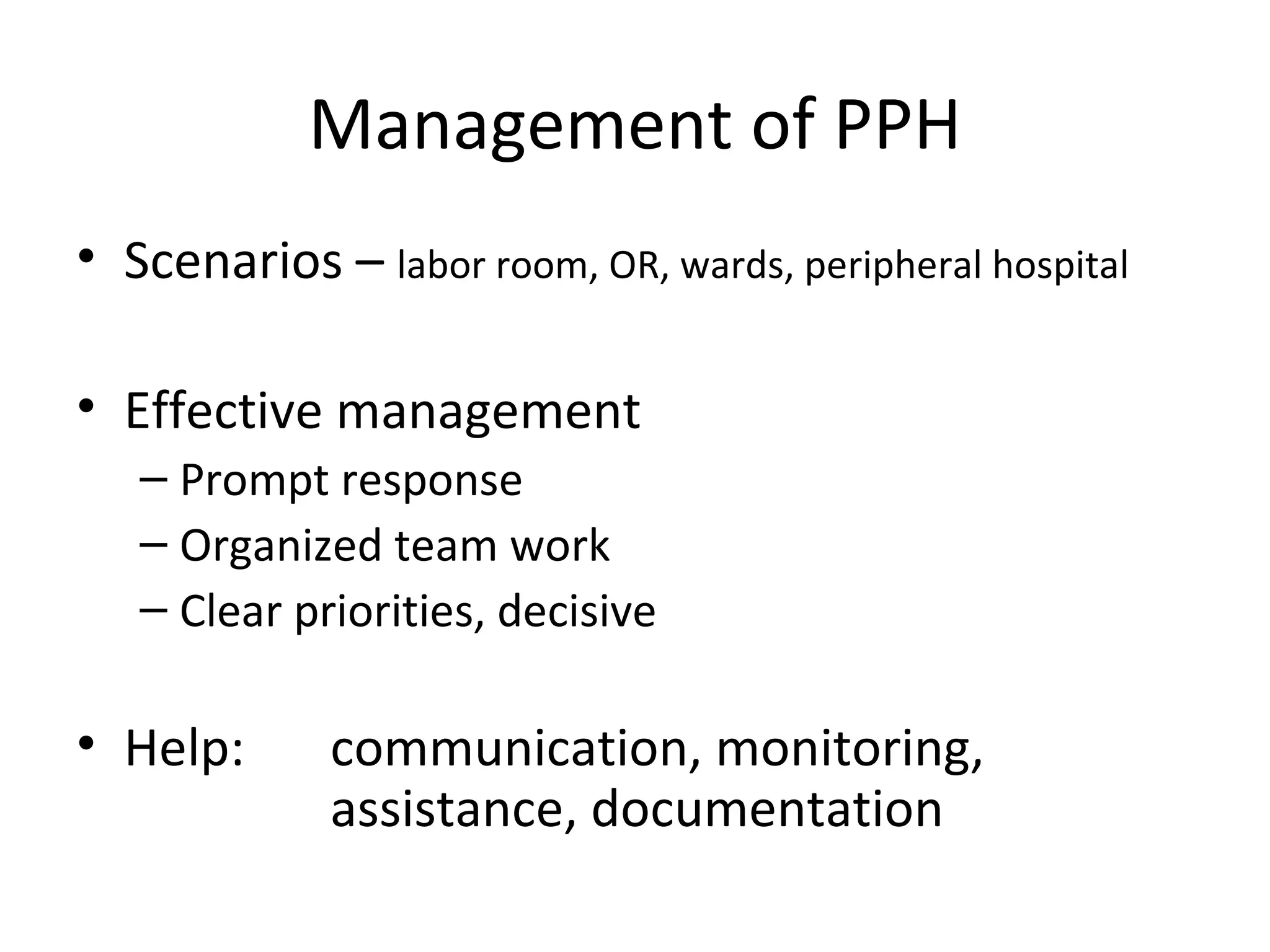
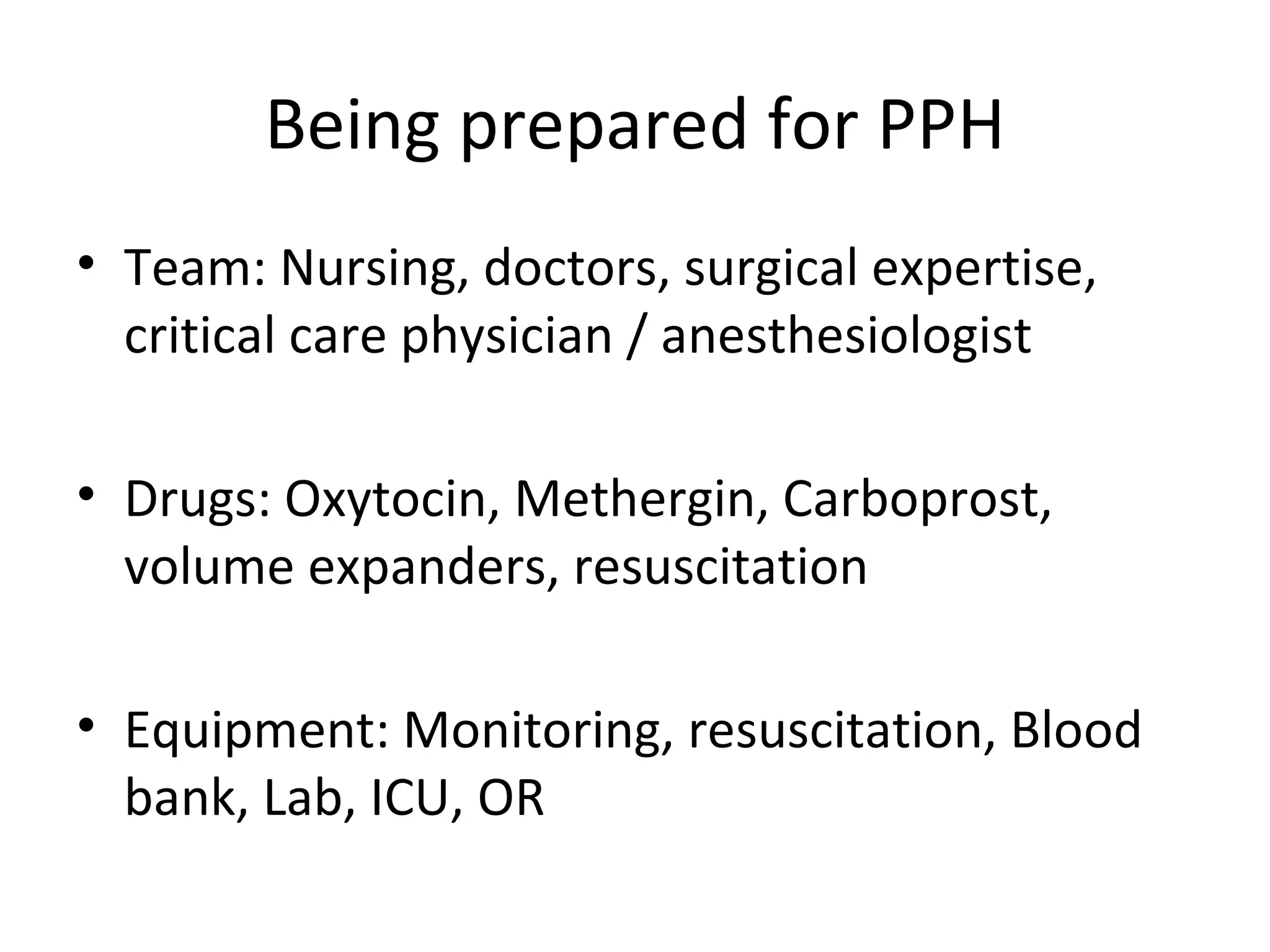
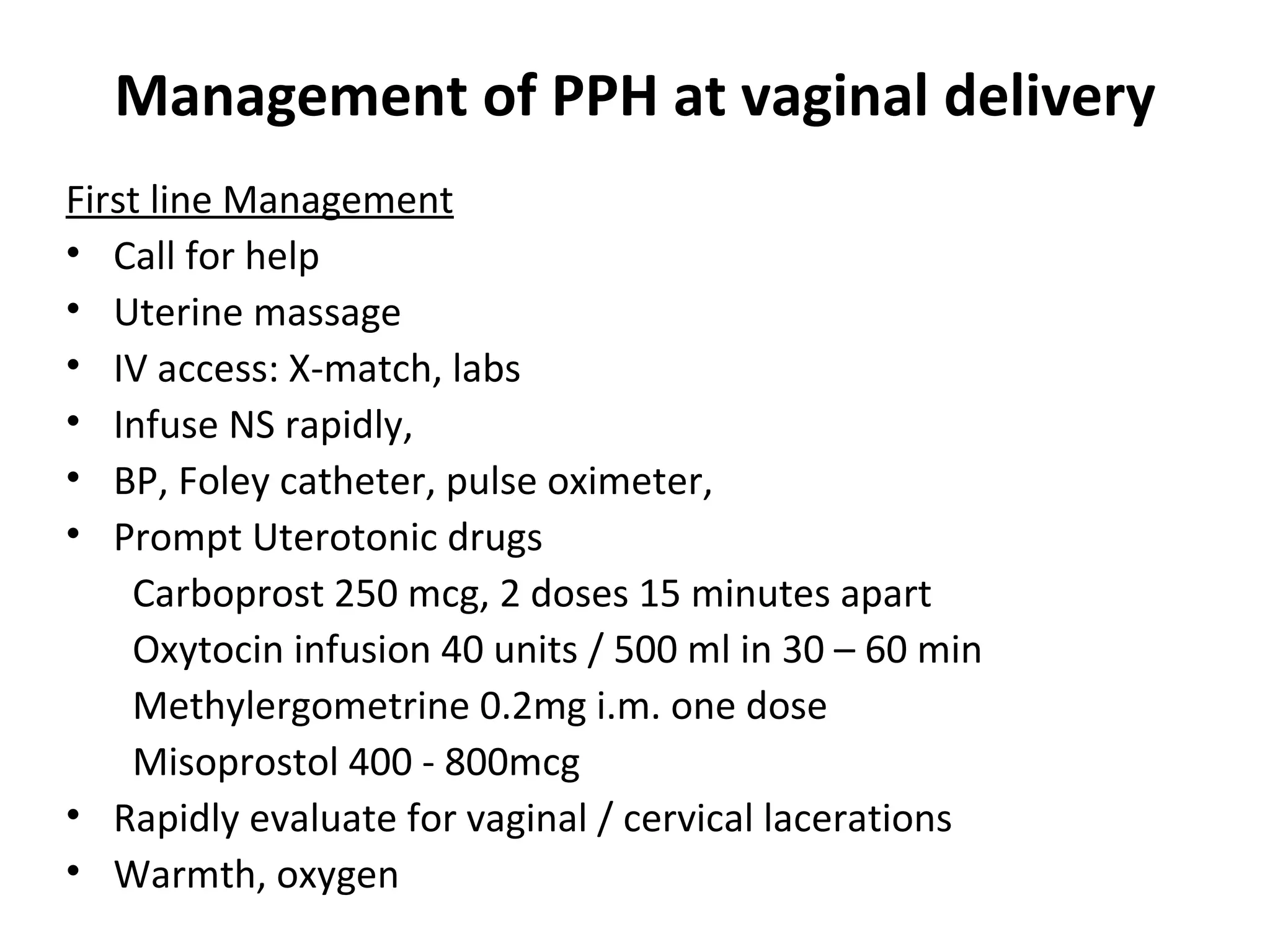
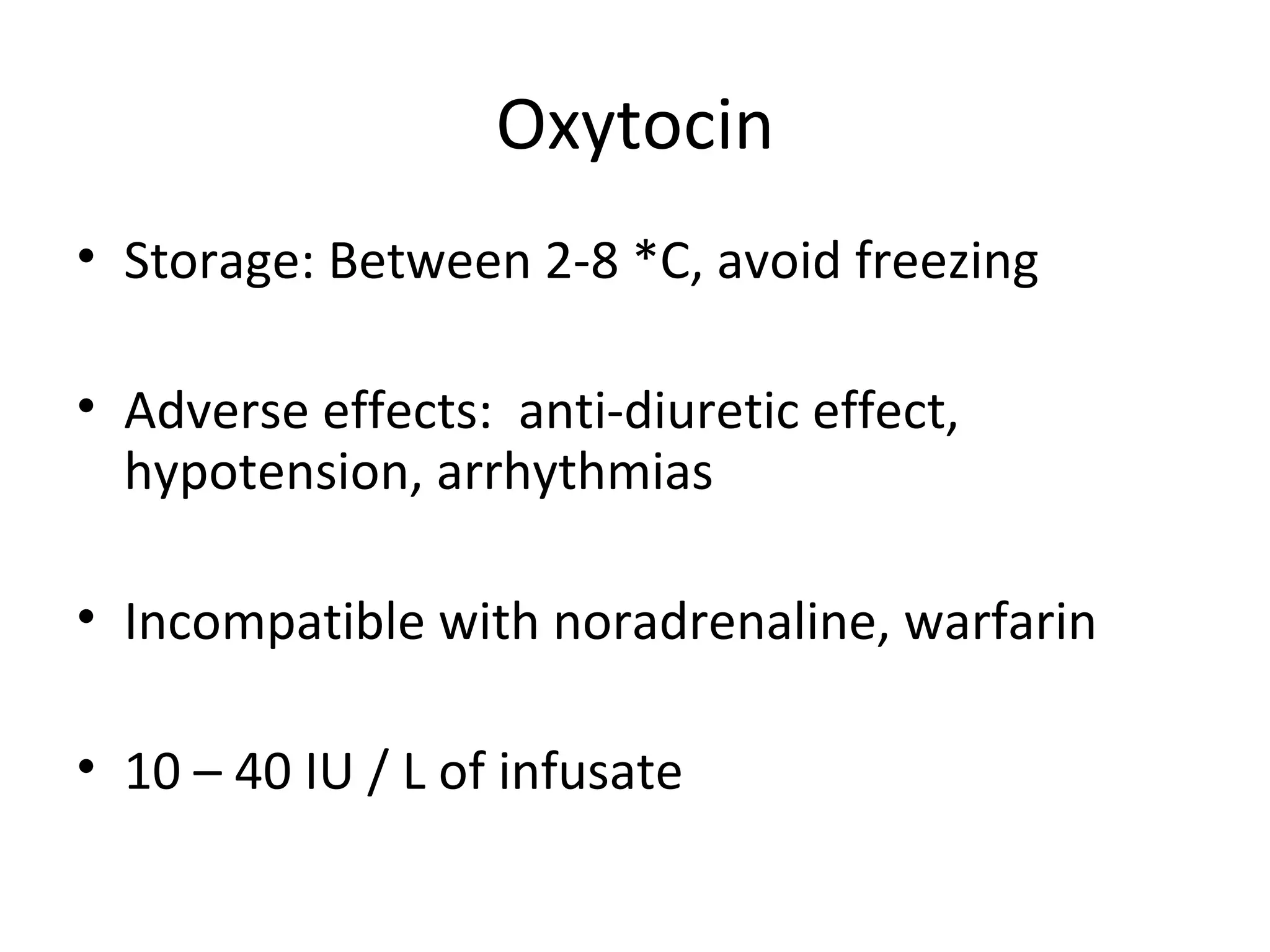
