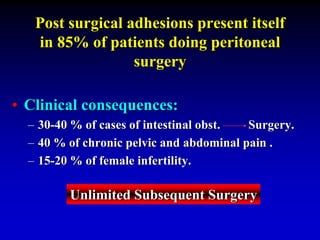
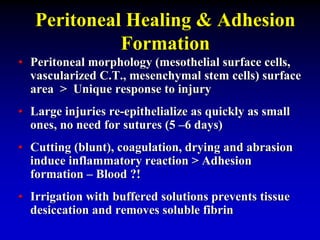
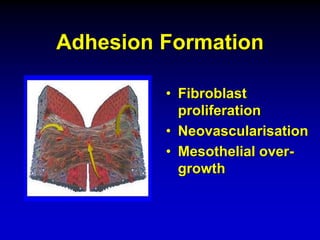
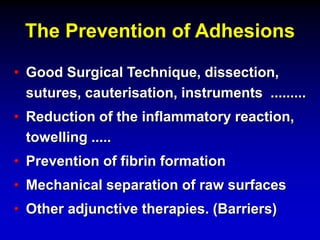
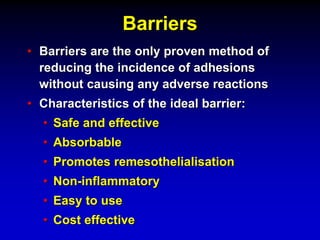
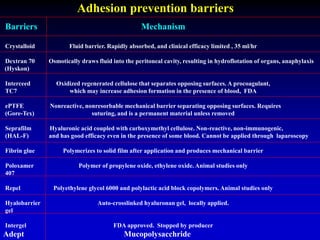
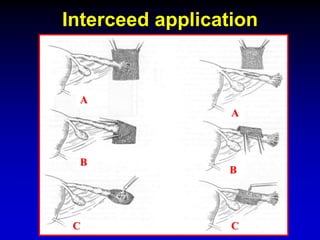
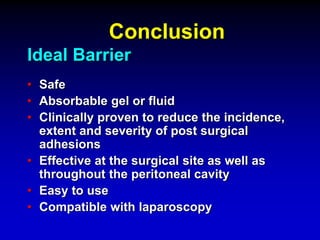
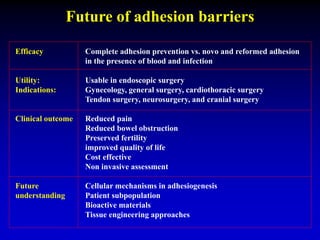
The document discusses the significant clinical consequences of peritoneal adhesions, which affect a substantial percentage of patients undergoing peritoneal surgery, leading to issues such as intestinal obstruction and infertility. It emphasizes the importance of surgical techniques and the use of barriers in preventing adhesion formation, comparing the outcomes of laparotomy and laparoscopy. The ideal adhesion prevention barriers should be safe, absorbable, and effective at reducing the incidence and severity of adhesions.