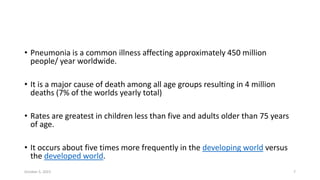
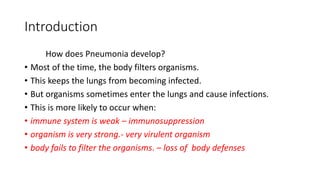
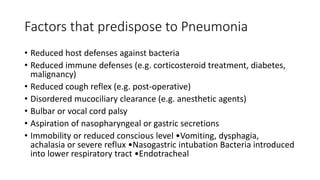
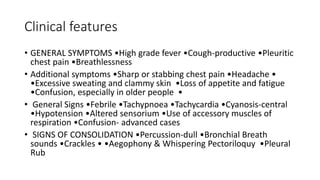
Pneumonia is an infection of the lungs that causes inflammation in the air sacs (alveoli) and makes breathing difficult. It has many potential causes including bacteria, viruses, and other pathogens. The presentation involves symptoms like cough, fever, and chest pain. Diagnosis involves chest x-ray and testing of sputum samples. Treatment depends on severity but generally involves antibiotics, oxygen, fluids and rest. Complications can include lung abscesses, sepsis and respiratory failure. Prevention focuses on vaccination, smoking cessation, and respiratory hygiene.
















![Treatment
• Outpatients Treatment(empirical) Previously healthy and no antibiotics in past 3 months
•A macrolide (clarithromycin or azithromycin or Doxycycline ) Comorbidities or
antibiotics in past 3 months: •Respiratory fluoroquinolone [moxifloxacin ,levofloxacin ] or
β- lactam ( high-dose amoxicillin or amoxicillin/clavulanate)
• Inpatients, non-ICU •A respiratory fluoroquinolone [moxifloxacin ,levofloxacin ] •β -
lactam [cefotaxime ,ceftriaxone ,ampicillin] plus a macrolide [oral clarithromycin or
azithromycin)
• Inpatients, ICU •β -lactam plus Azithromycin or a fluoroquinolone
• Pseudomonas •An antipneumococcal, antipseudomonal β-lactam
[piperacillin/tazobactam, cefepime , imipenem , meropenem plus flouroquinolons
•Above β-lactams plus an aminoglycoside and azithromycin •Above β-lactams plus an
aminoglycoside plus an antipneumococcal fluoroquinolone
• Methicillin-resistant Staphylococcus aureus If MRSA , add linezolid or vancomycin](https://image.slidesharecdn.com/pneumonialecturenotes-231005053159-ceed6b06/85/PNEUMONIA-LECTURE-NOTES-pptx-32-320.jpg)