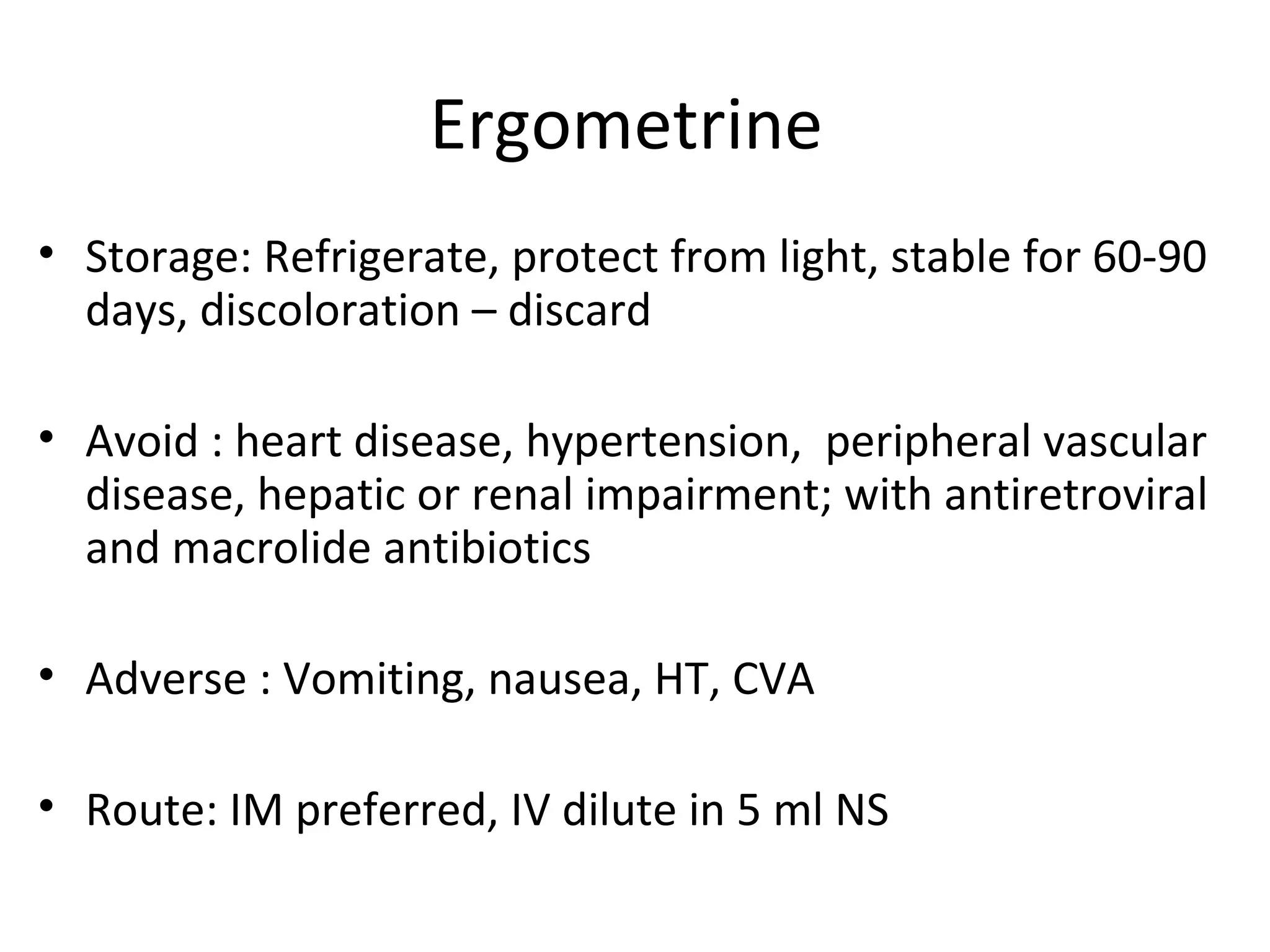
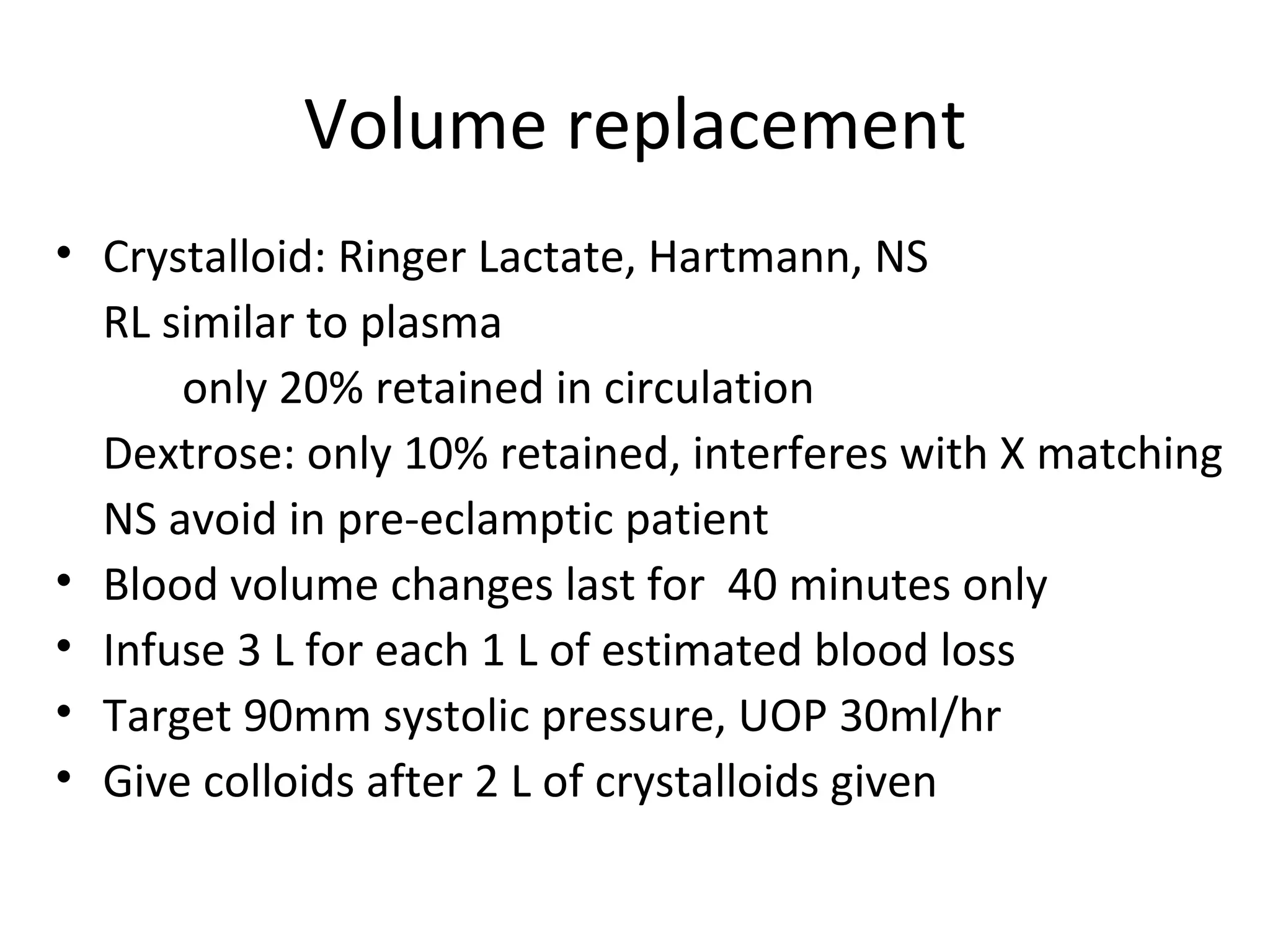
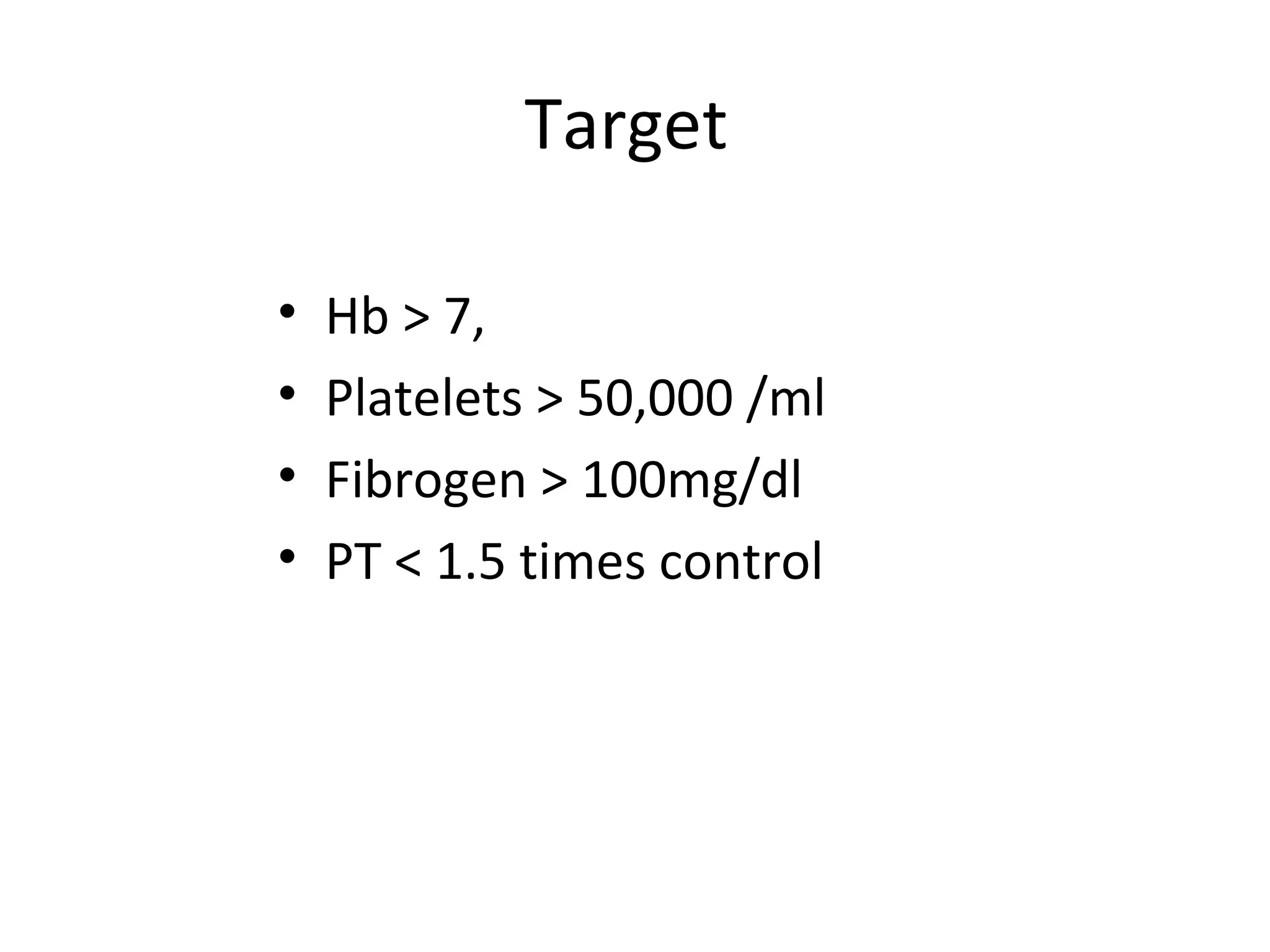
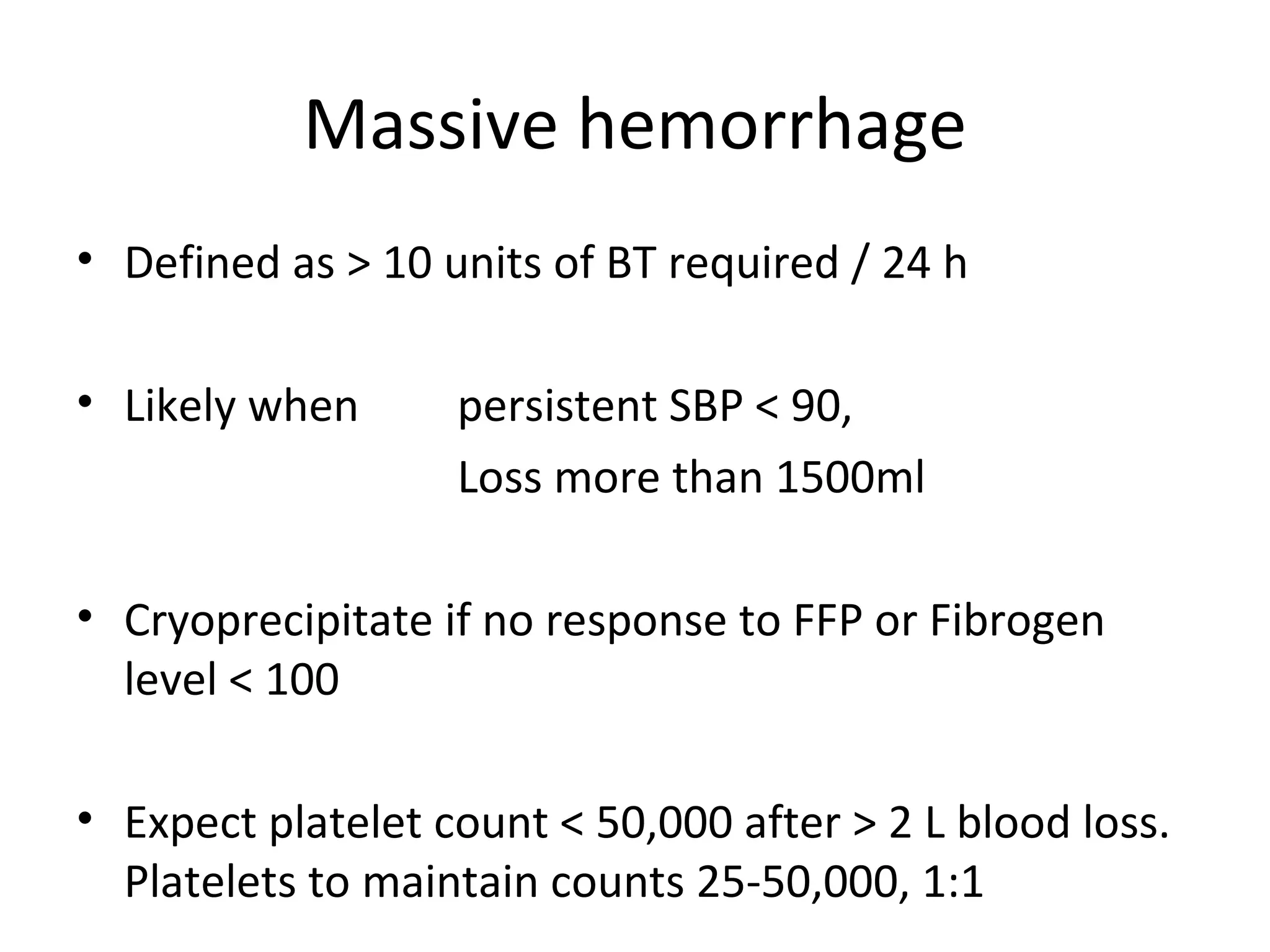
