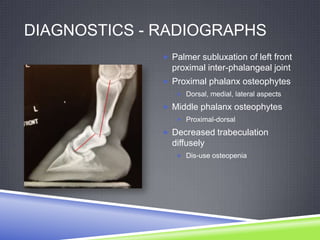
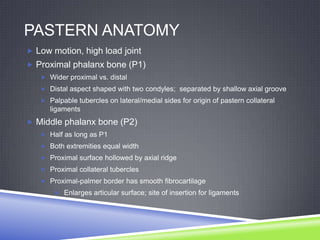
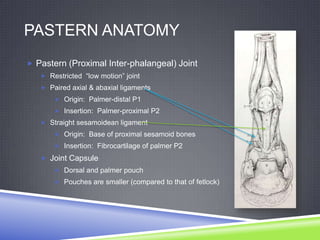
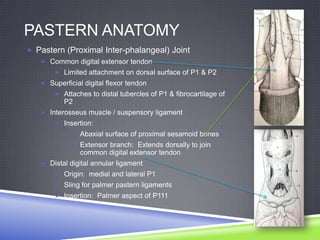
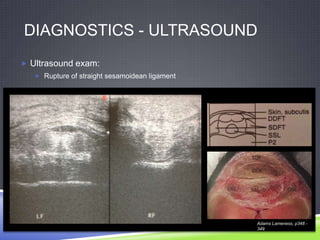
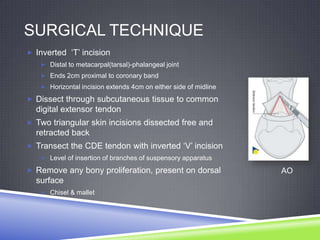
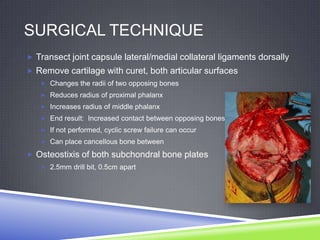
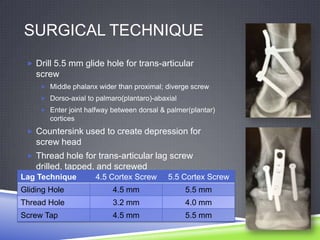
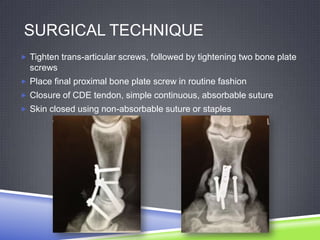
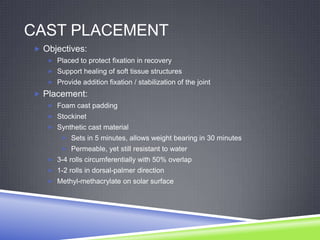
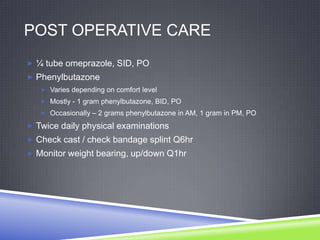
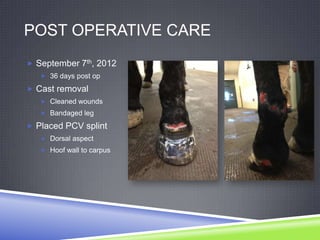
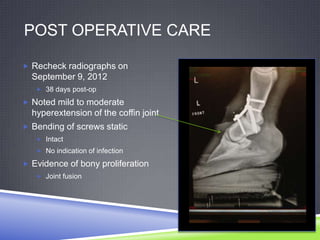
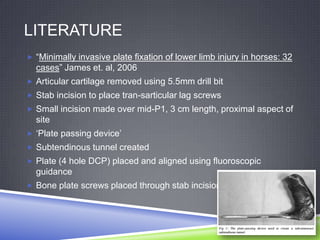
This document describes a case of pastern arthrodesis surgery performed to address a horse's chronic left forelimb lameness. It provides details on the horse's history, physical exam findings, diagnostic imaging, surgical technique, post-operative care, rehabilitation, prognosis, and relevant literature. The surgery involved removing cartilage from the pastern joint, placing a plate with screws dorsally, and inserting two lag screws transarticularly to fuse the joint. The horse's recovery and long-term prognosis after pastern fusion are discussed.