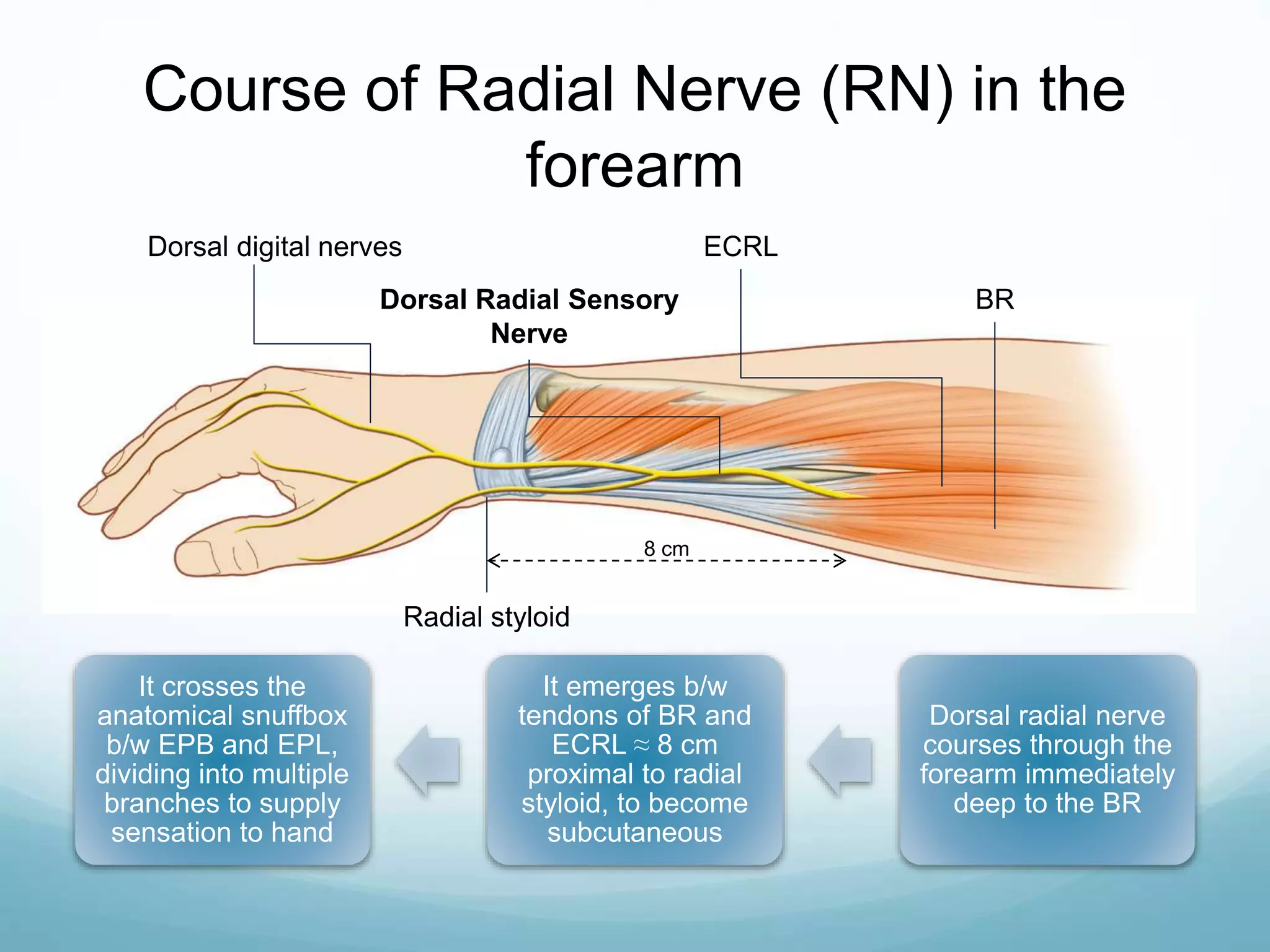
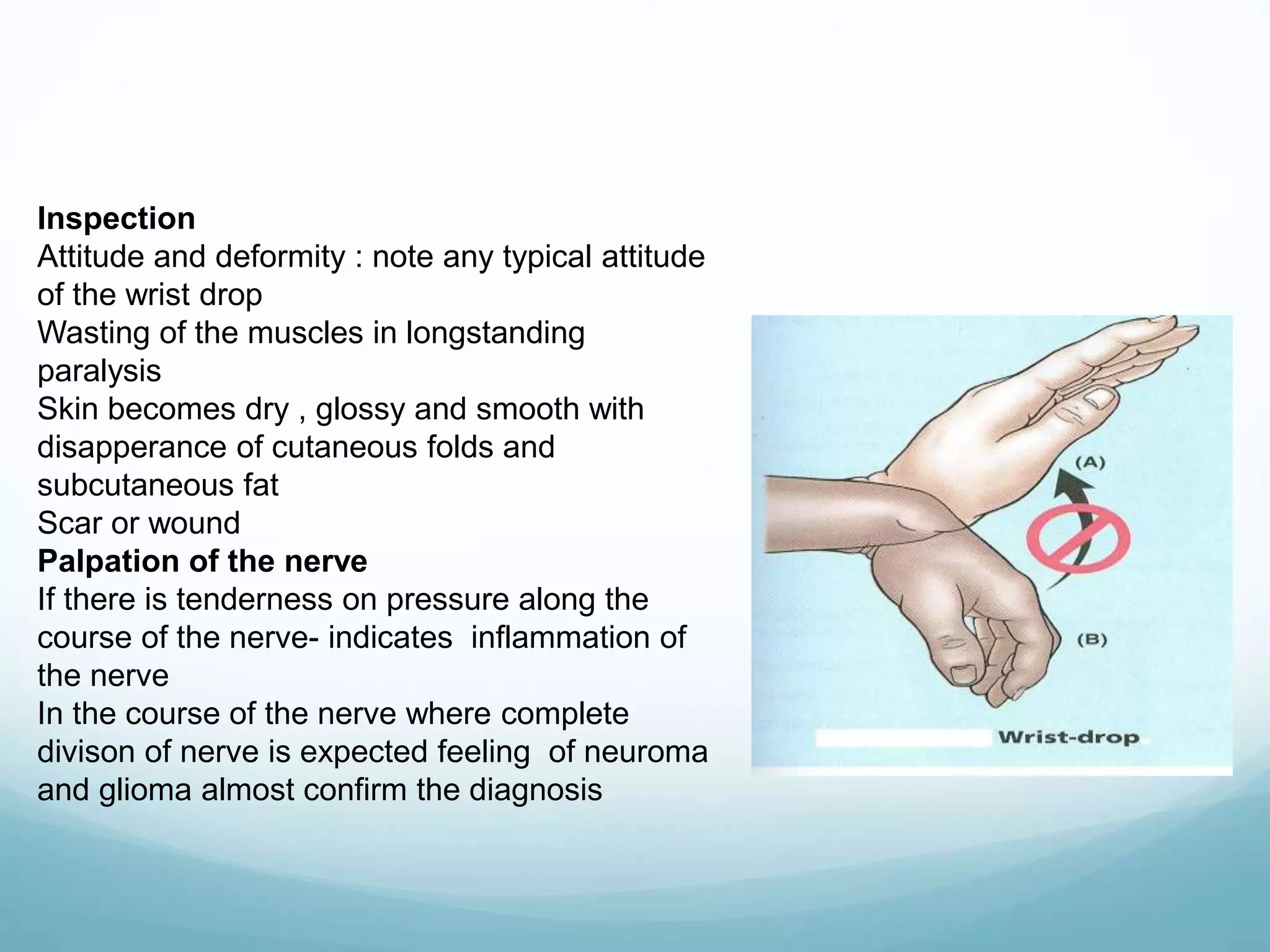
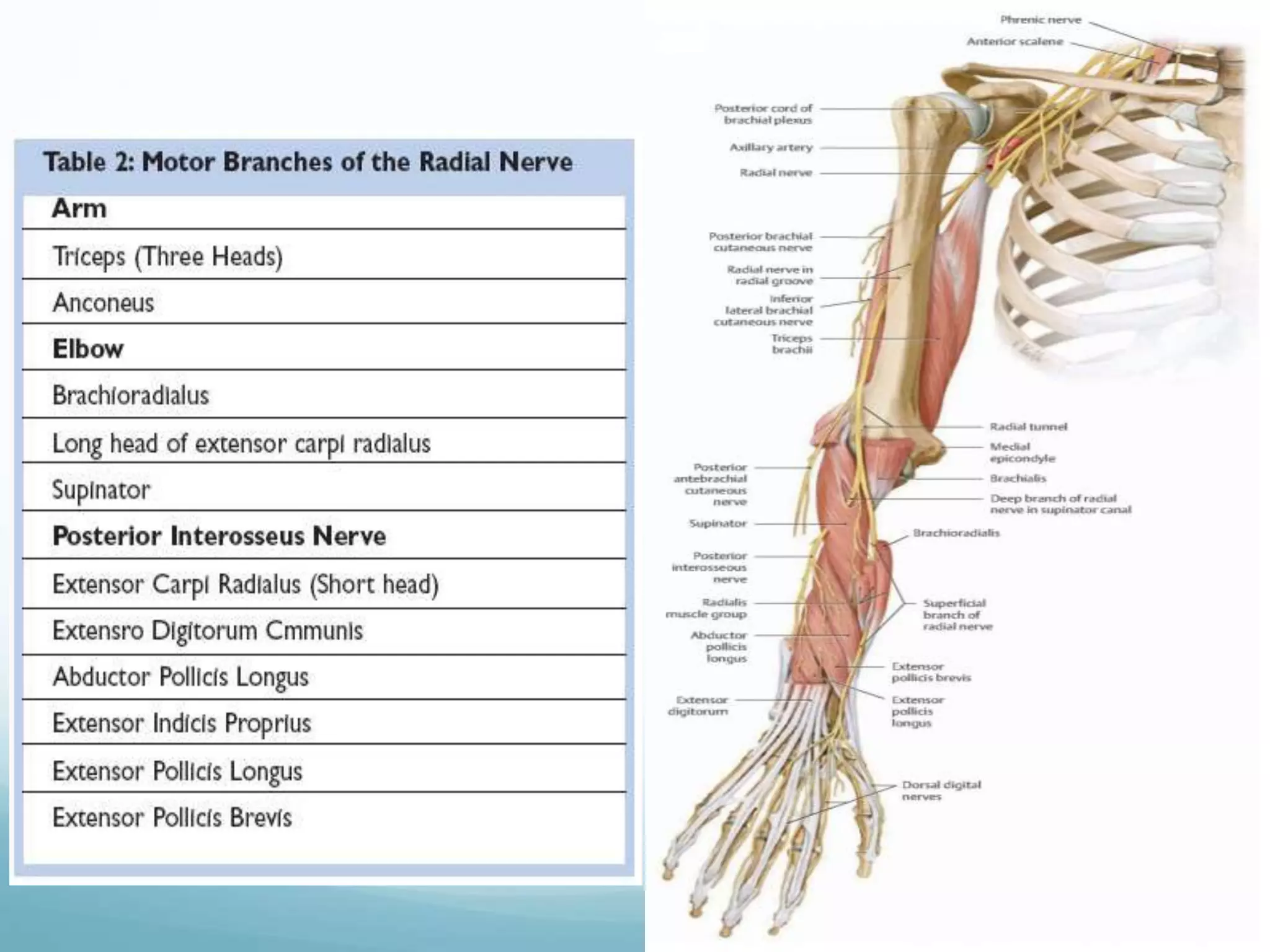
