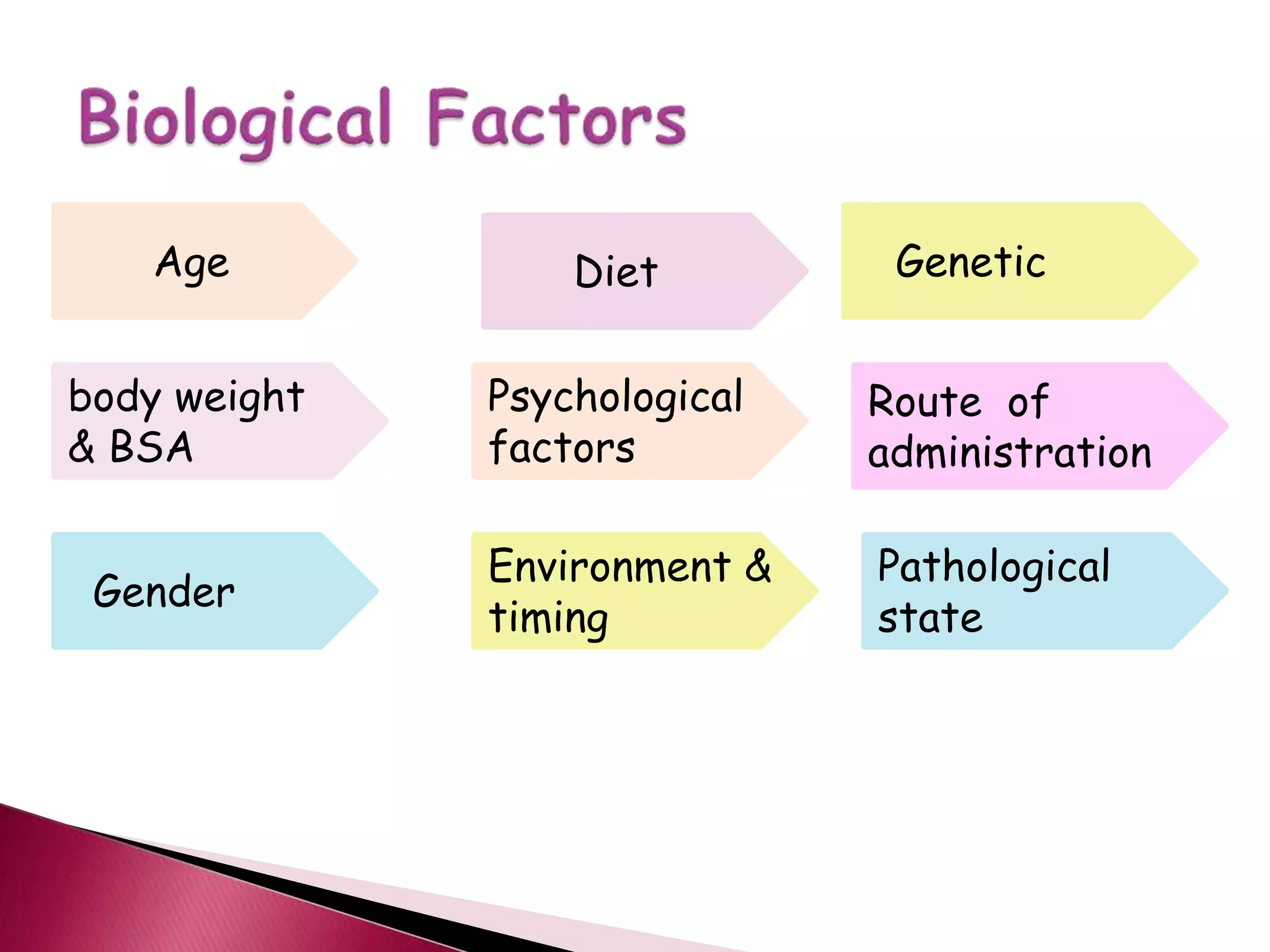
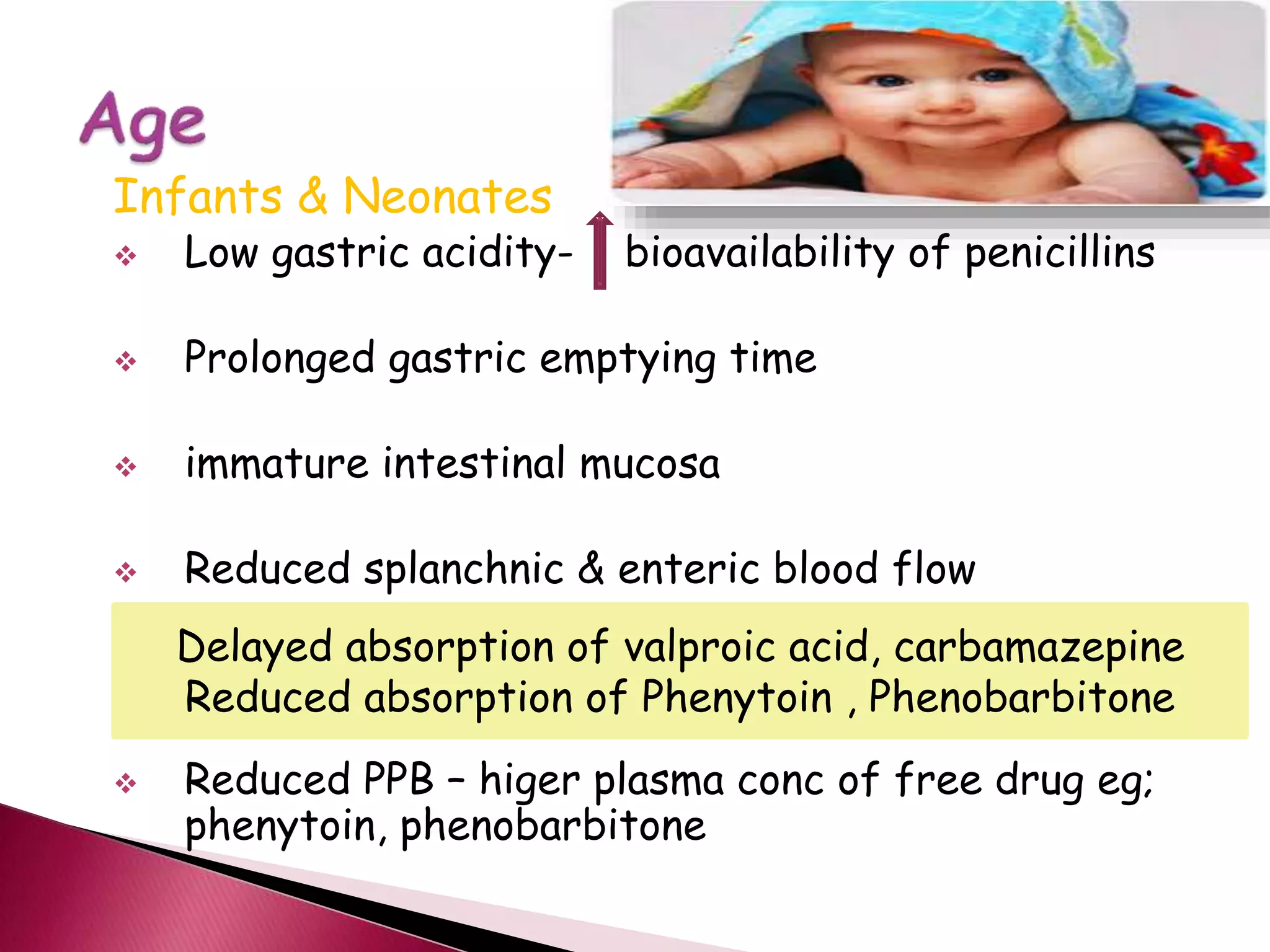
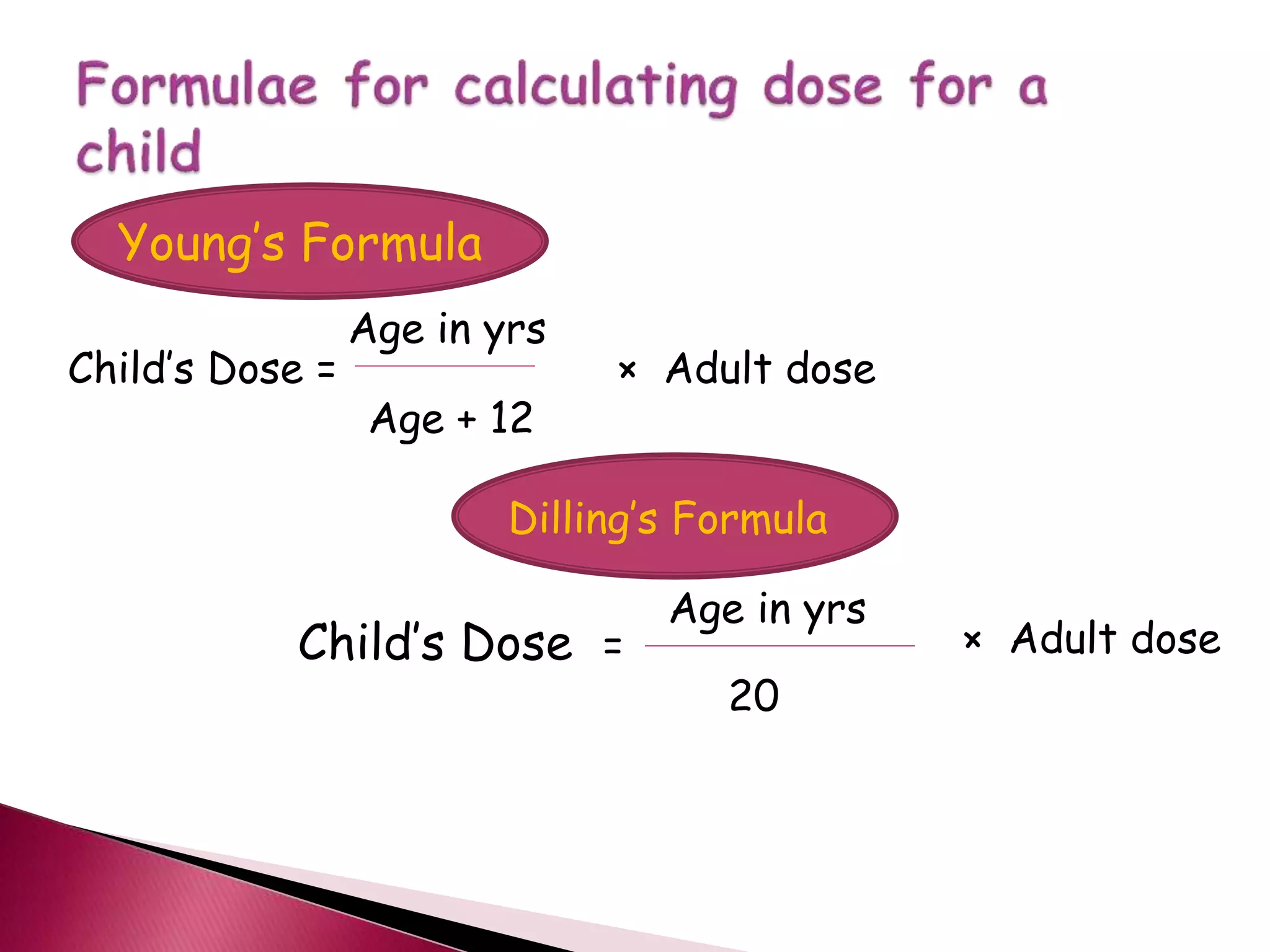
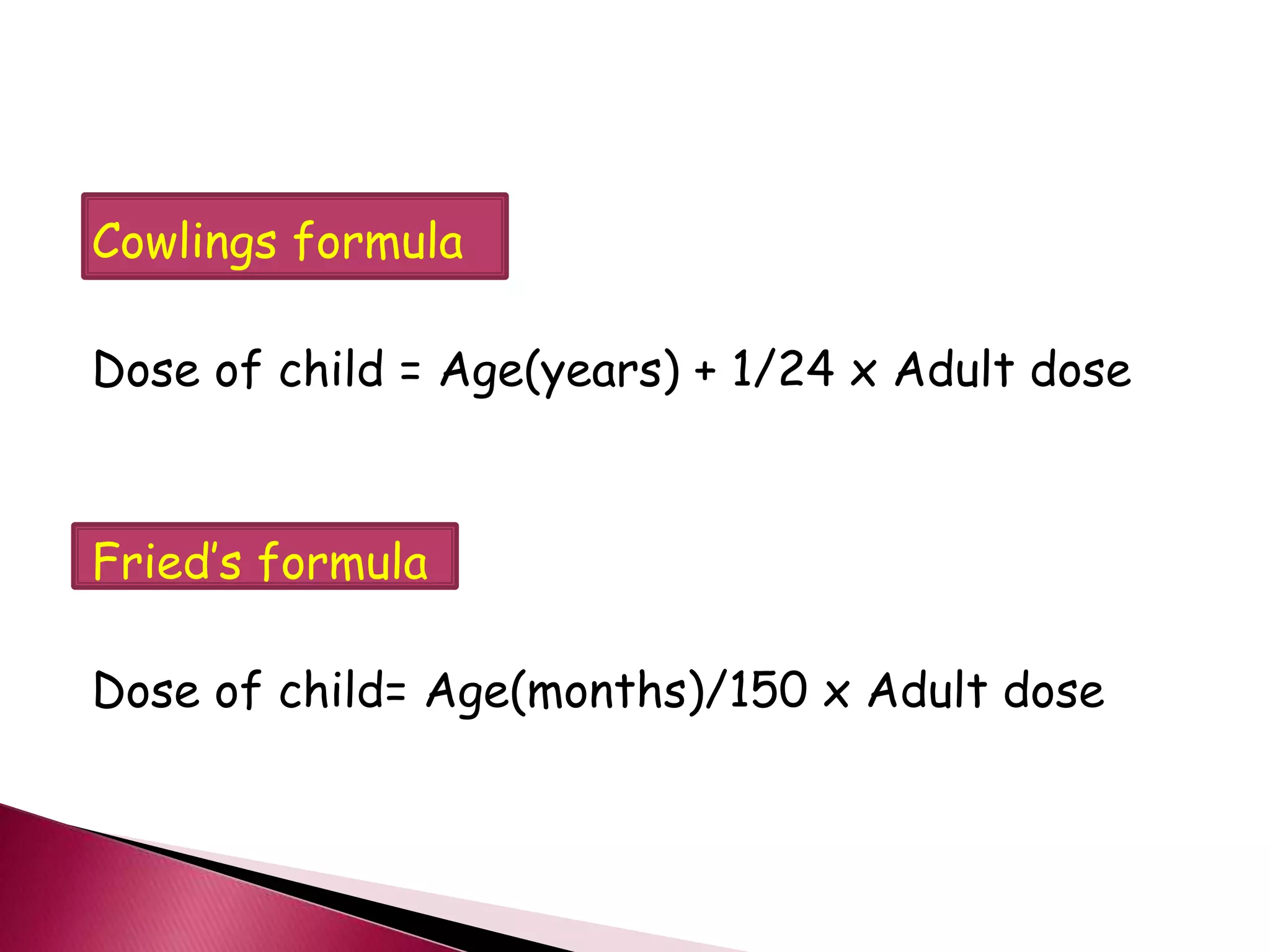
