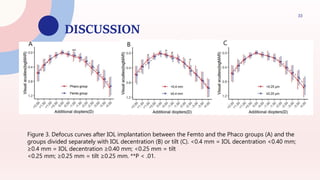
This study compared visual outcomes after cataract surgery using femtosecond laser-assisted cataract surgery (FLACS) versus conventional phacoemulsification (CPS) with implantation of an extended depth of focus (EDOF) intraocular lens (IOL). The study found that FLACS produced significantly less IOL decentration and tilt, lower wavefront aberrations, better contrast sensitivity, and fewer visual disturbances reported by patients. Therefore, FLACS may provide improved visual performance compared to CPS when using an EDOF IOL by achieving a more precisely centered IOL position. The study provides evidence that lens positioning is an important factor for optimal visual outcomes with EDOF IOLs.