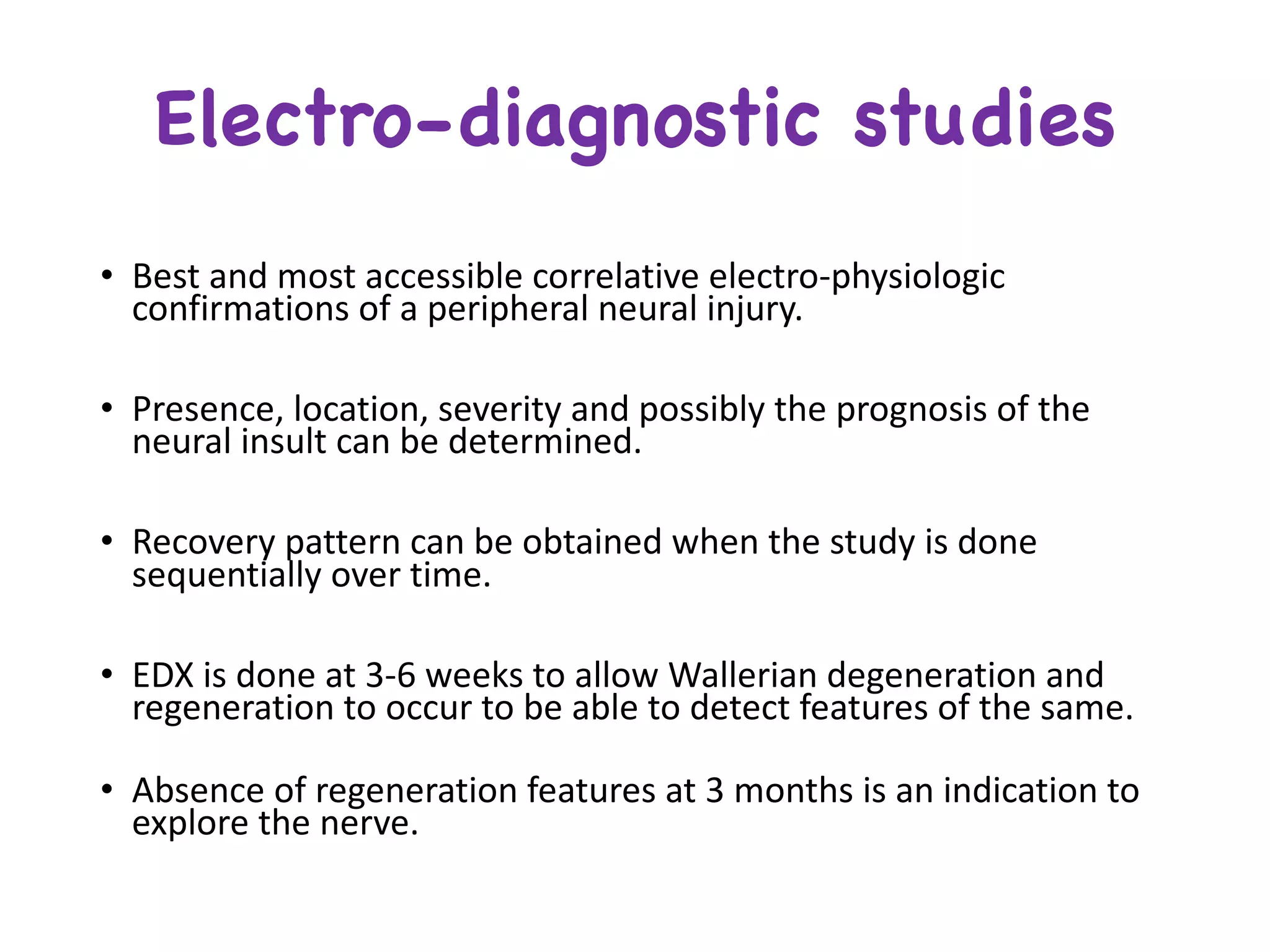