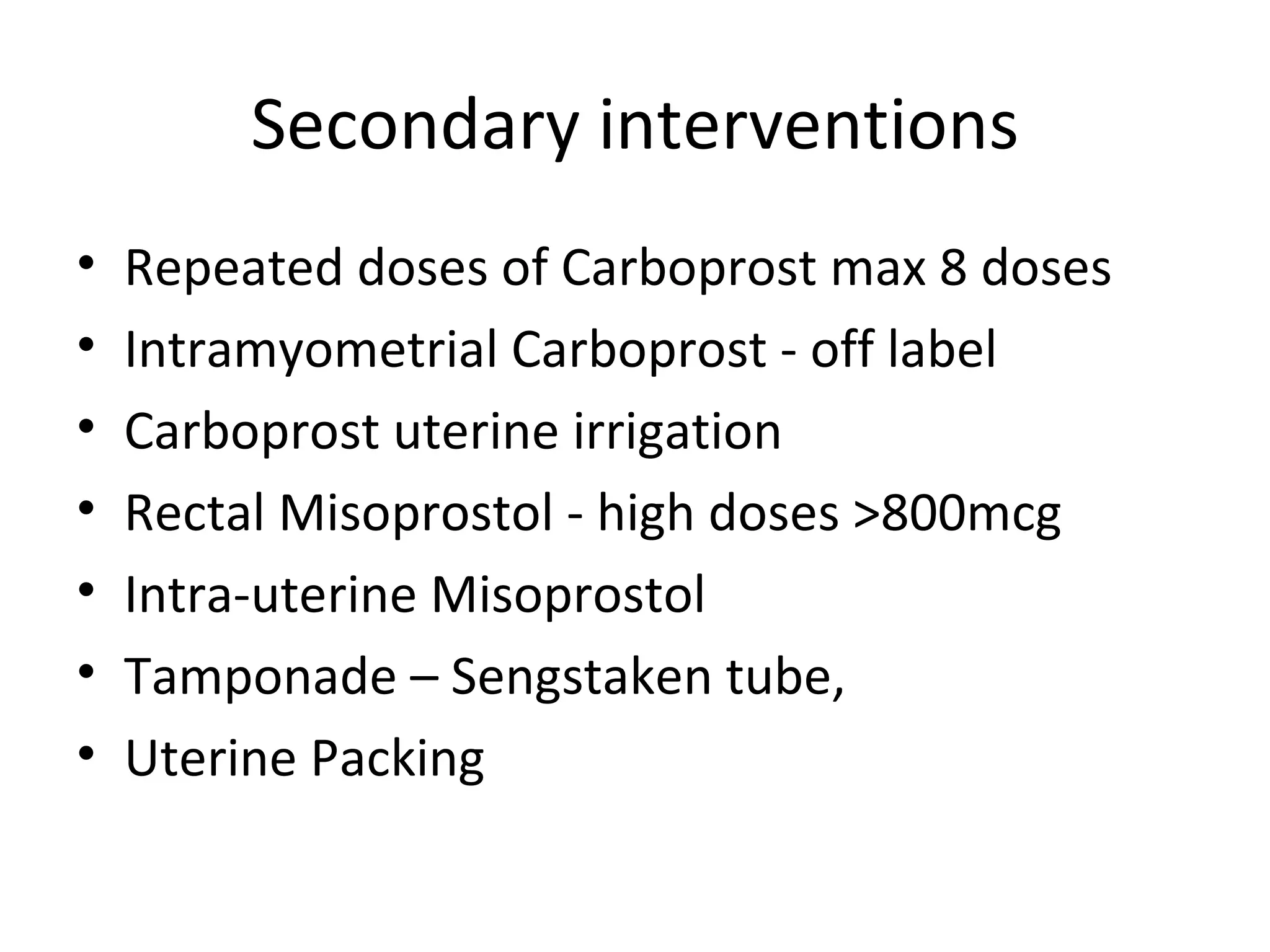
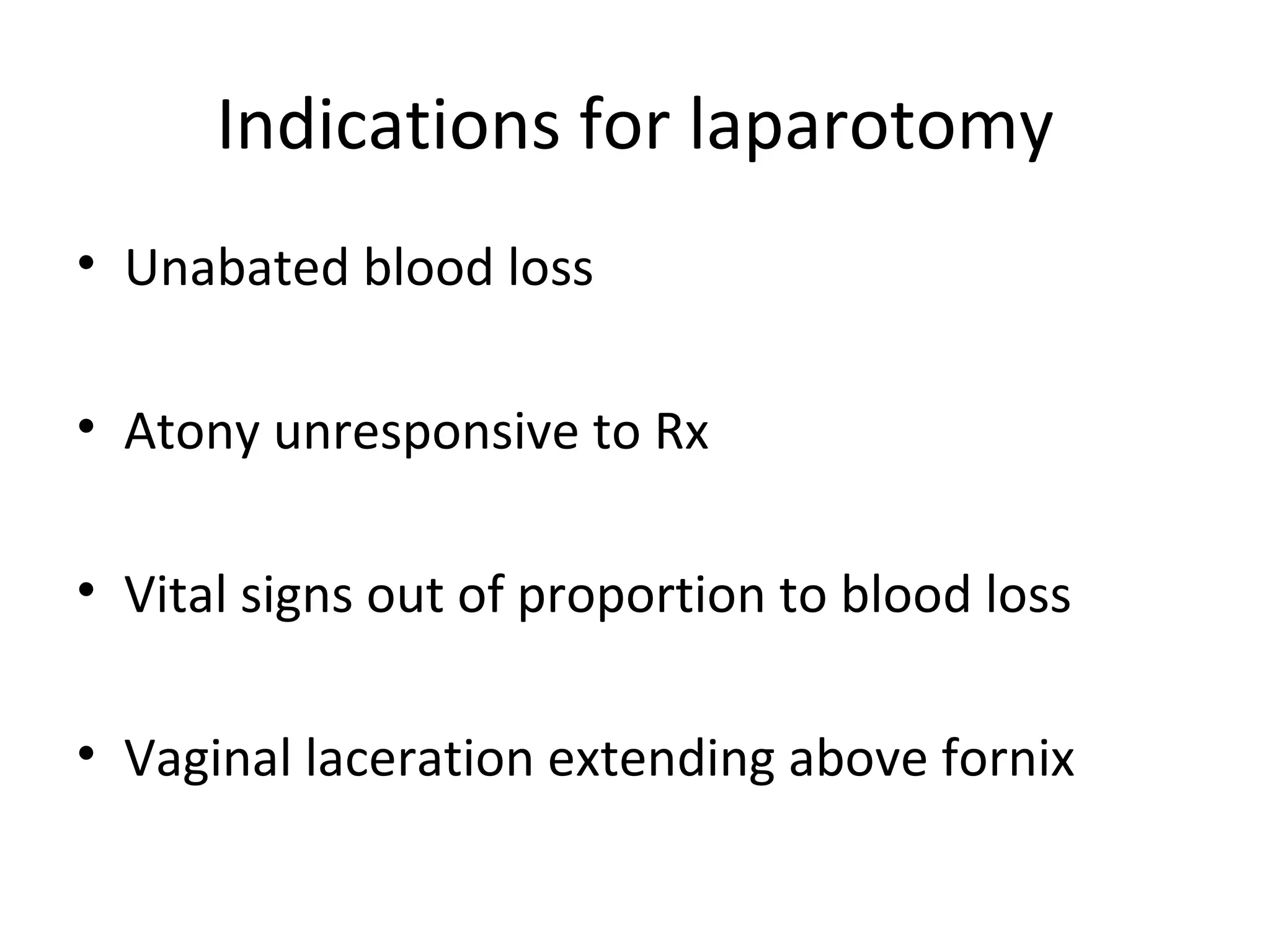
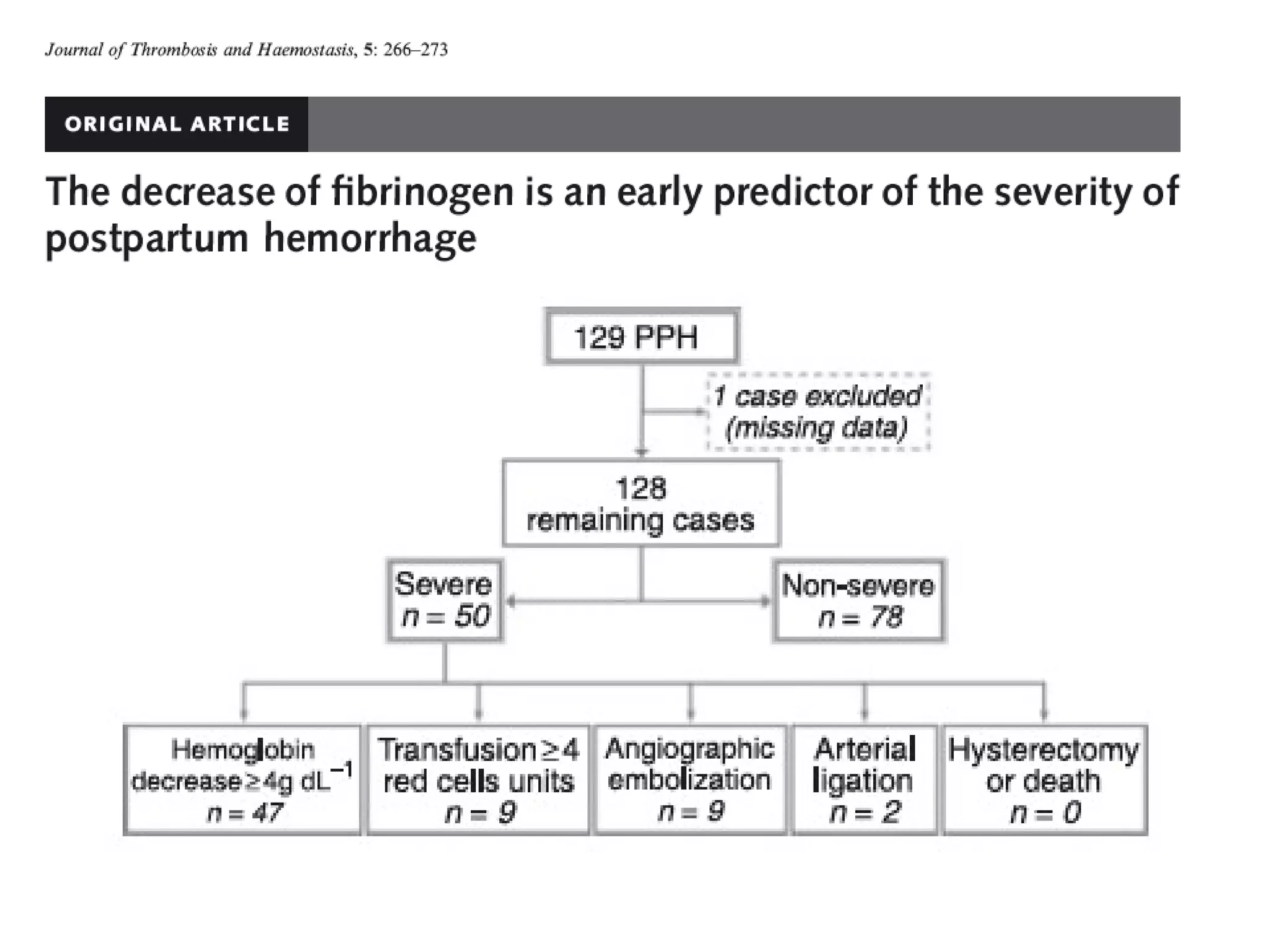
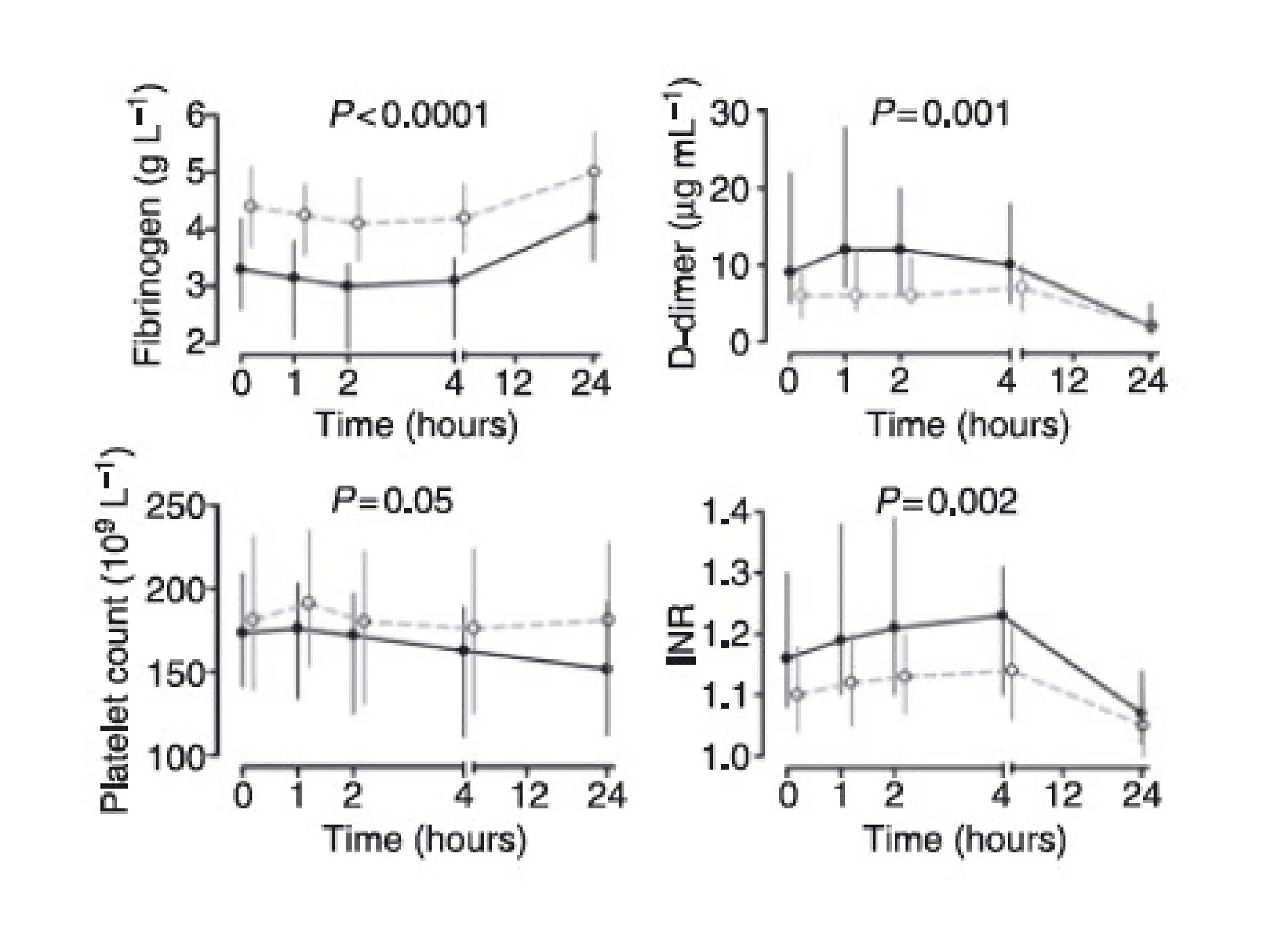
