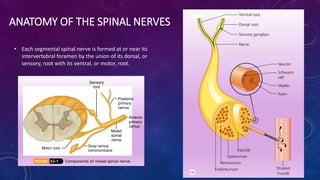
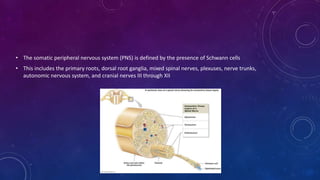
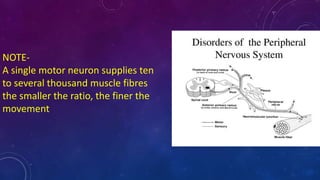
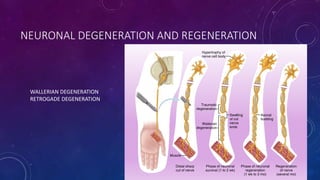
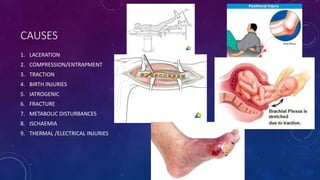
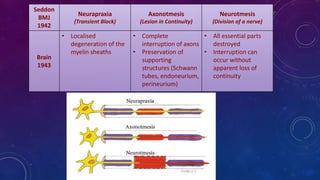
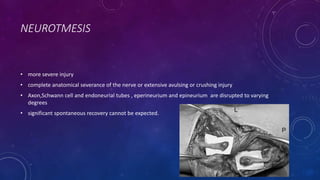
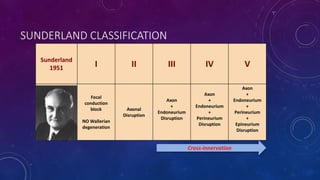
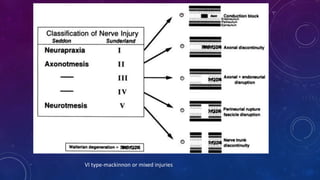
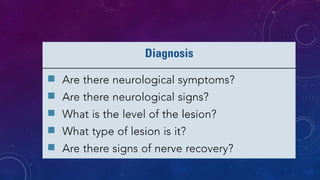
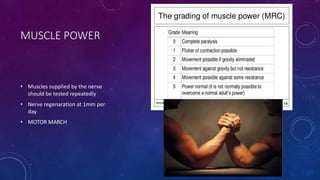
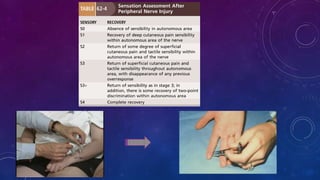
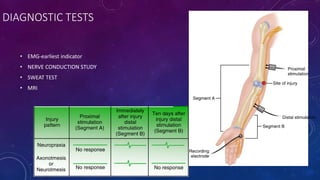
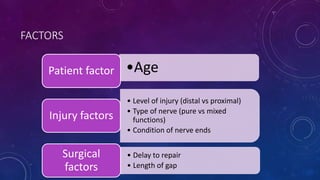
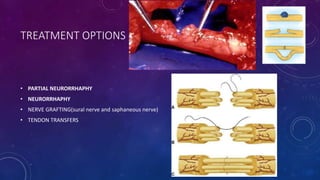
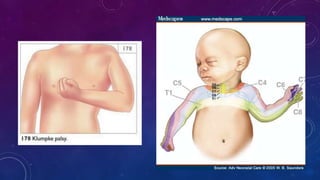
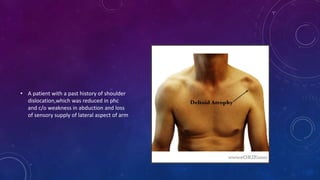
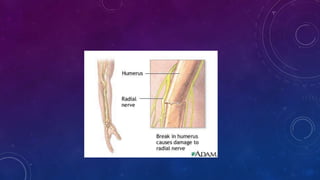
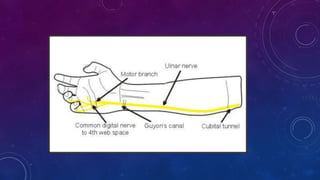
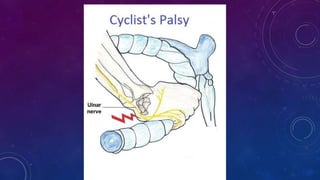
This document summarizes peripheral nerve injuries. It describes the anatomy of spinal nerves and their components. It discusses the types of nerve injuries including neurapraxia, axonotmesis, and neurotmesis. Common sites of injury in the upper and lower limbs are provided. The stages of nerve injury and recovery are outlined. Methods of diagnosing nerve injuries through examination, tests like EMG and NCS, and imaging are presented. Surgical and non-surgical treatment options are summarized along with factors that influence recovery.