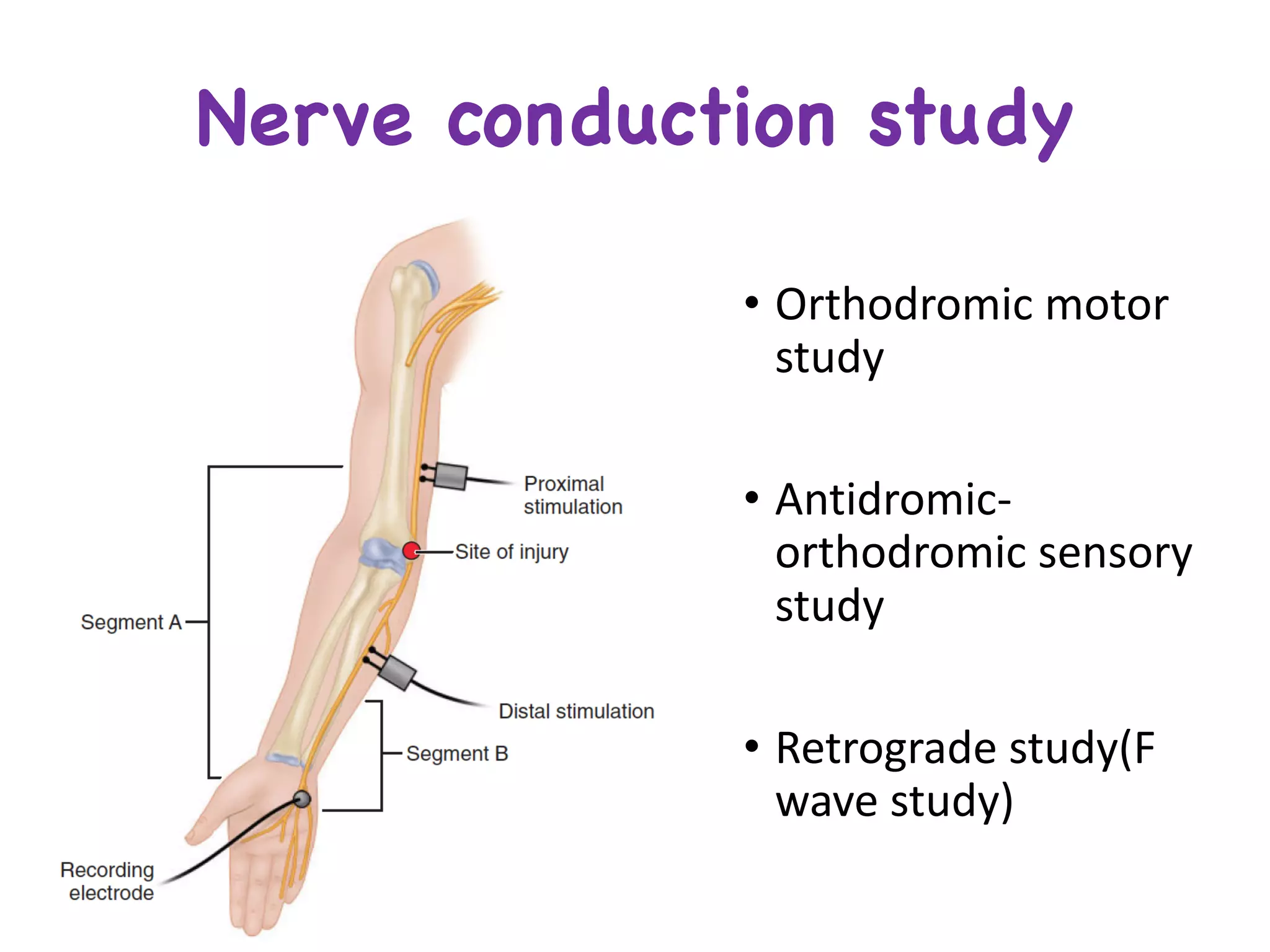
