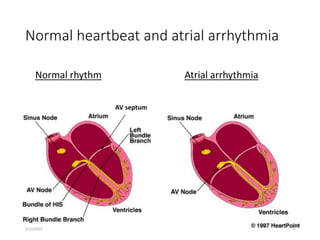
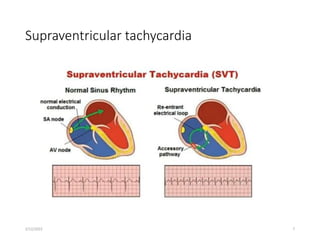
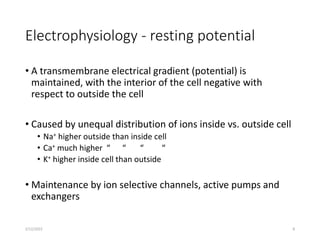
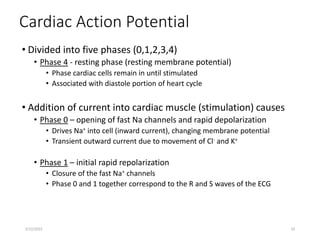
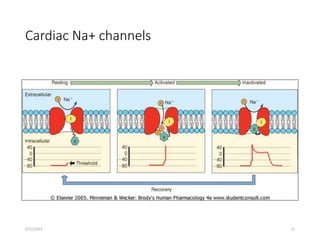
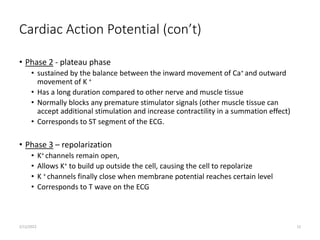
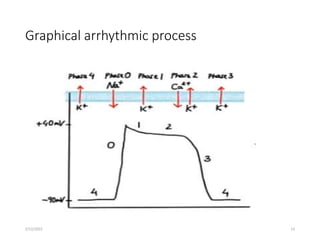
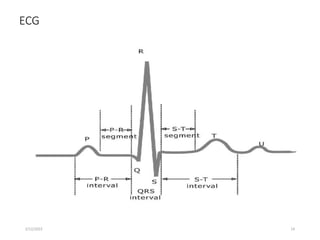
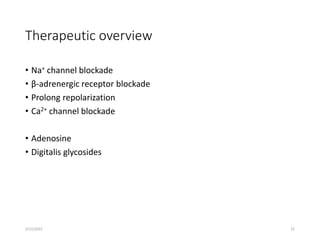
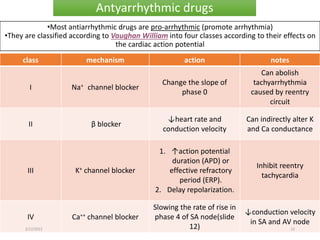
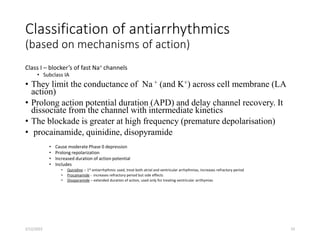
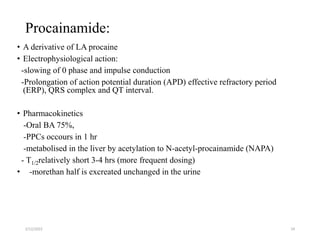
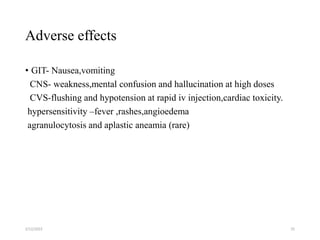
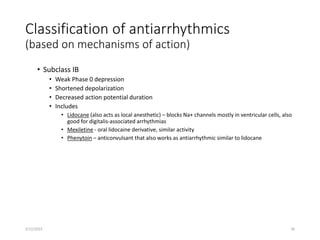
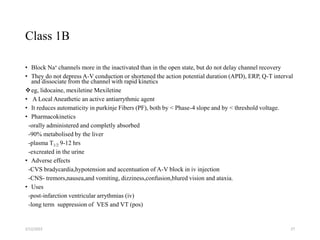
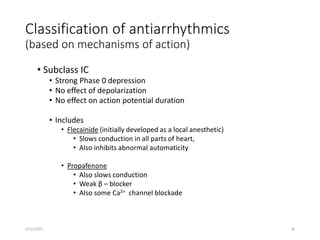
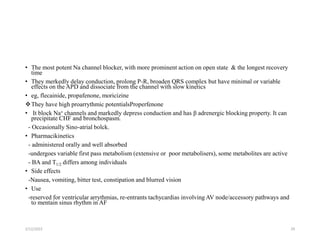
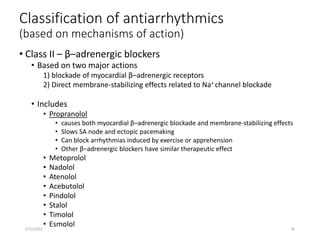
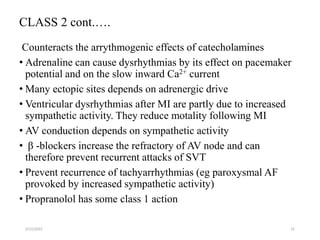
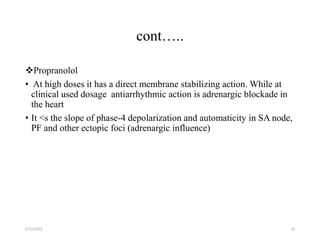
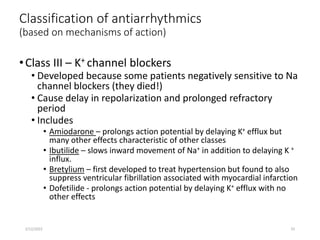
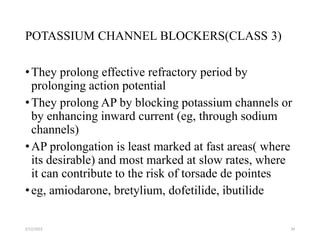
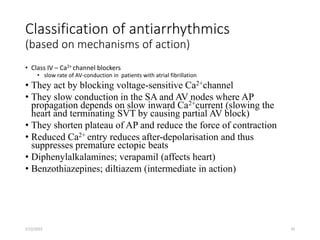
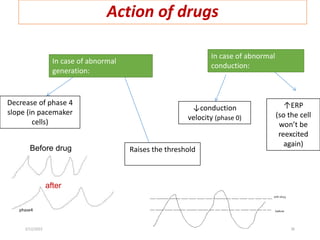