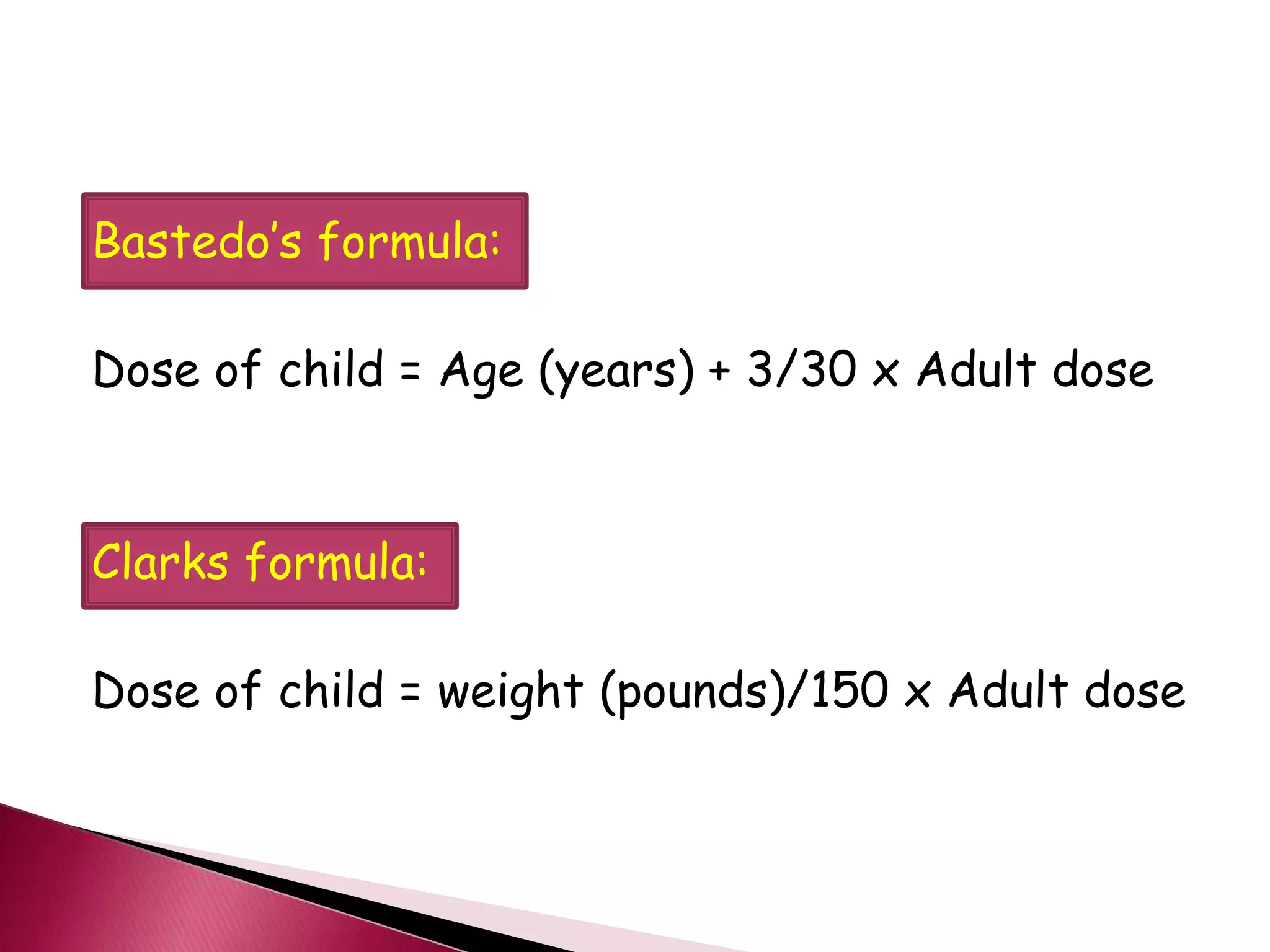
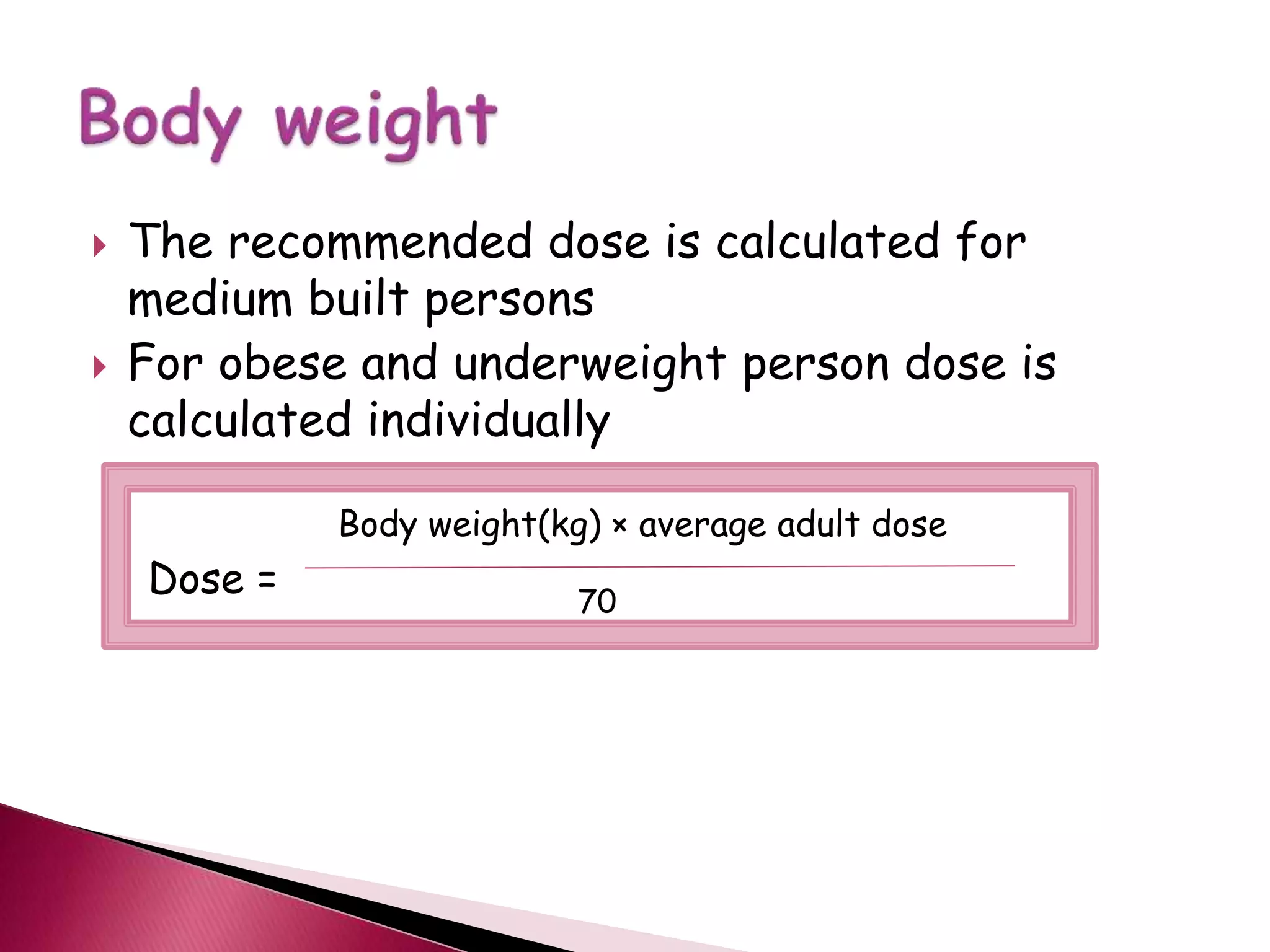
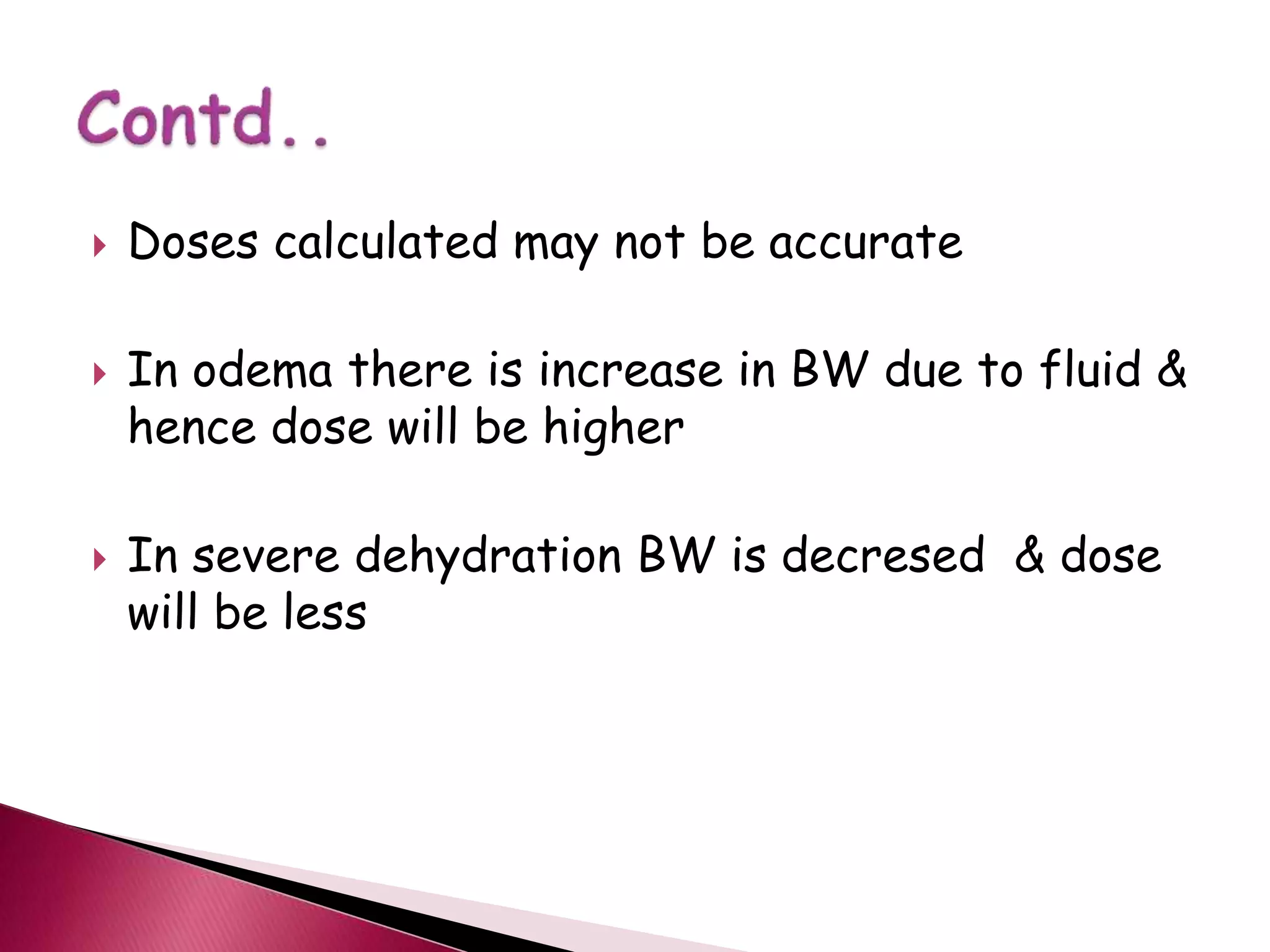
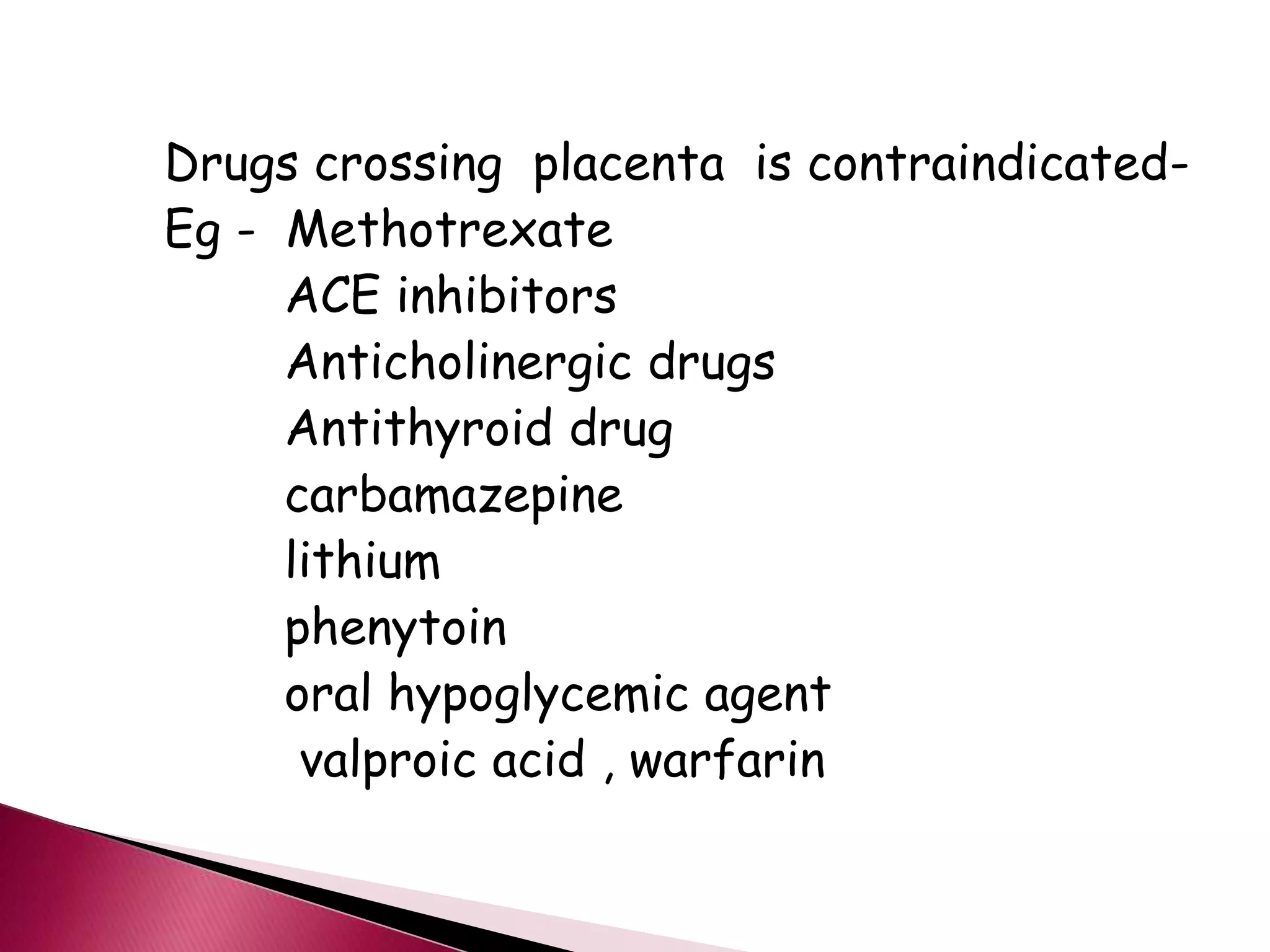