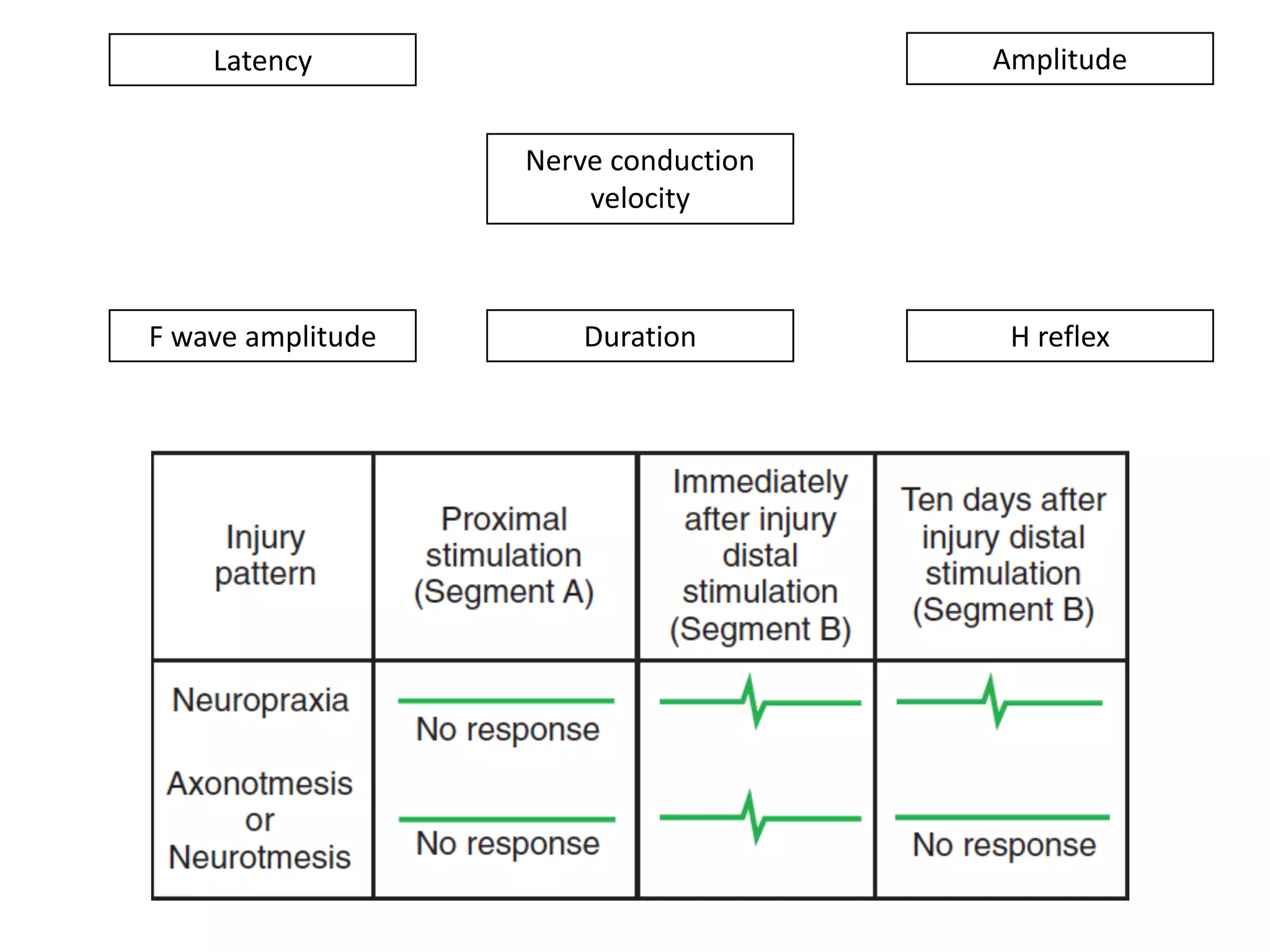
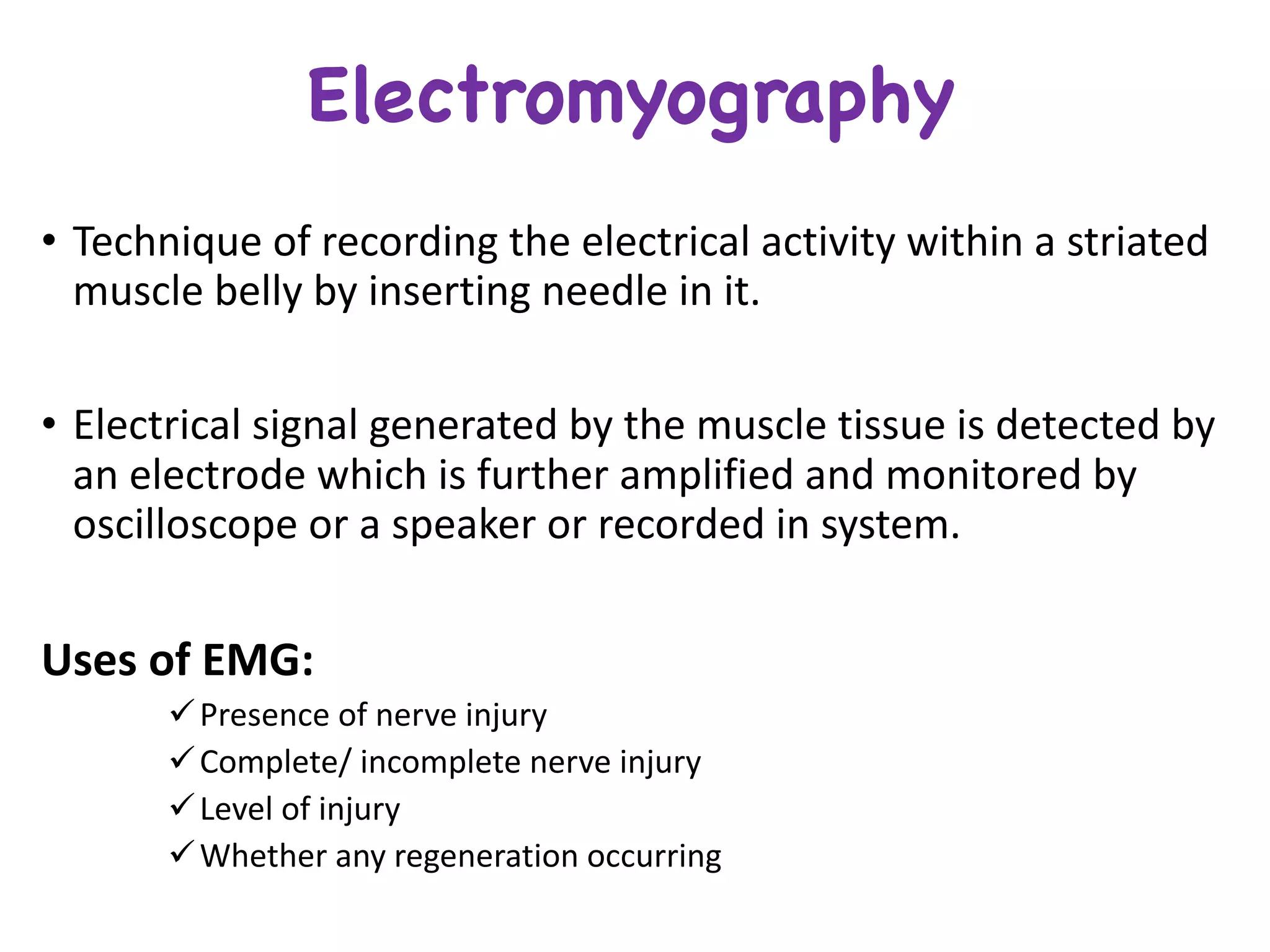