This document provides an overview of antiarrhythmic agents. It begins by defining arrhythmia and discussing the normal cardiac rhythm and electrophysiology. It then examines the mechanisms of cardiac arrhythmias and various causes. Antiarrhythmic drugs are classified into four main classes based on their effects on the cardiac action potential. Examples from each class are discussed along with their mechanisms of action. The classes include sodium channel blockers, beta blockers, potassium channel blockers, and calcium channel blockers.


![2/12/2022 37
Campbell, T. J. & Williams, K. M. (1998). Therapeutic drug monitoring:
Antiarryhthmic drugs. Br J Clin Pharmacol, 46: 307- 319.
Cardiovascular Pharmacology Concepts (2009) Antiarrhythmic Classes. [online]
Available at: www.cvpharmacology.com [Accessed: October 2012].
Stanfield, C. L, & Germann, W. J. Principles of Human Physiology. 3. London,
England: Benjamin Cummings, 2007. Print.
phm.utoronto.ca/~jeffh/PPT/phm12barr.ppt
www.ksums.net/.../2.%20antiarrhythmic%20dr..
faculty.ksu.edu.sa/.../Antiarrhythmic%20Drugs..
References](https://image.slidesharecdn.com/antiarrythmia-221202075624-1d1f0ea2/85/ANTIARRYTHMIA-37-320.jpg)