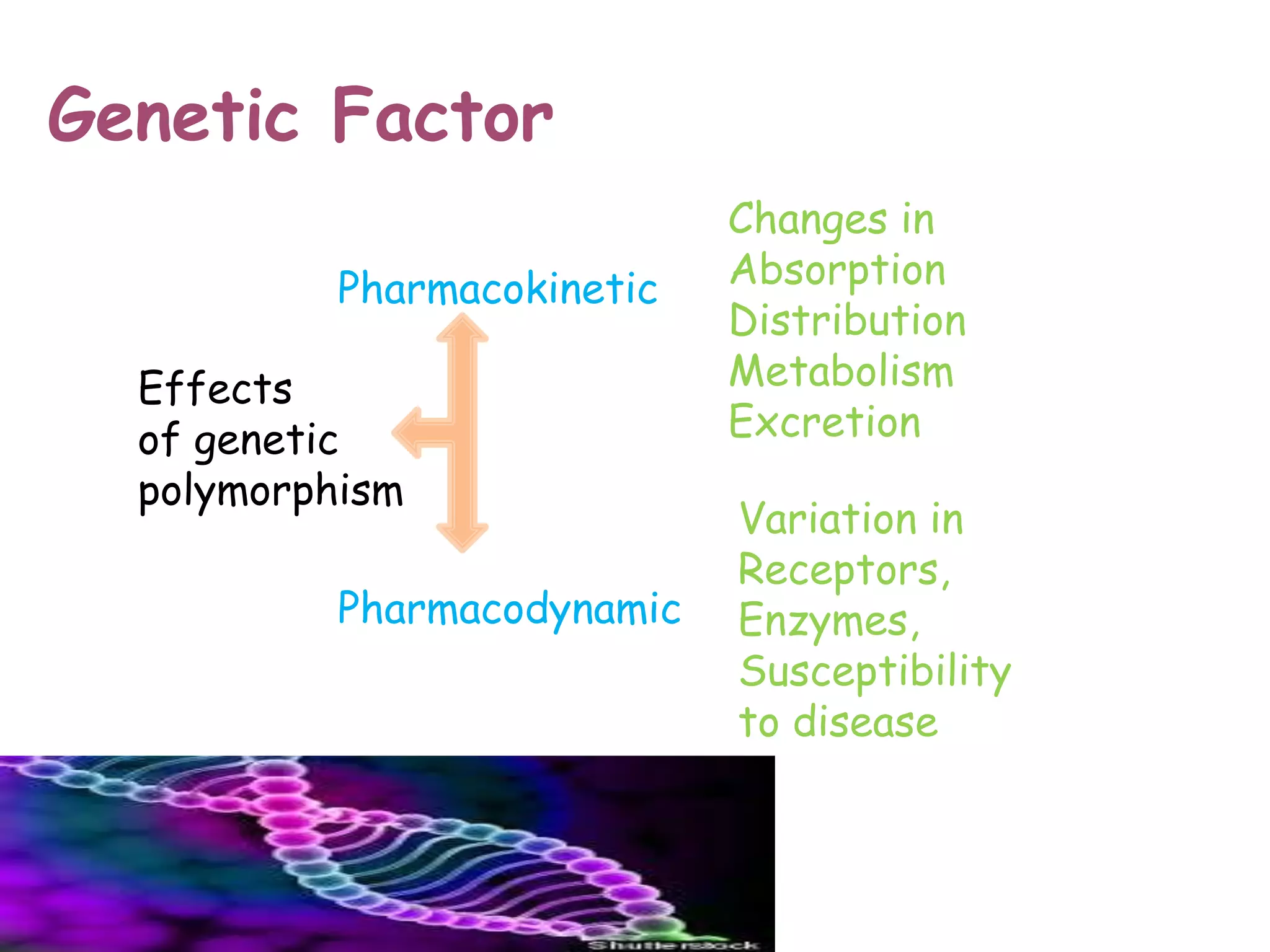
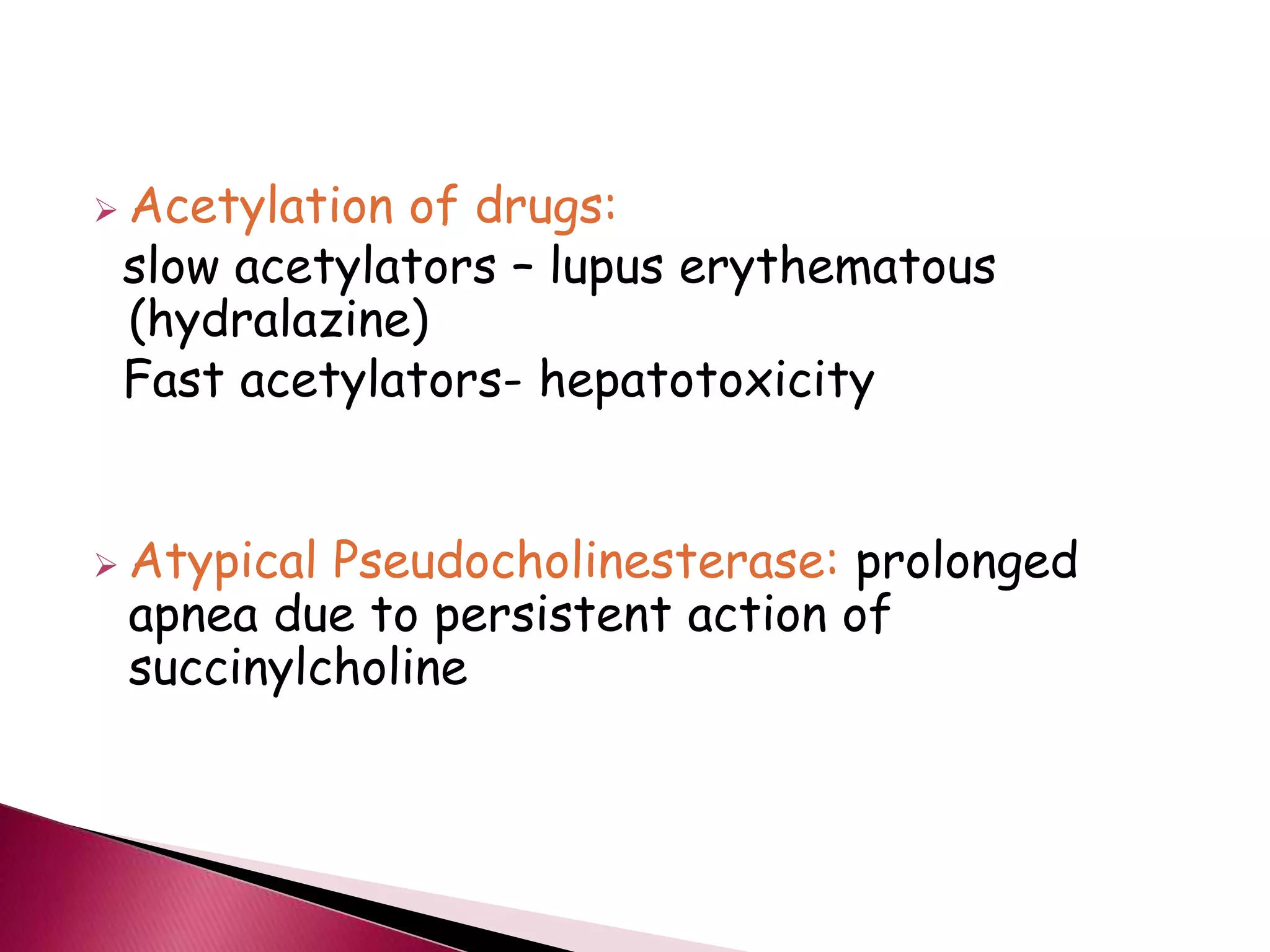
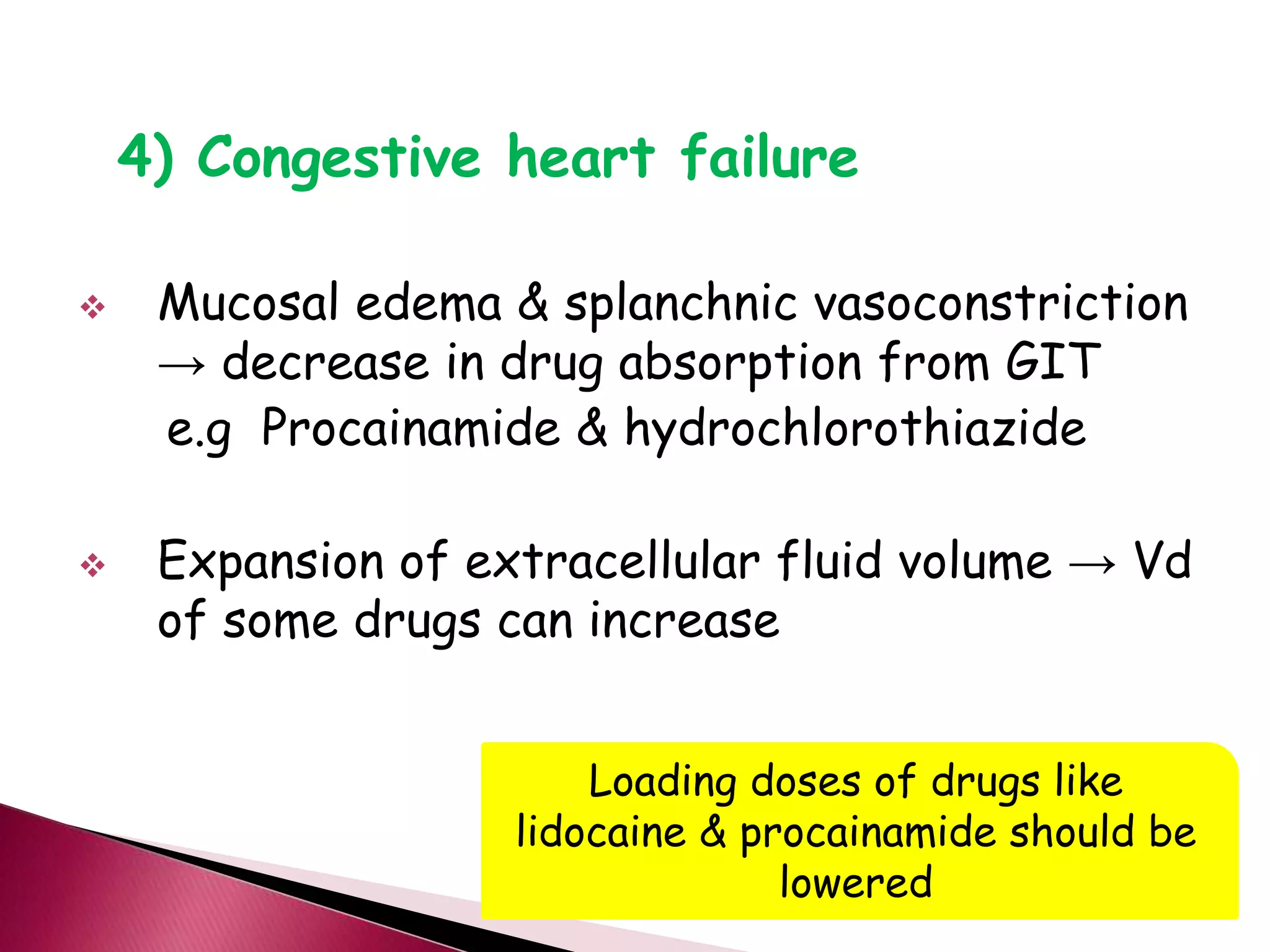
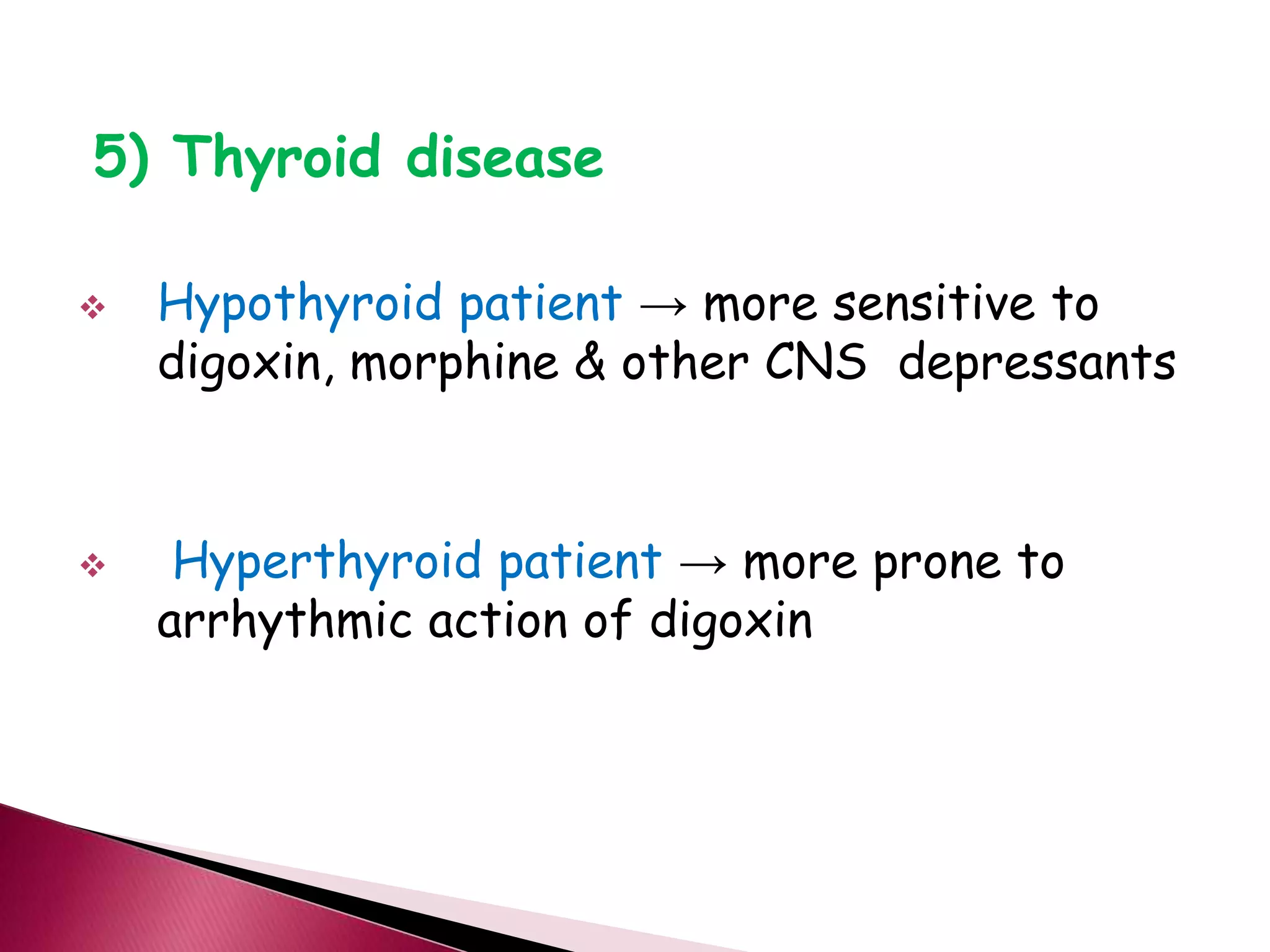