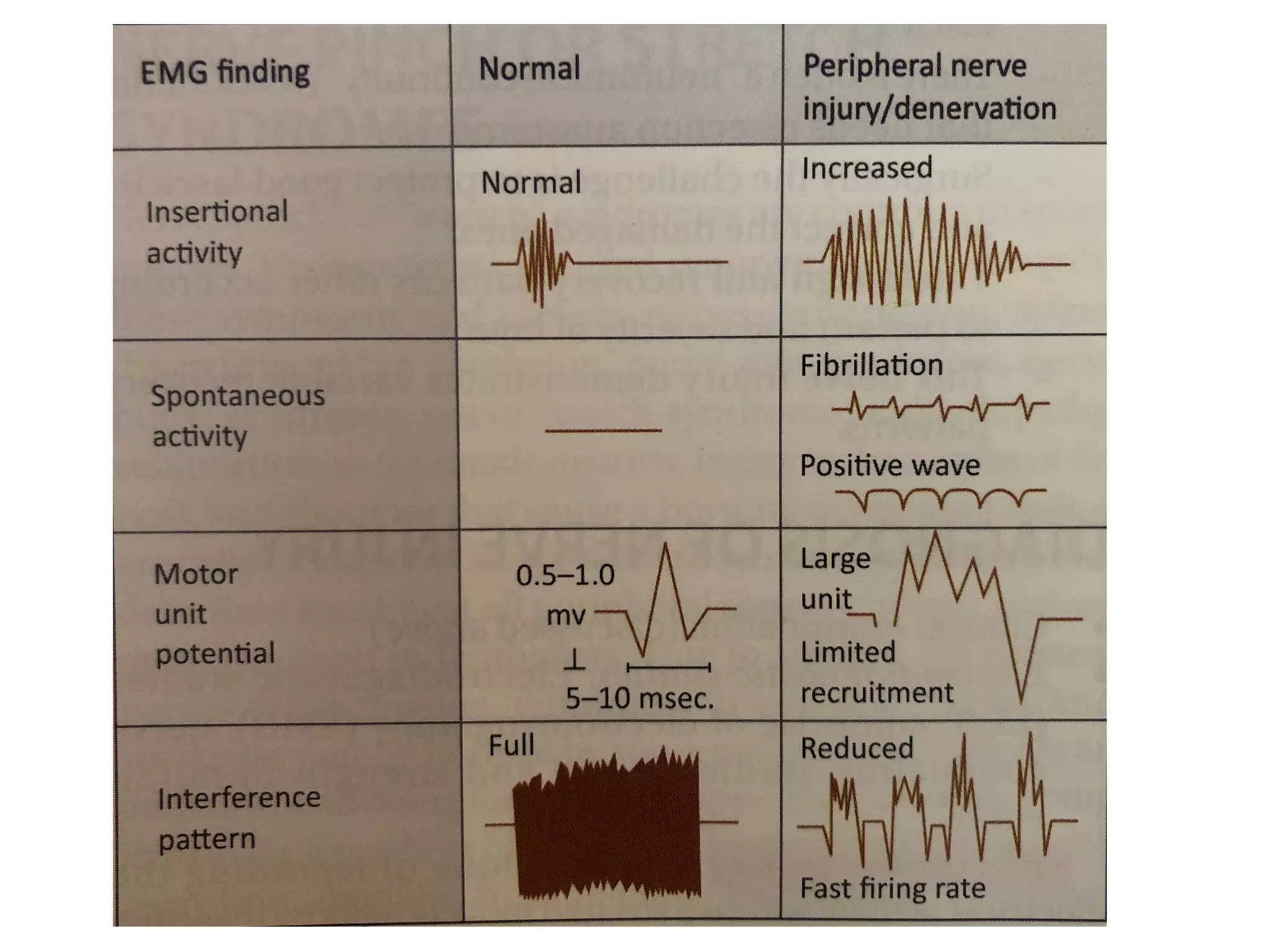