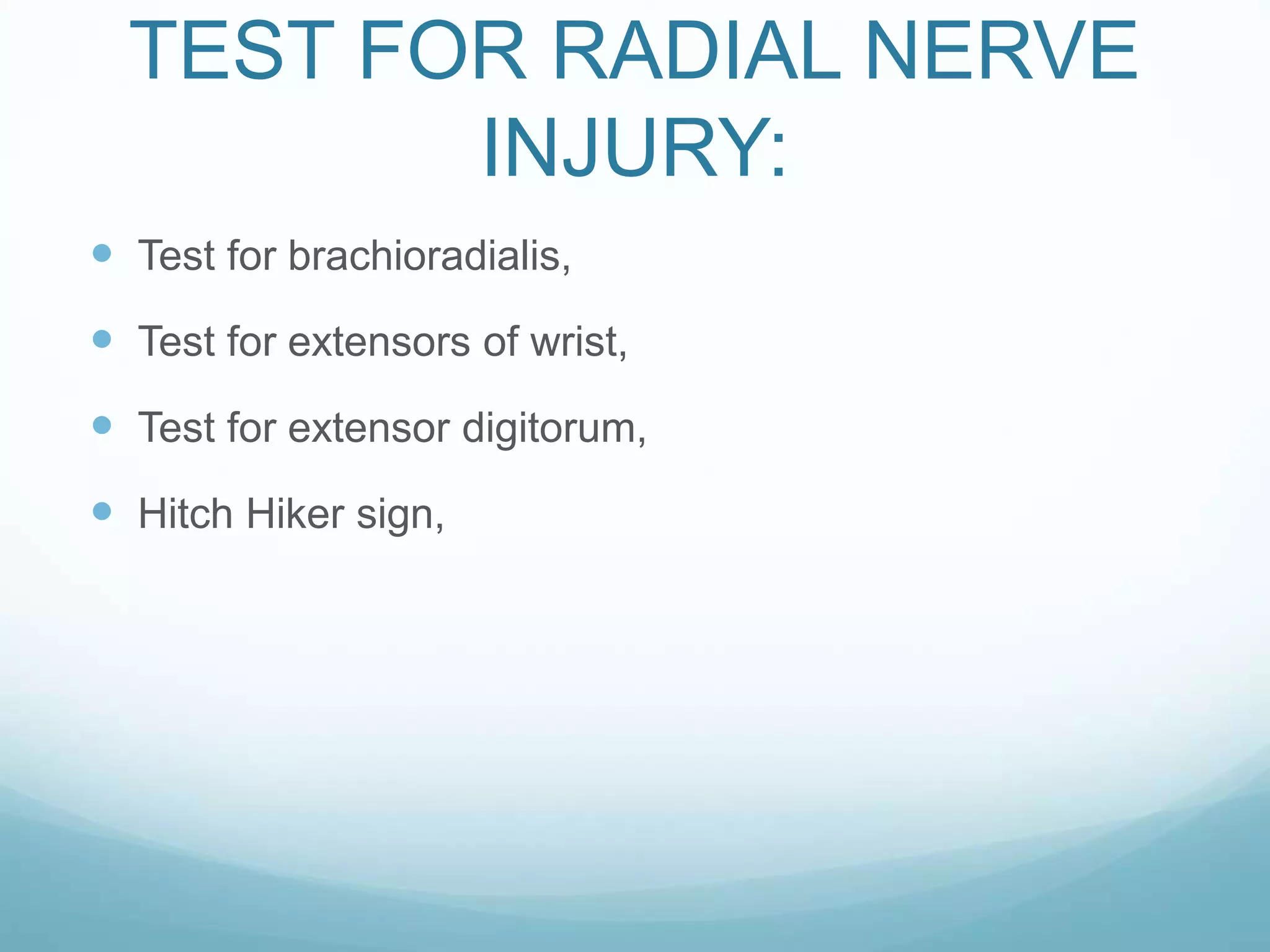
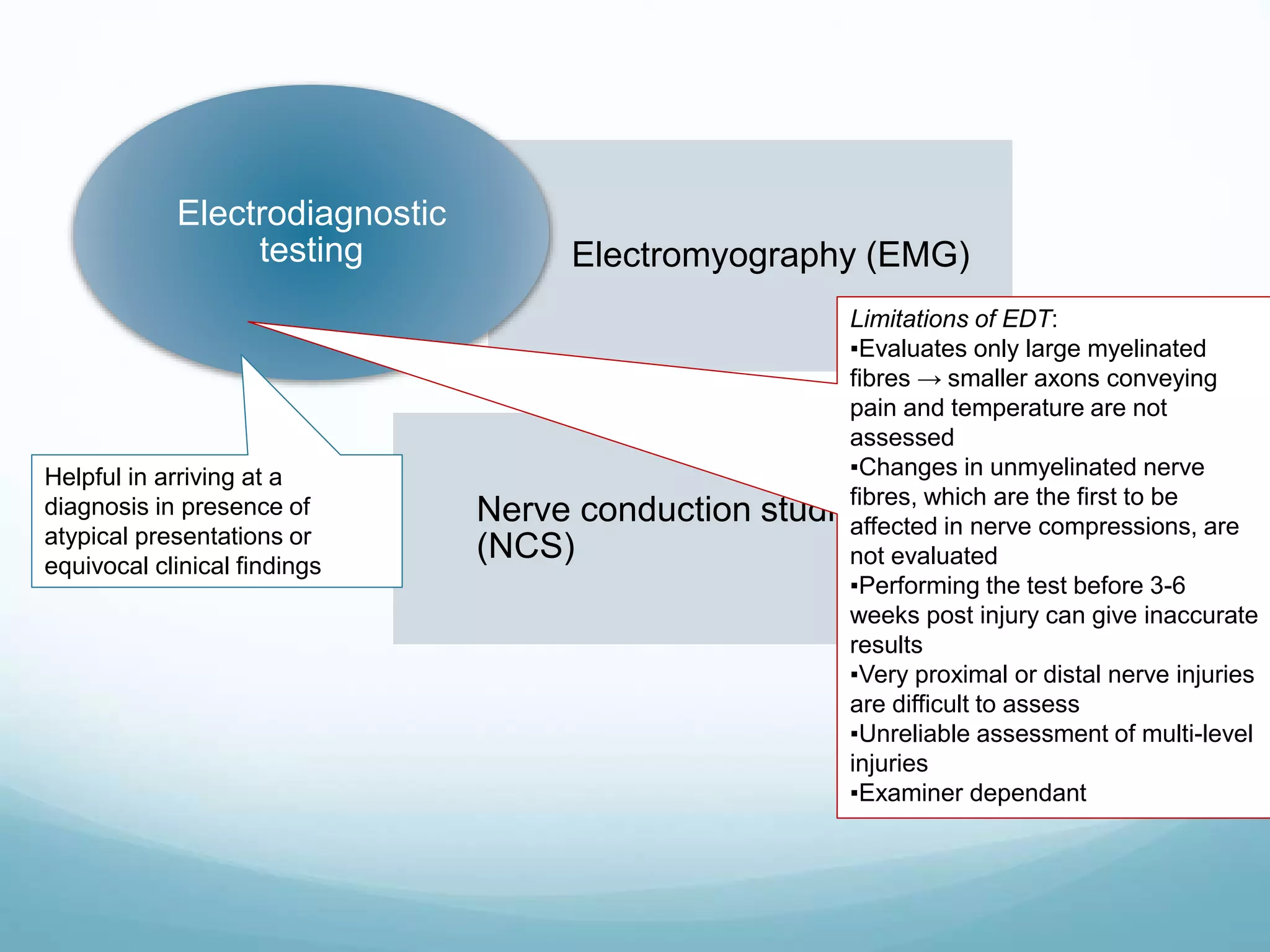
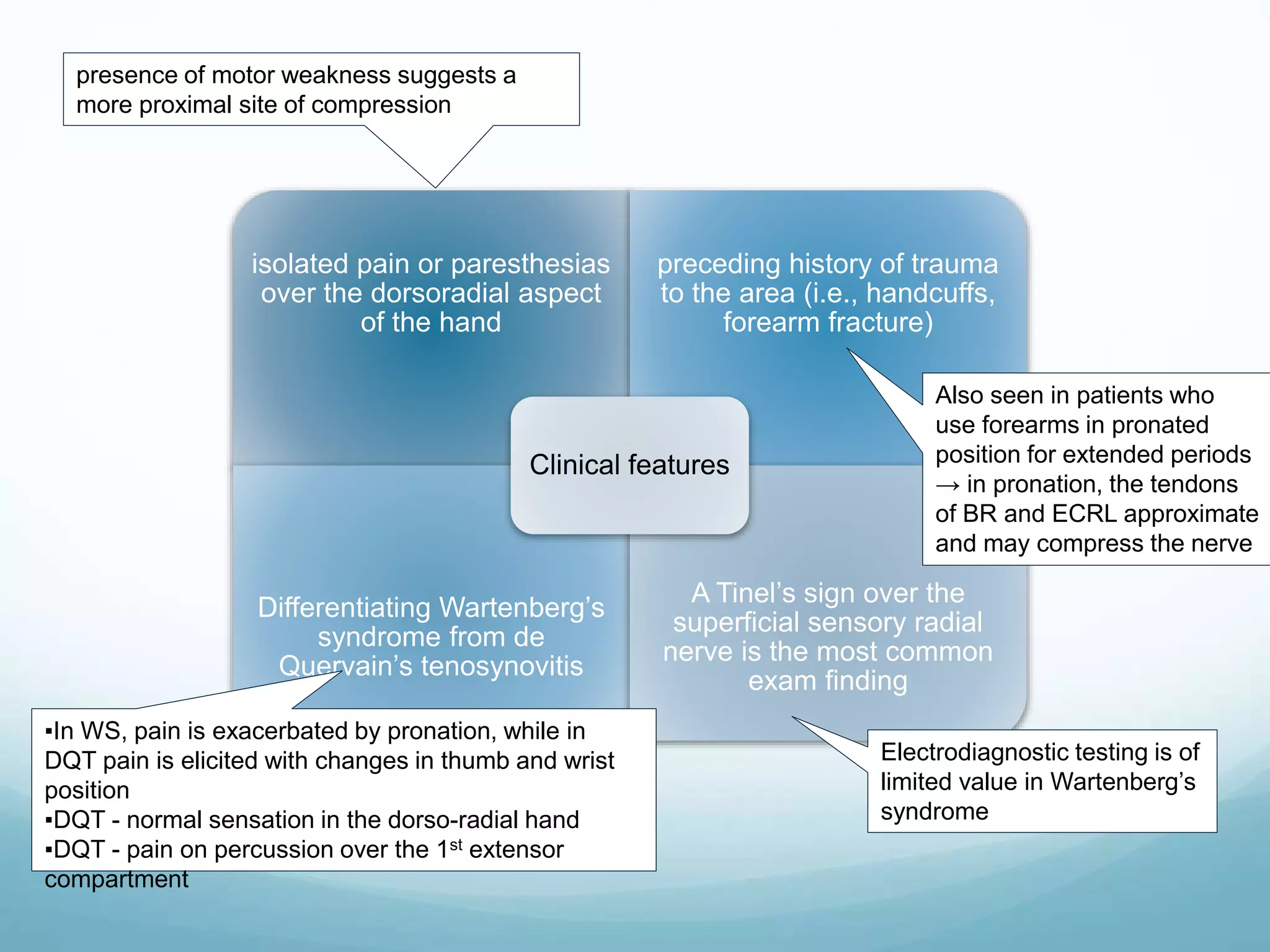
