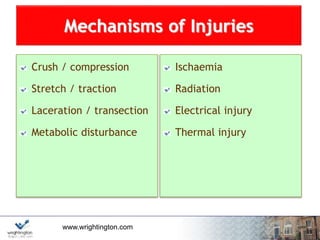
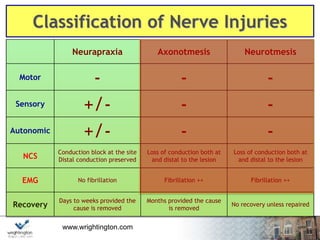
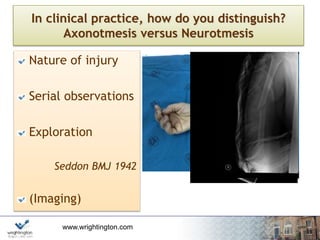
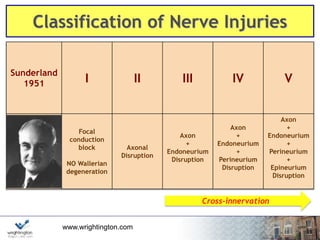
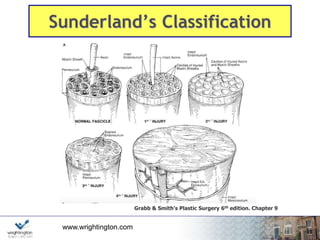
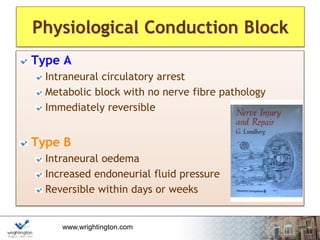
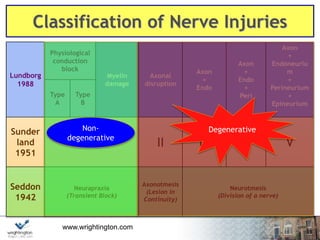
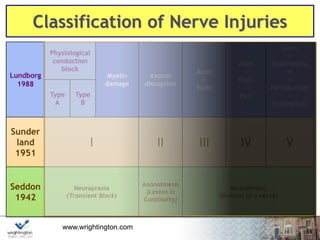
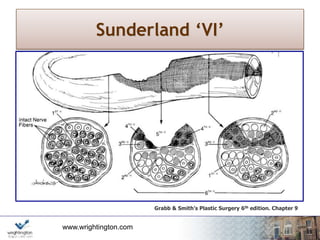
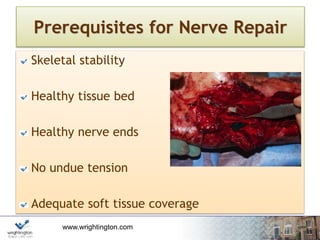
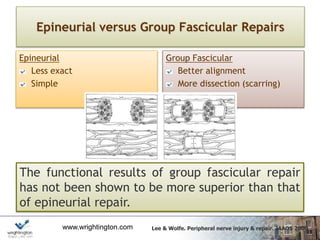
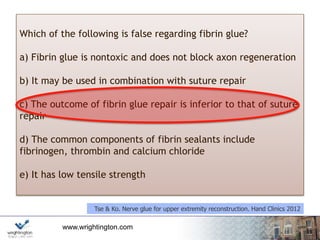
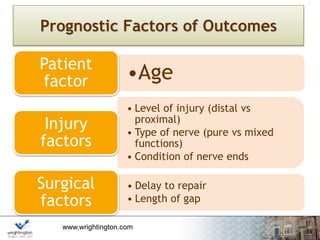
This document discusses peripheral nerve injuries. It begins with an overview and classifications of nerve injuries including Seddon and Sunderland systems. Principles of nerve surgery such as neurolysis and nerve repair are covered. Factors that influence nerve regeneration like age, injury level and surgical delay are addressed. The document concludes with details on the peripheral nerve injury service contact information.