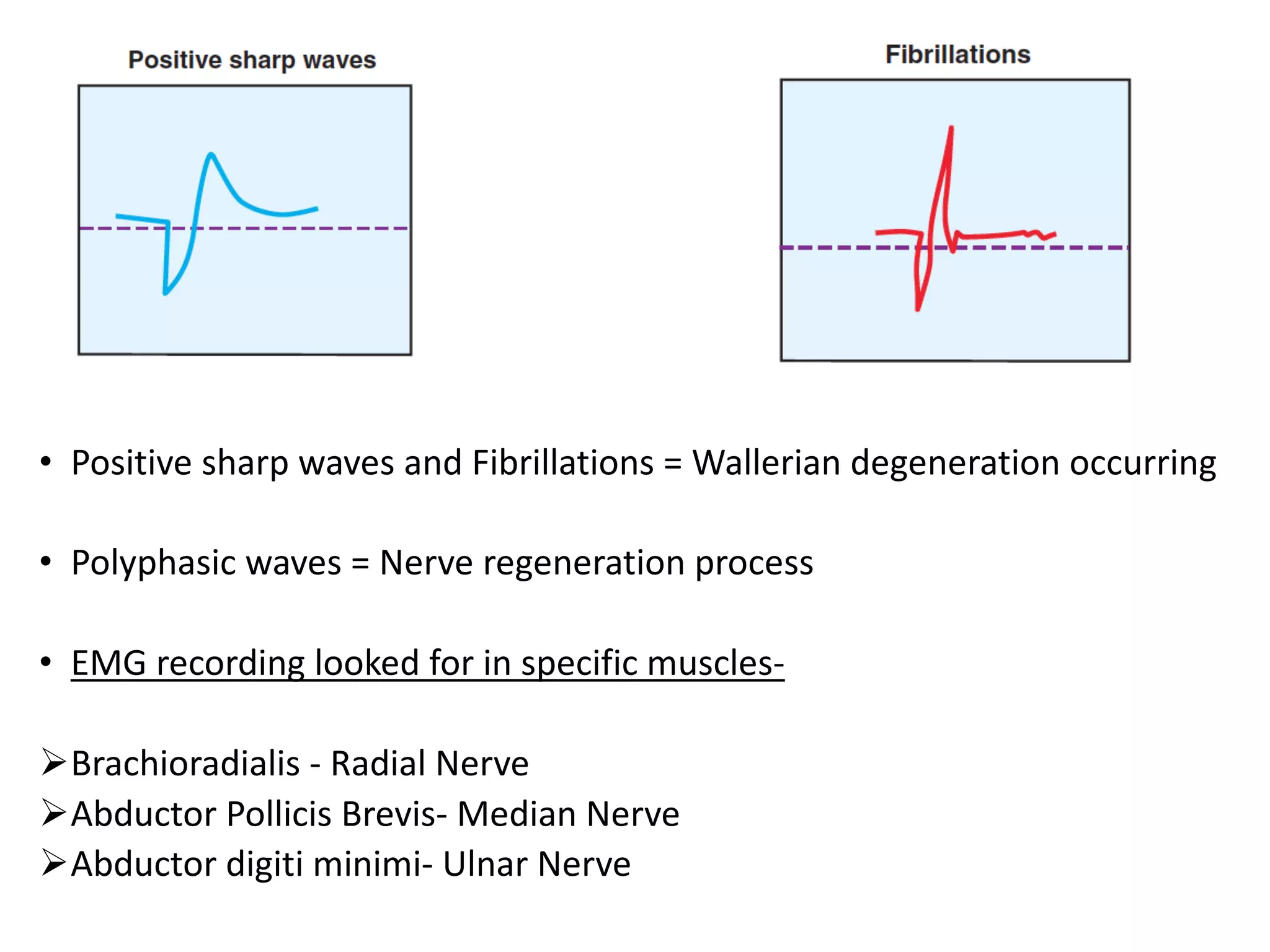
