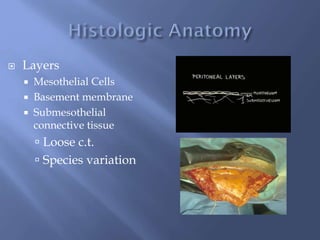
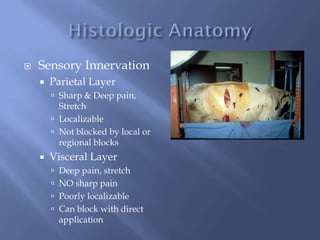
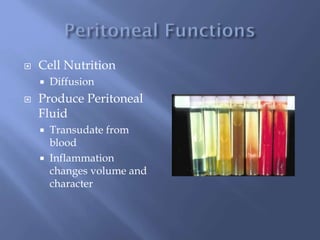
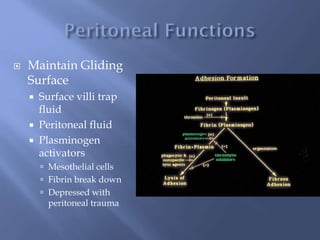
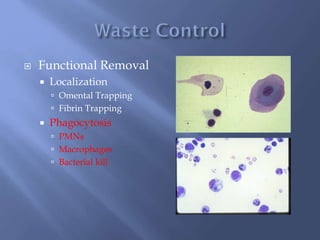
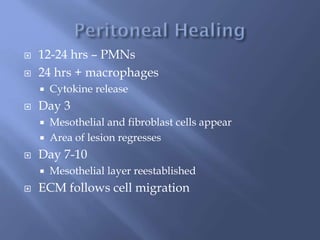
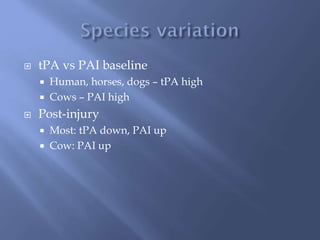
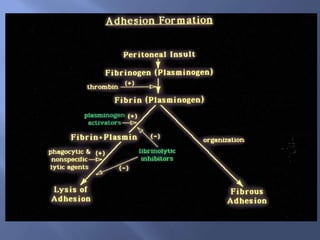
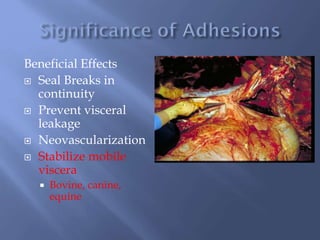
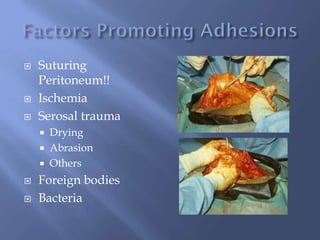
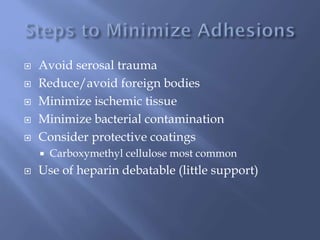
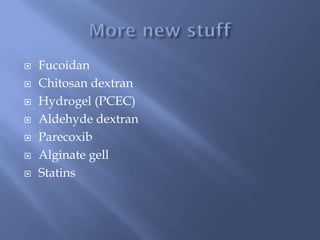
This document discusses the histology, innervation, functions, and healing process of the peritoneum. It covers the layers of the peritoneum, how it is innervated leading to pain perception, its roles in nutrient diffusion, fluid production, and waste removal. The document also summarizes the inflammatory and coagulation cascades triggered by peritoneal trauma, as well as preventative methods for reducing post-operative adhesions.