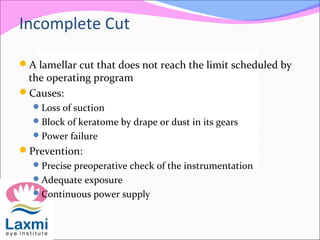
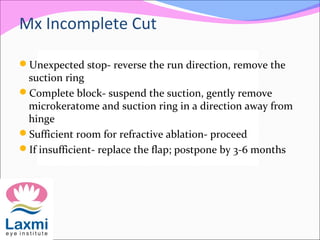
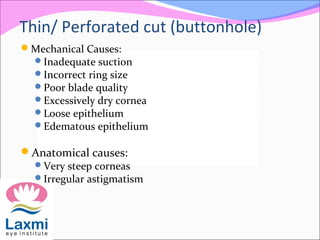
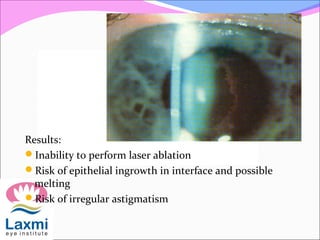
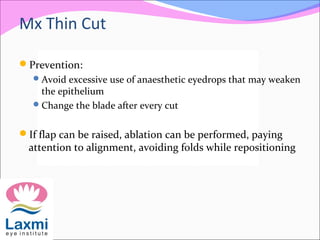
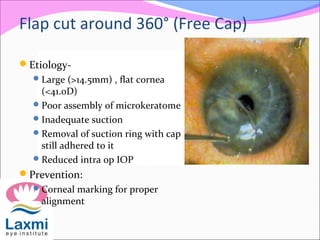
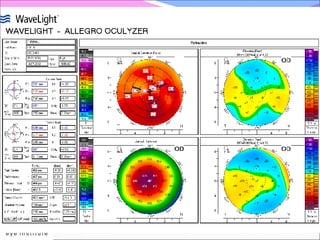
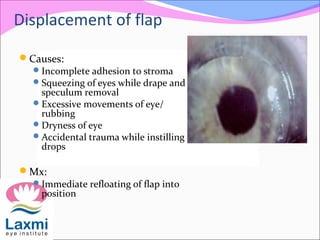
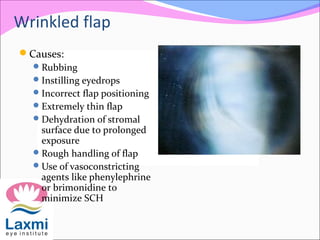
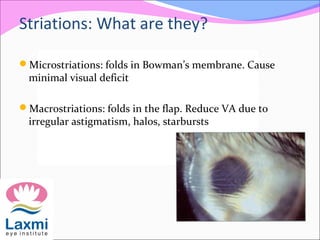
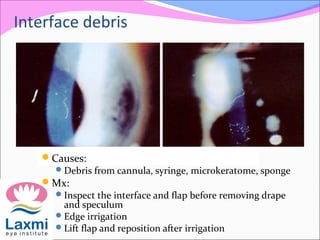
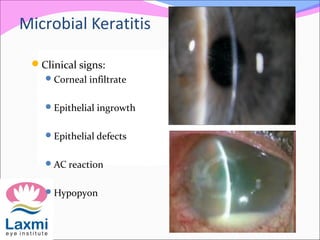
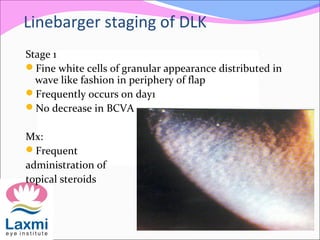
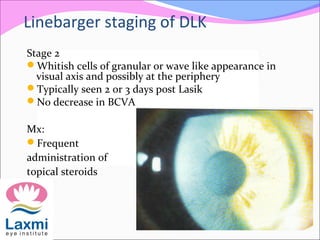
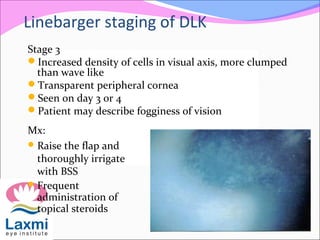
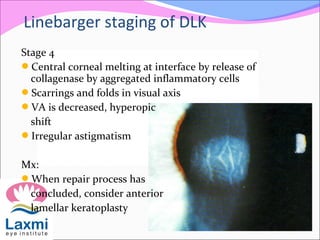
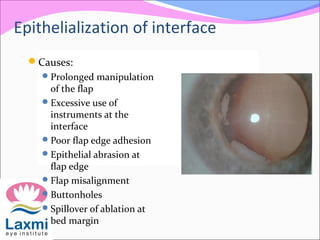
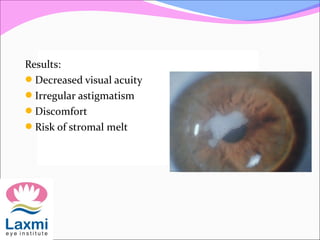
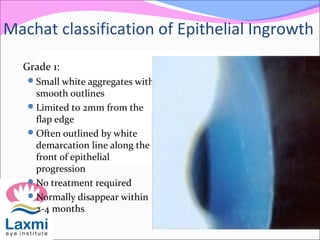
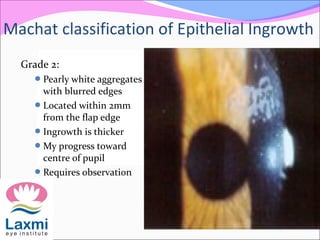
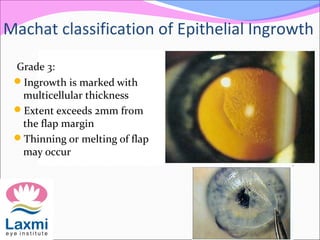
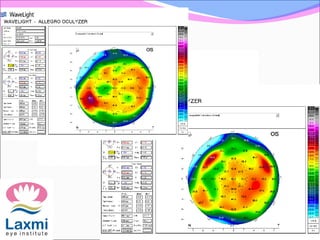
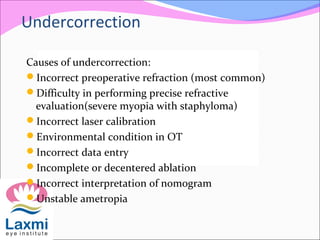