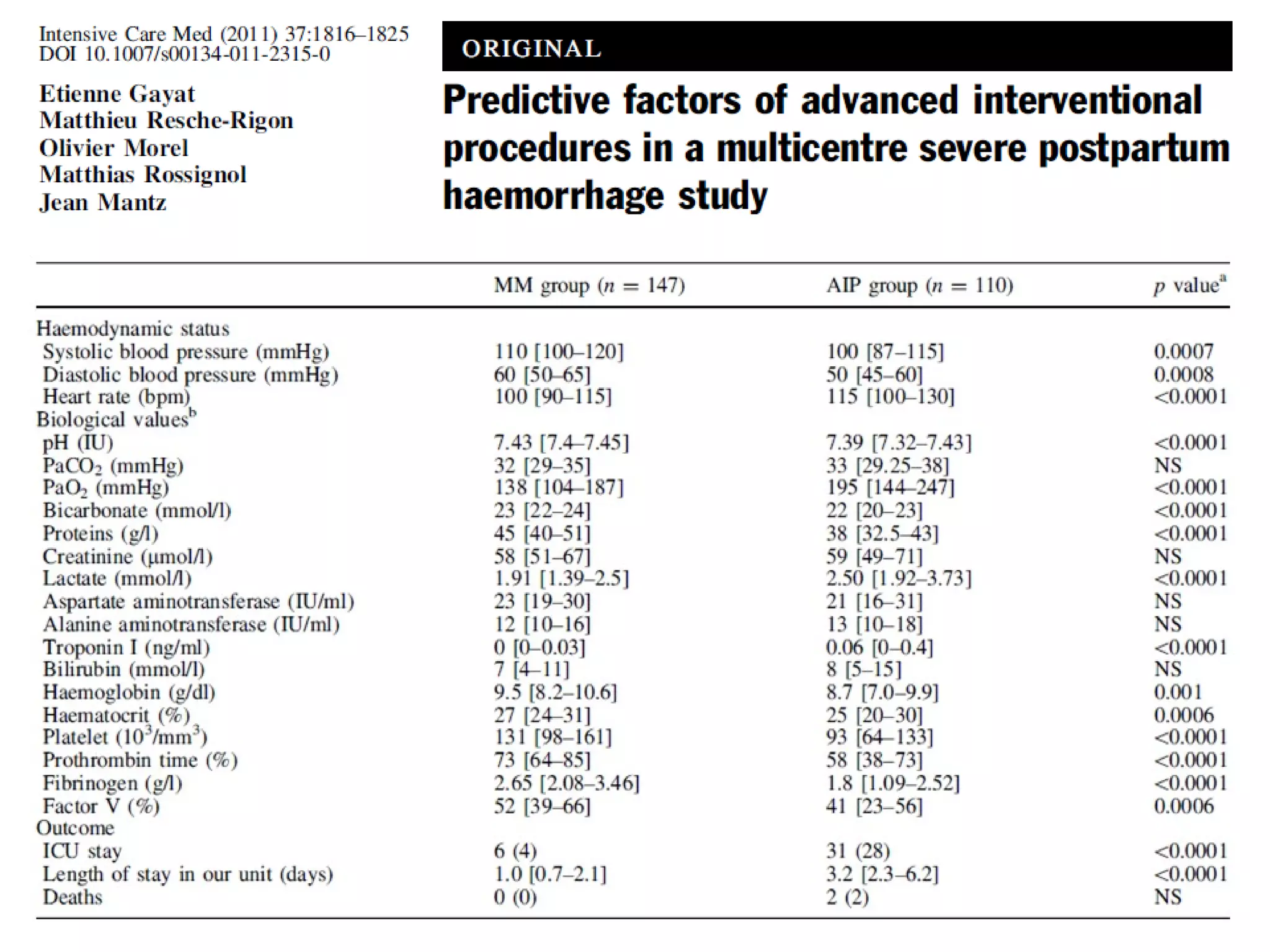
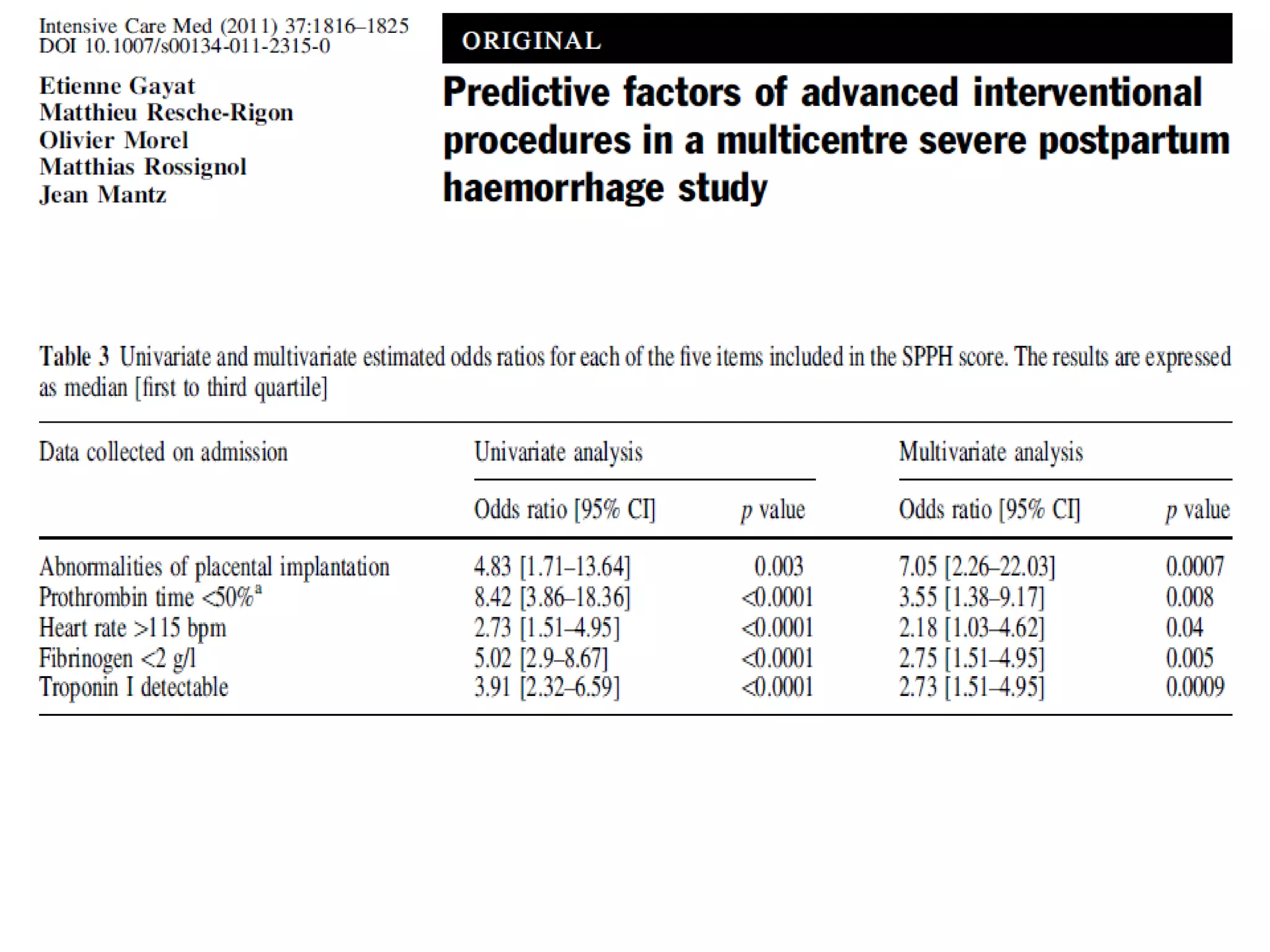
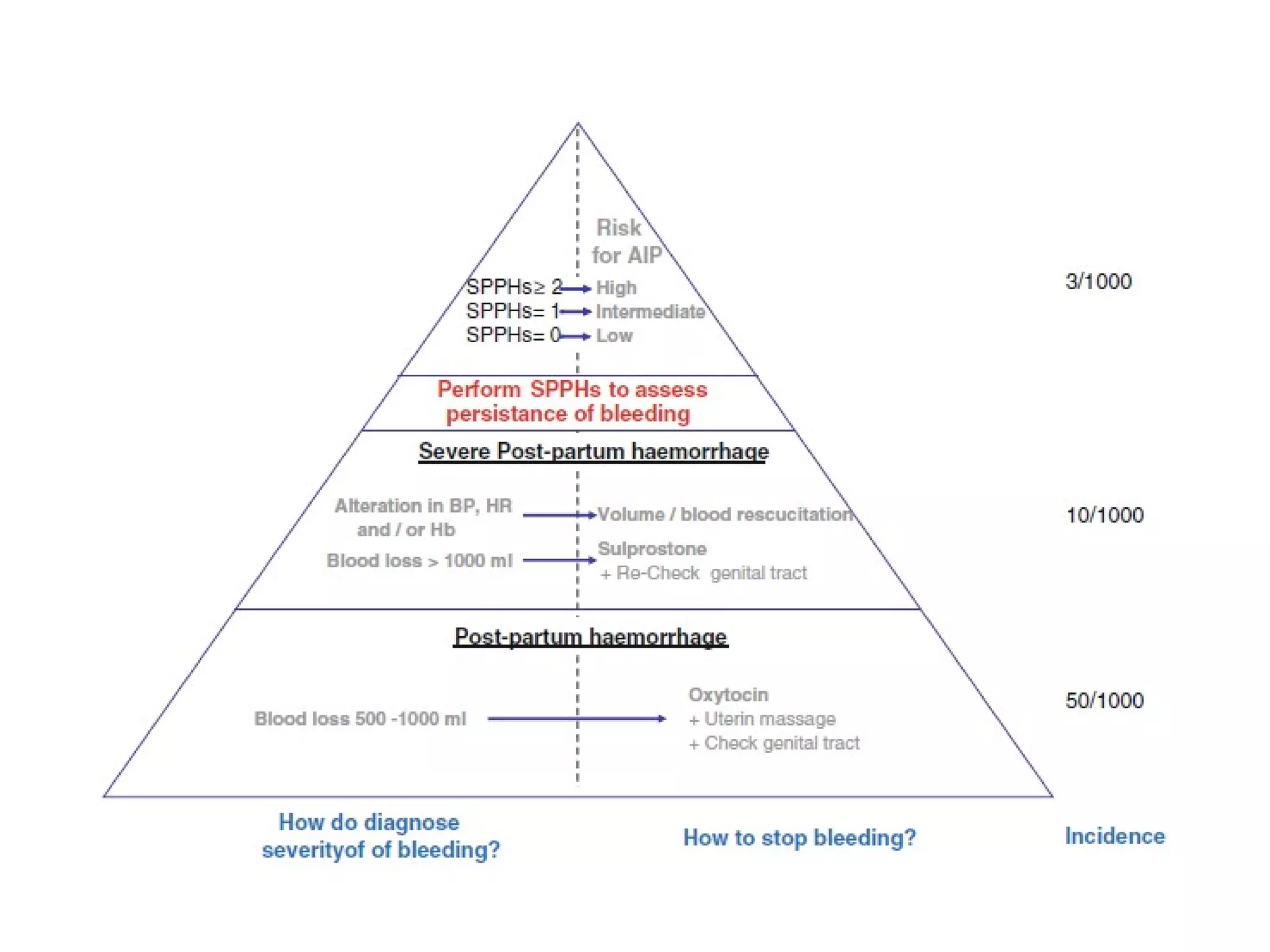
PPH is a leading cause of maternal mortality. It can occur after vaginal or cesarean delivery. Uterine atony accounts for over 80% of cases. Initial management involves calling for help, uterine massage, IV access, rapid fluid resuscitation, and administration of uterotonic drugs like oxytocin, carboprost, and misoprostol. If bleeding continues, examination to check for lacerations or retained products is needed. Blood transfusion may be required based on Hb, platelets, fibrinogen levels. Secondary interventions include additional uterotonics, tamponade, or laparotomy for uncontrolled bleeding. Prompt recognition and treatment following protocols is key to reducing morbidity from PPH.