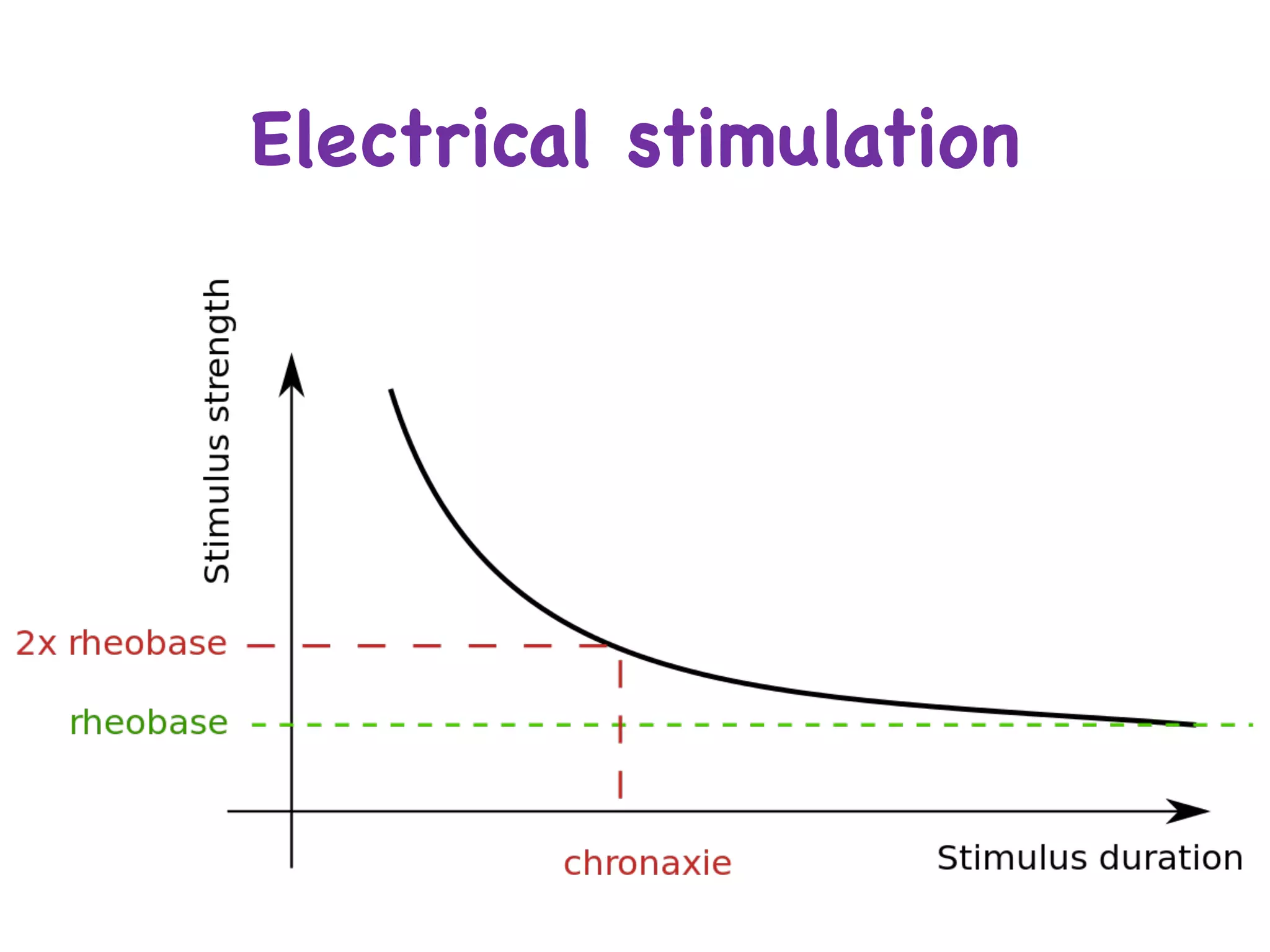
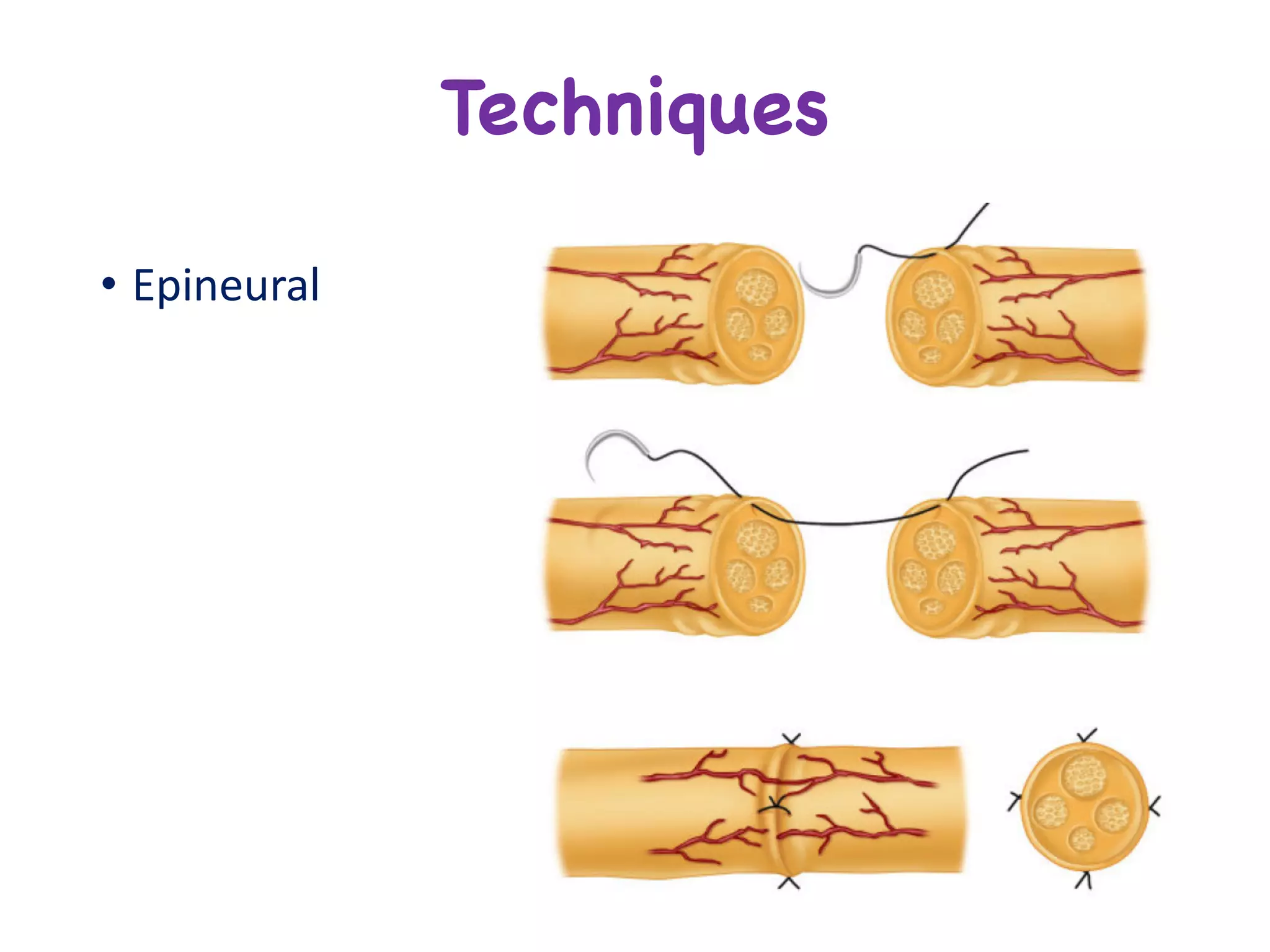