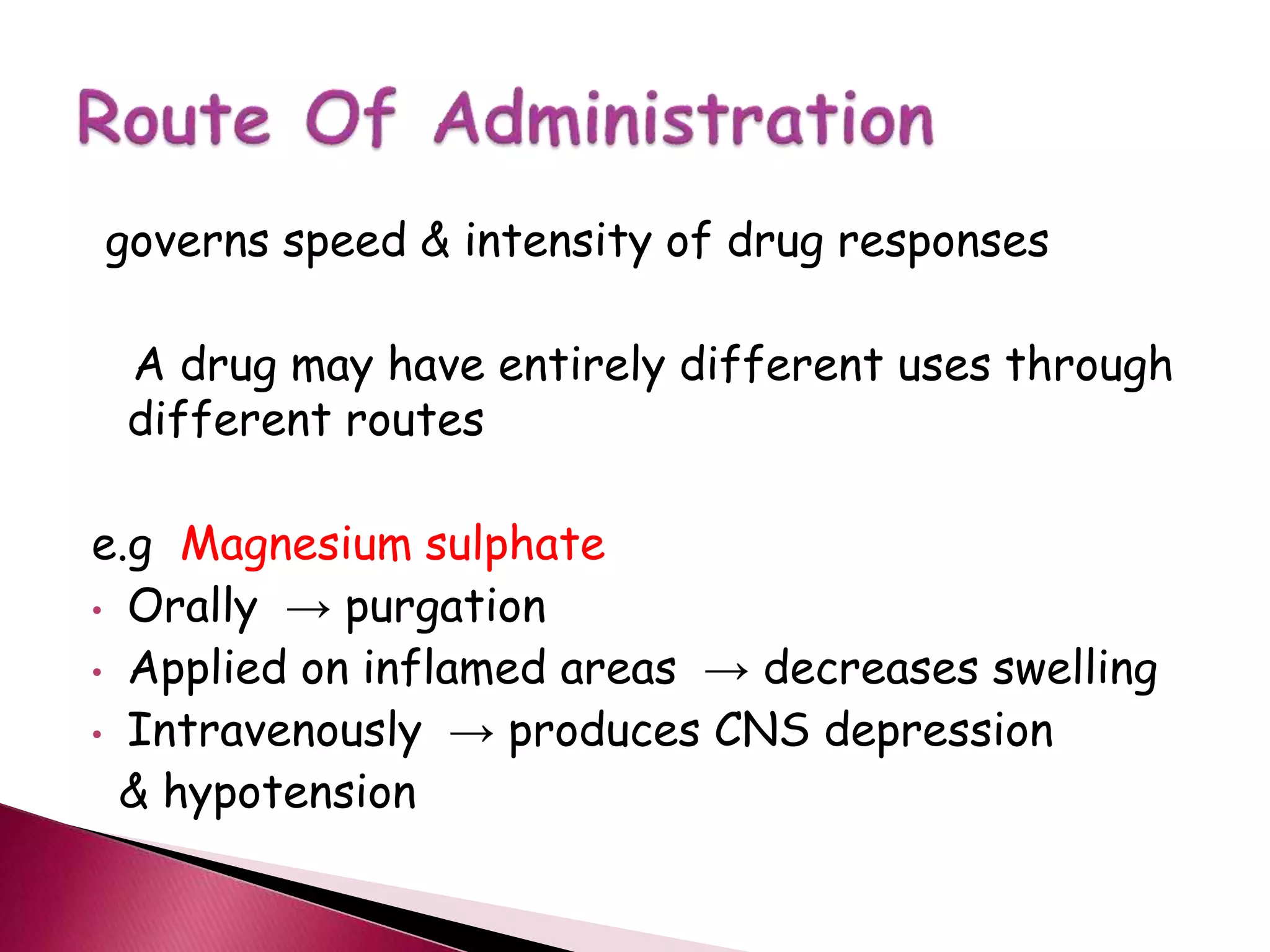
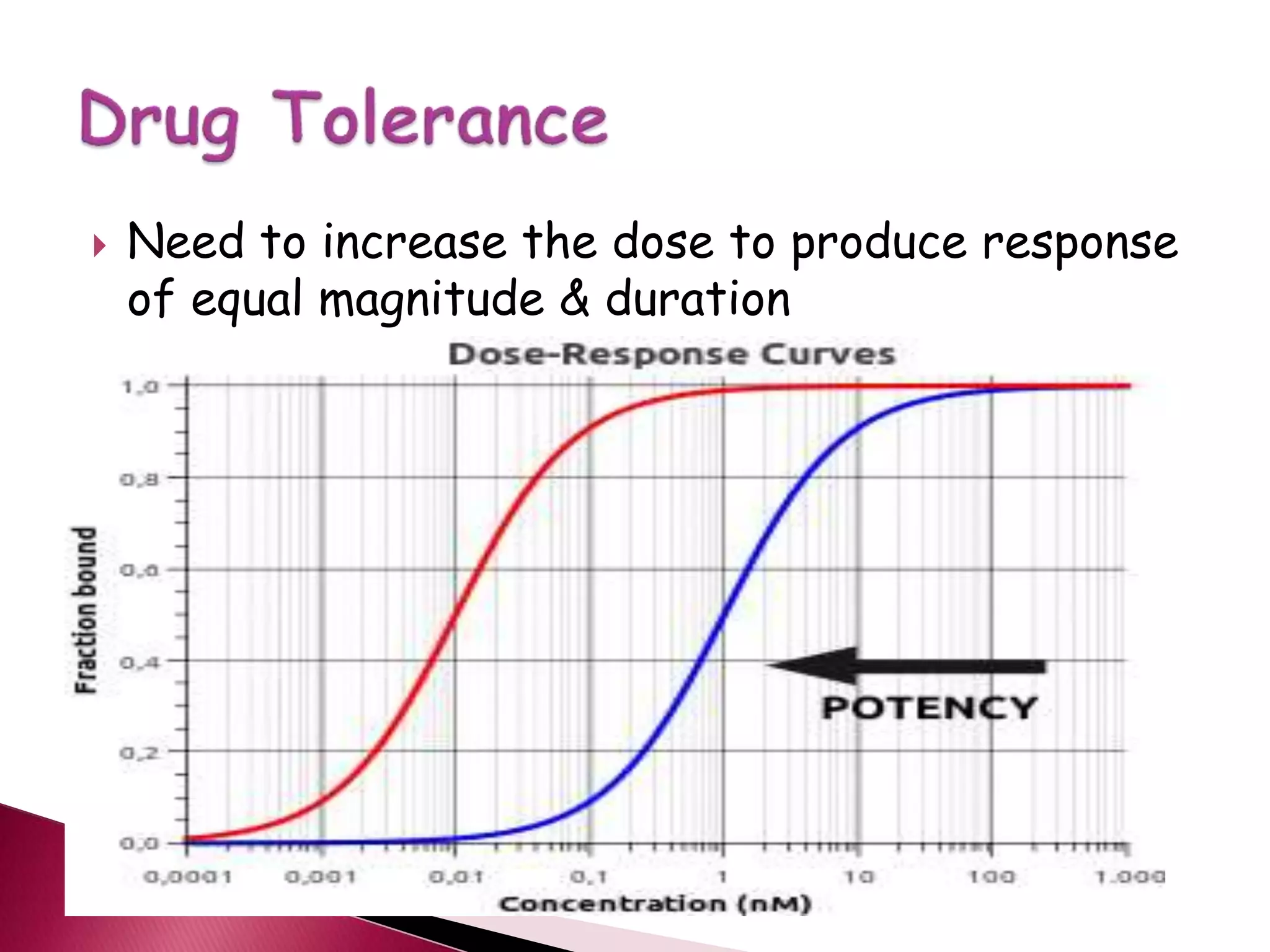
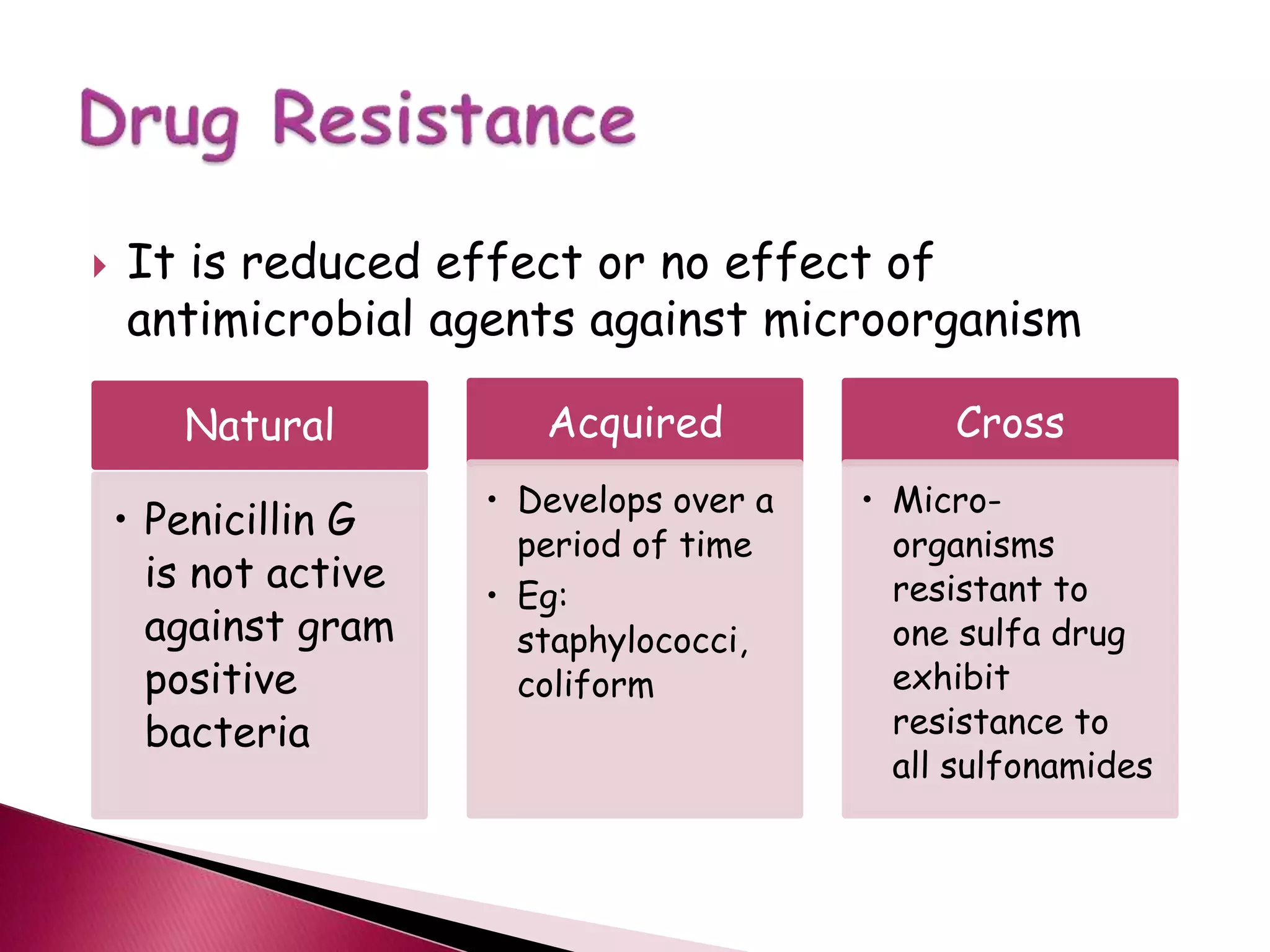
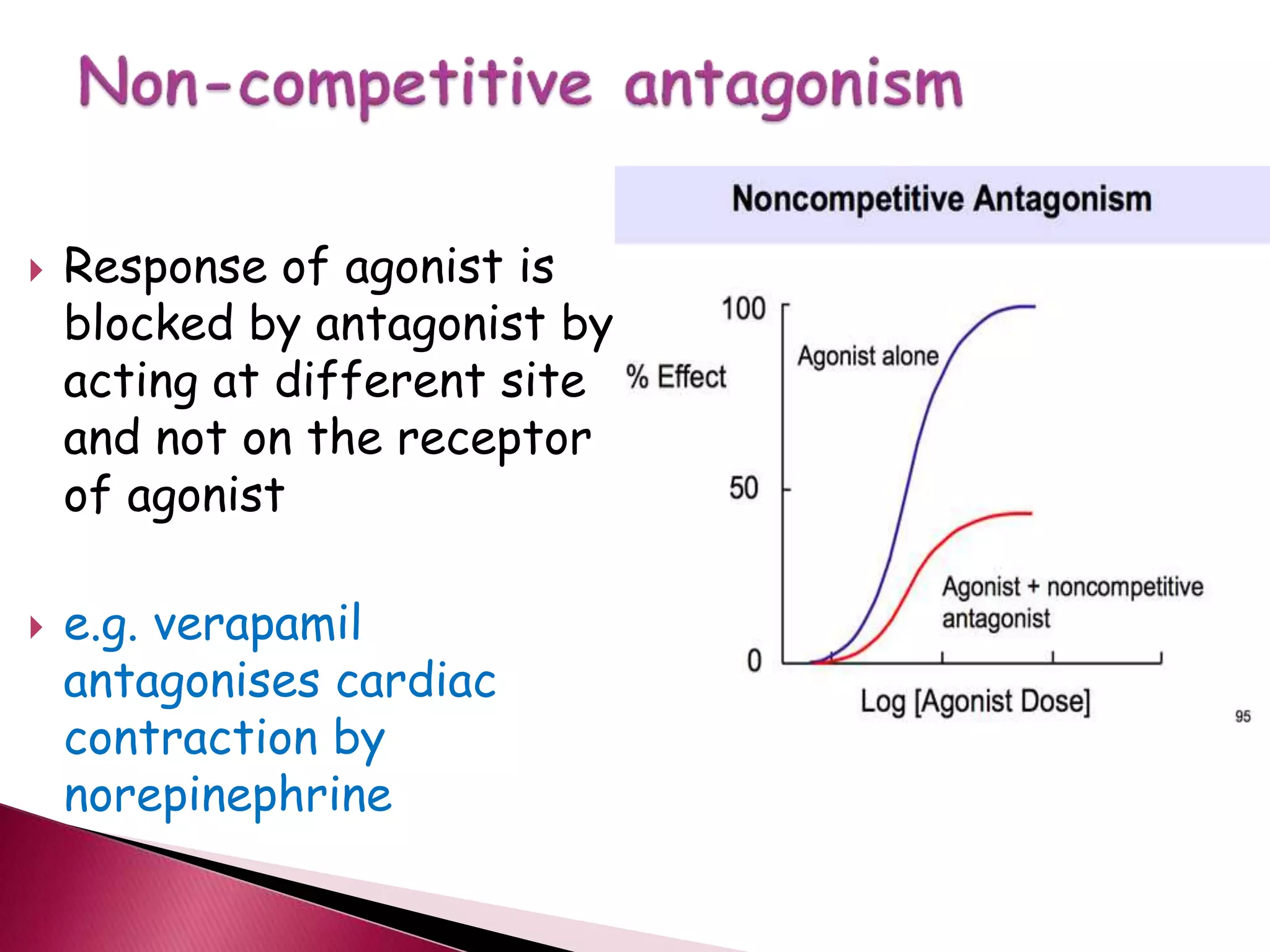
This document discusses factors that can modify a drug's effects in the body. It summarizes that individual responses to drugs can vary due to differences in pharmacokinetics and pharmacodynamics. Genetic and non-genetic factors like age, disease states, diet, and concurrent medications can impact drug absorption, distribution, metabolism, and excretion. Drug interactions, tolerance, and cumulative effects are also reviewed. The document emphasizes considering a patient's individual factors when determining appropriate drug dosing to achieve the desired therapeutic effects while avoiding unnecessary adverse reactions.