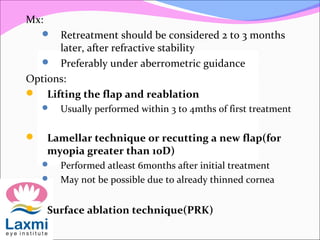
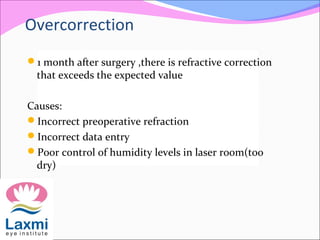
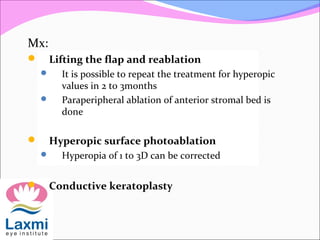
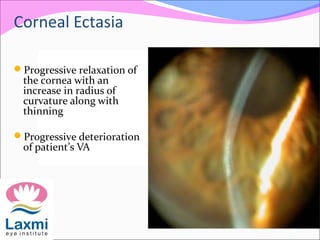
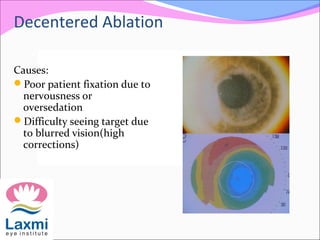
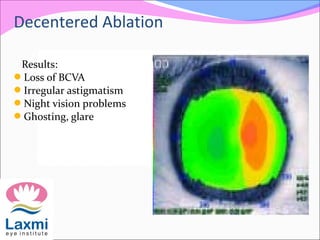
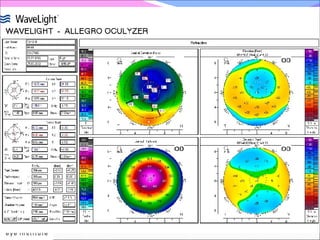
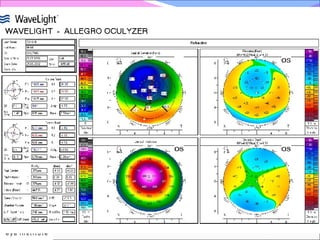
This document discusses LASIK complications and their management. It describes potential intraoperative complications such as incomplete cuts, thin cuts, and free caps. Early postoperative complications include flap-related issues like displacement, wrinkling, and striations. Late complications include epithelial ingrowth, diffuse lamellar keratitis, microbial keratitis, and corneal ectasia. Refractive complications like irregular astigmatism, undercorrection, overcorrection, regression, and ectasia are also reviewed. Prevention and management strategies are provided for each complication.