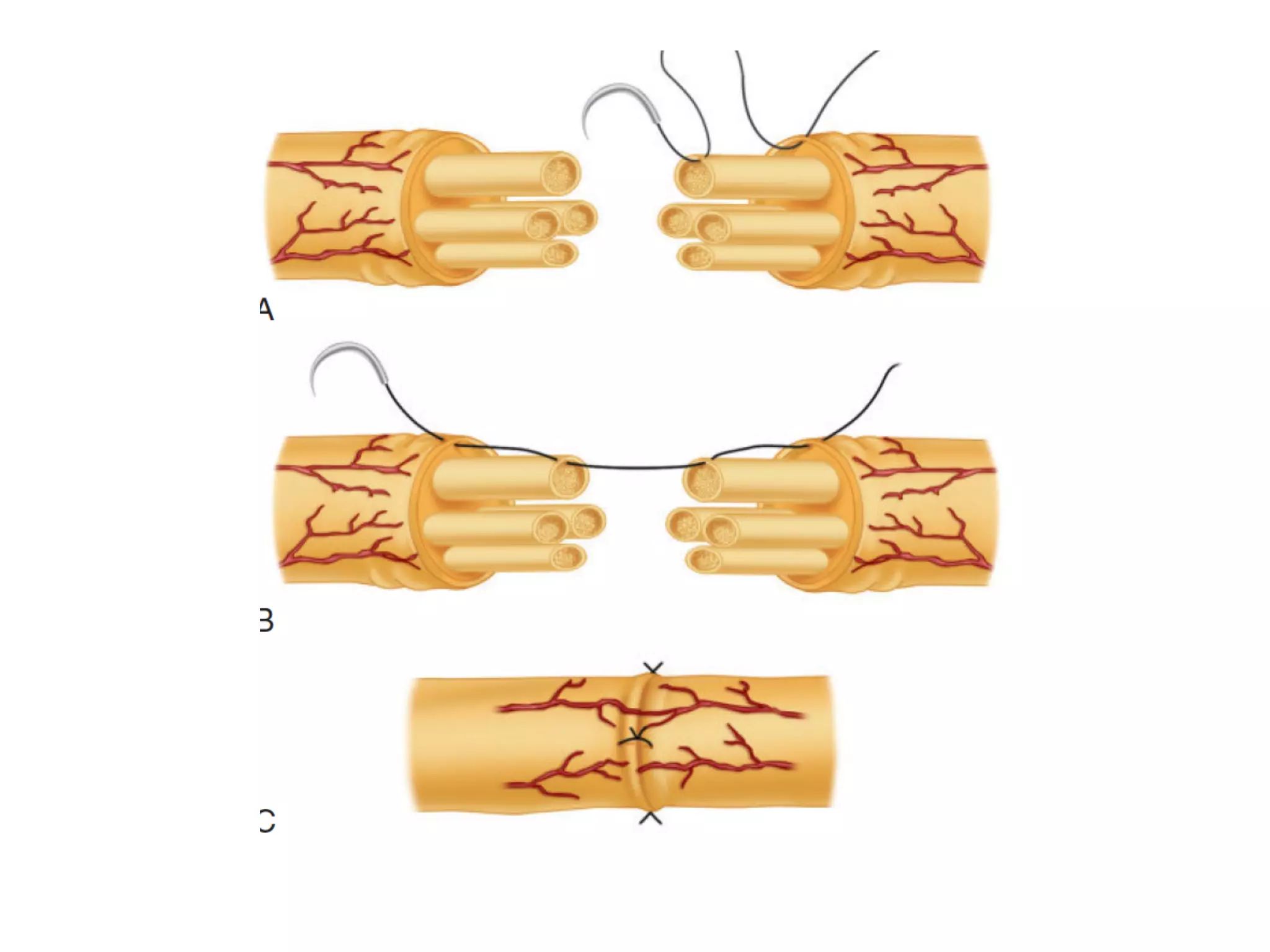