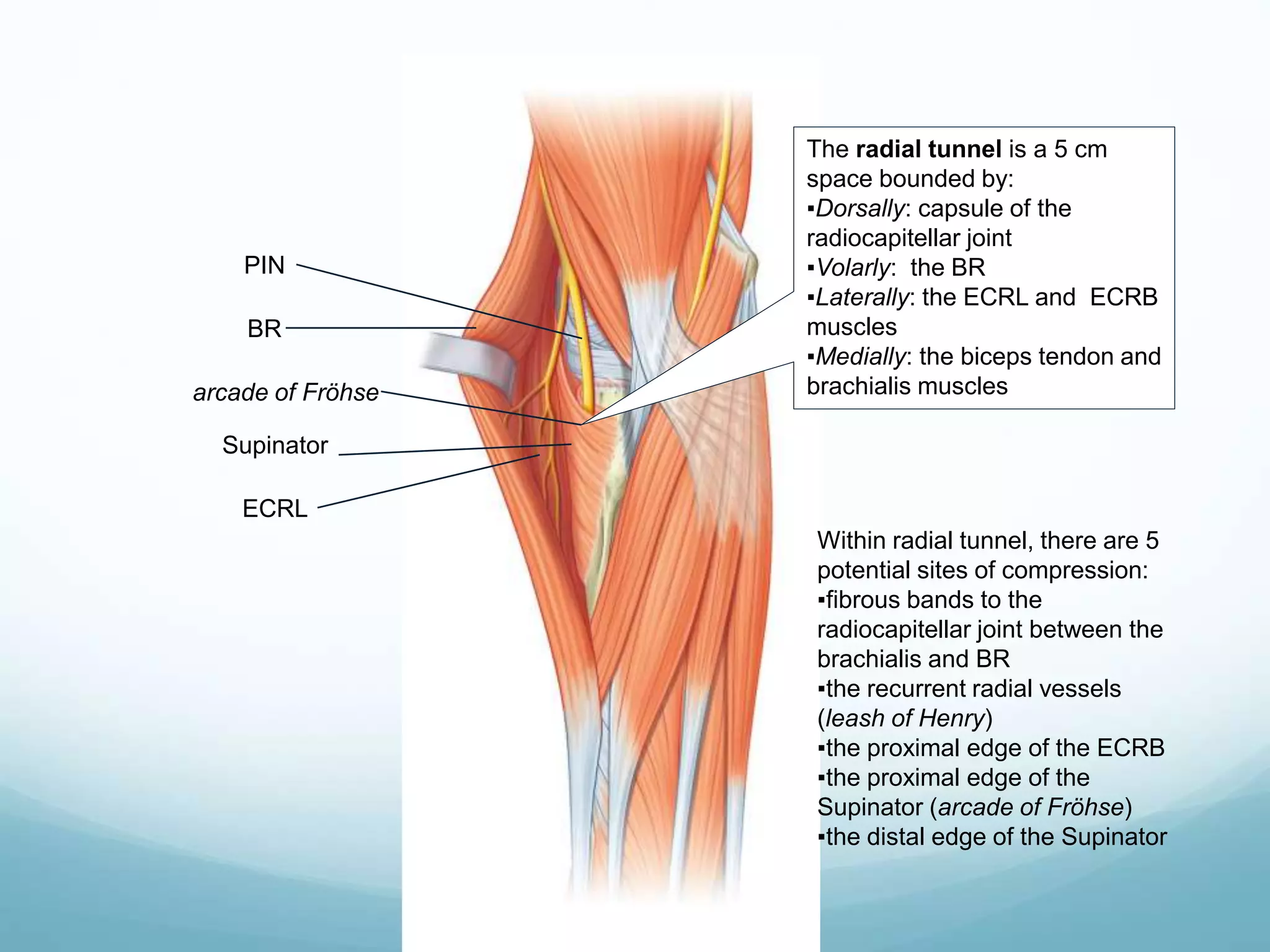
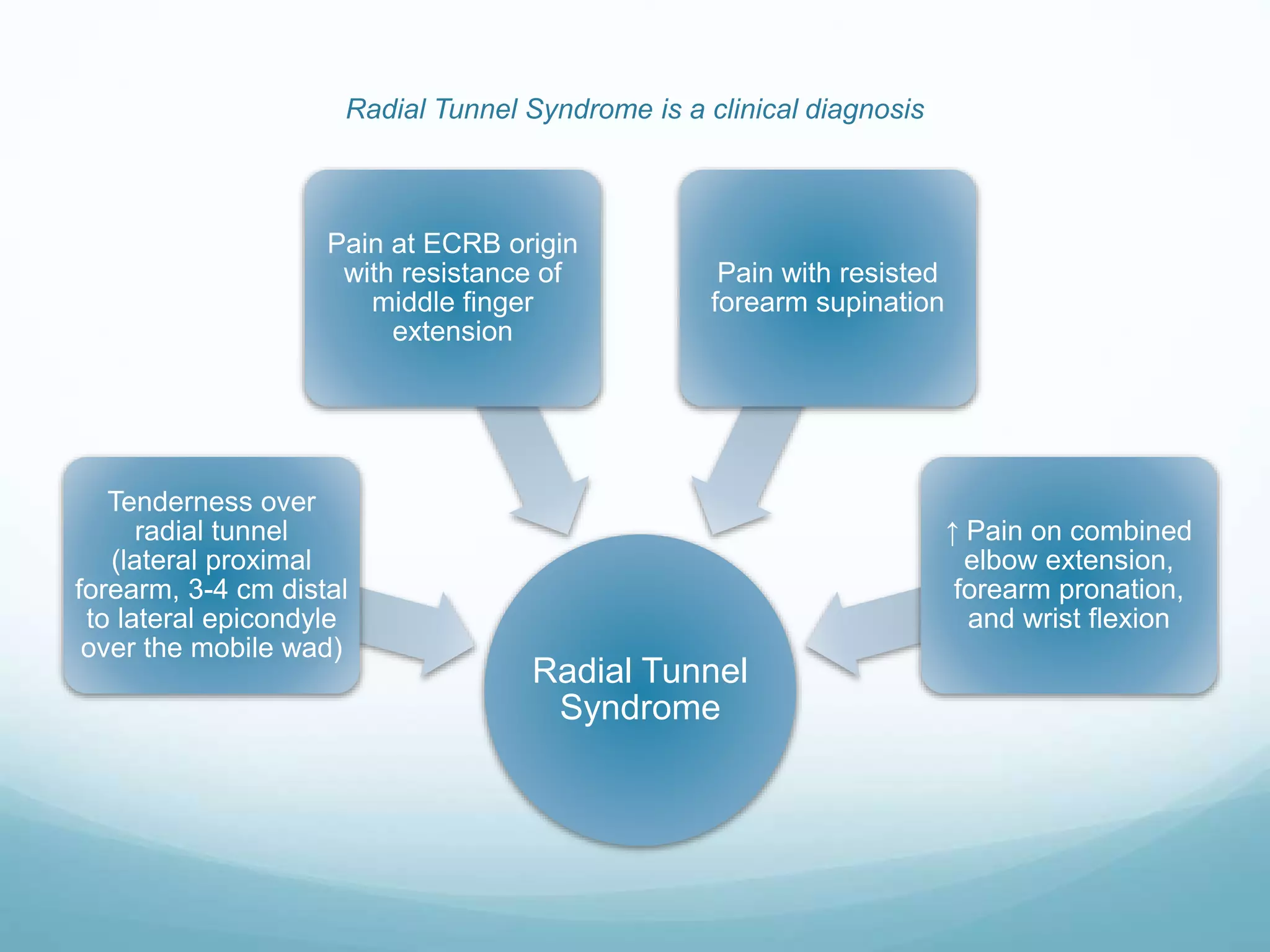
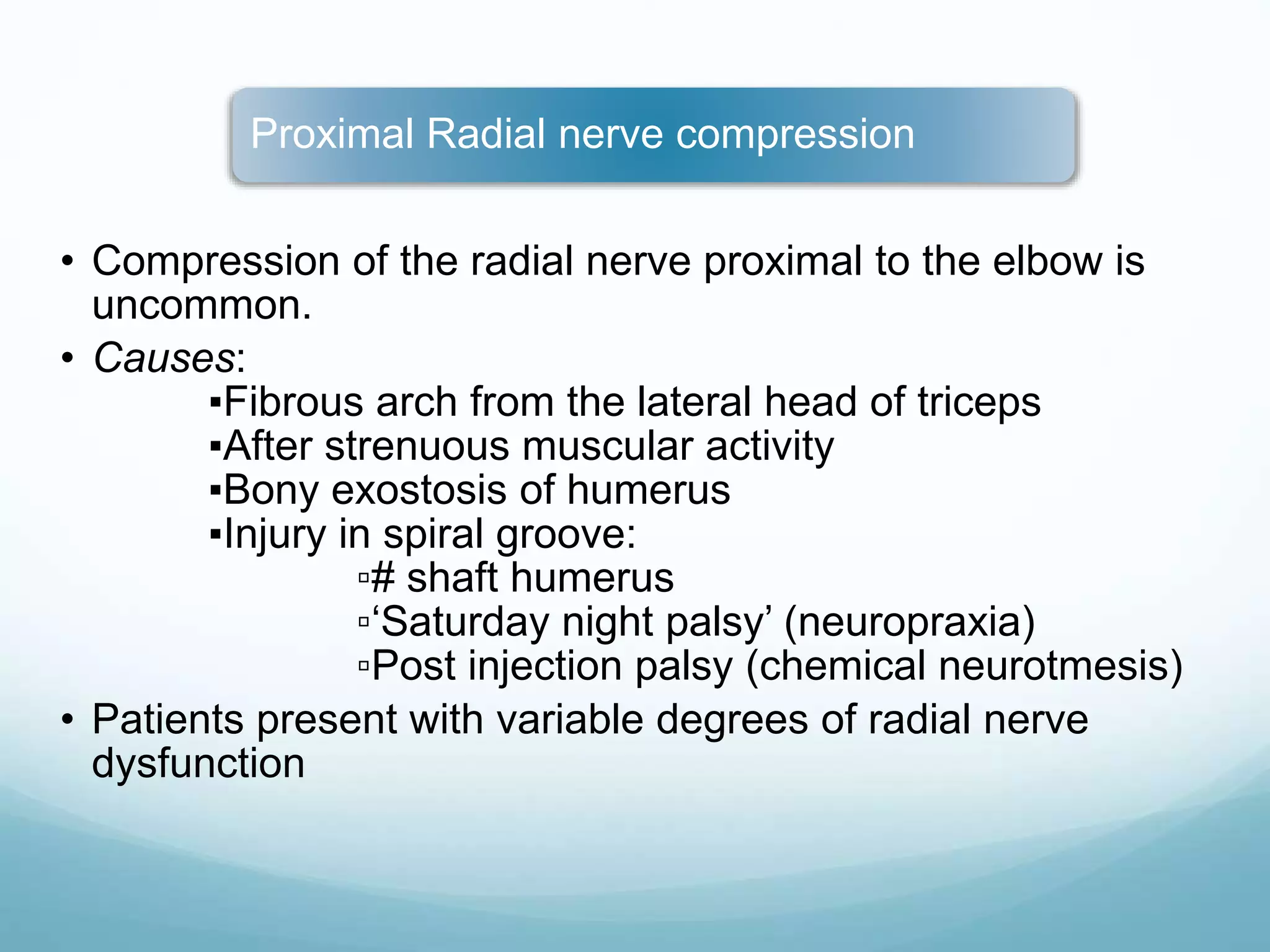
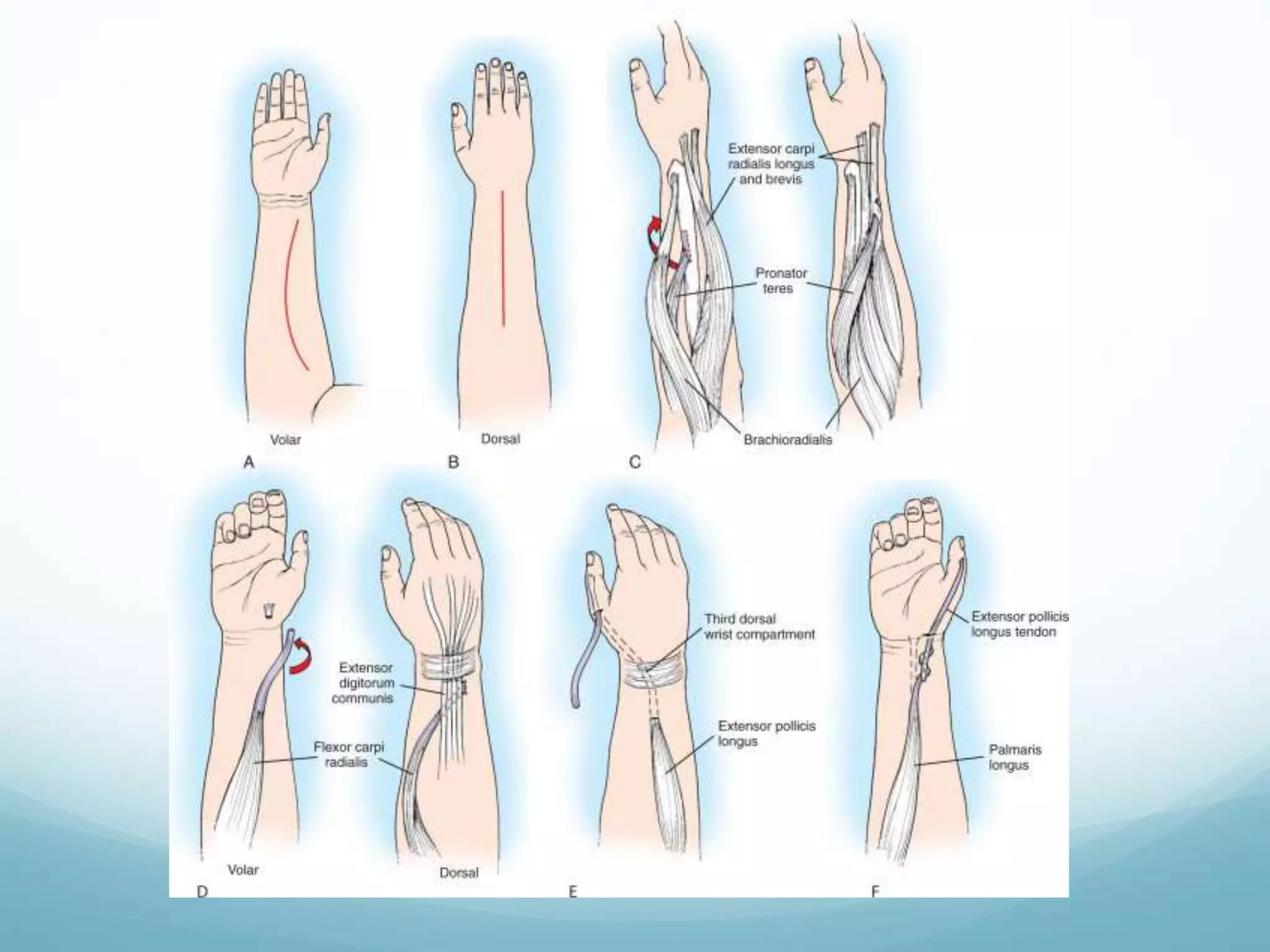
This document discusses radial nerve injury and management. It begins with the anatomy of the radial nerve, describing its course from the posterior cord through the arm, forearm, and hand. It then covers the etiology, types, clinical features, diagnostic tests, and electrophysiological evaluation of radial nerve injuries at different levels. Specific conditions involving radial nerve compression are also explained, such as Wartenberg's syndrome and posterior interosseous nerve syndrome. The document provides a comprehensive overview of radial nerve anatomy and the clinical assessment and management of various radial nerve injuries.