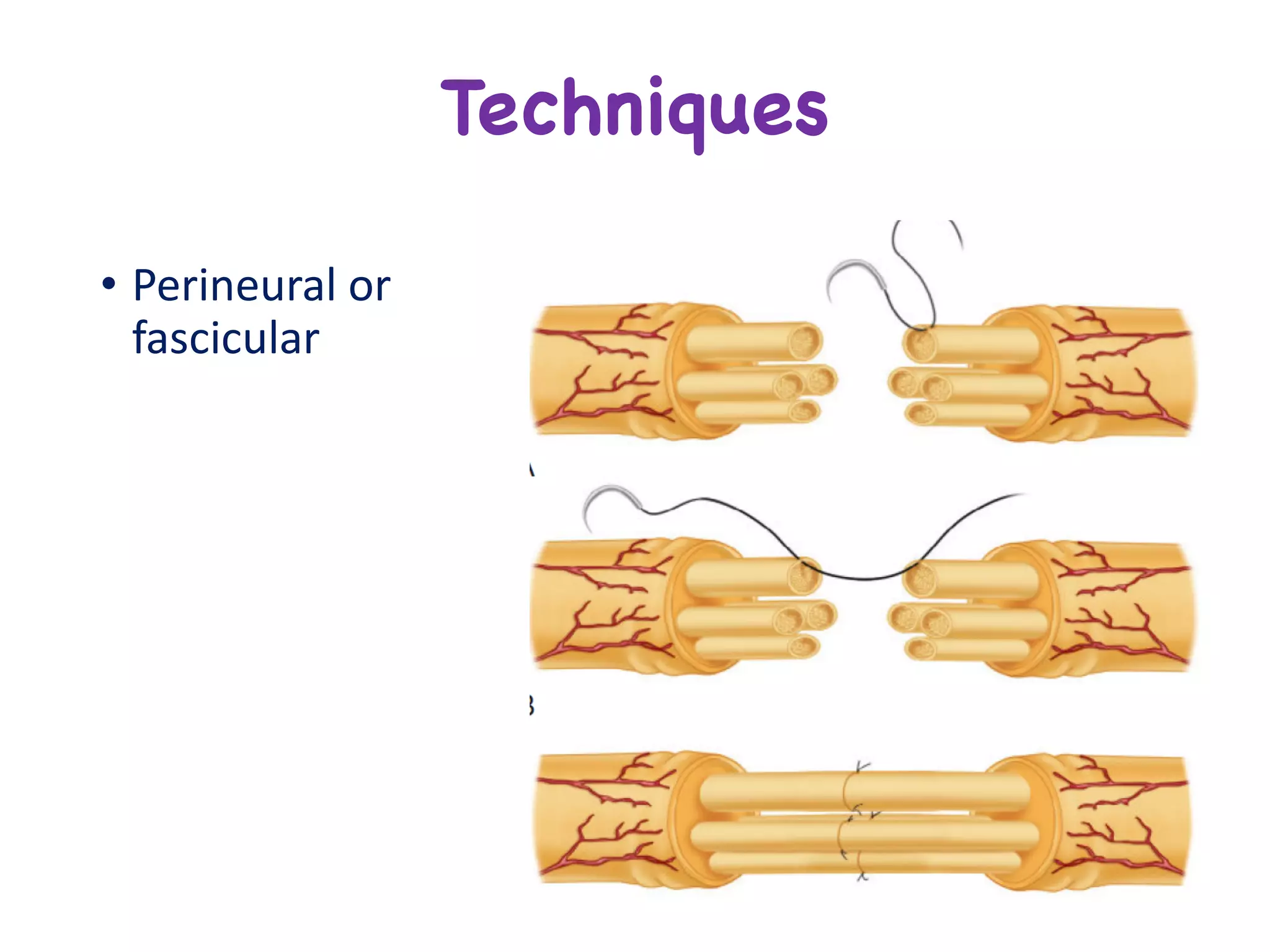
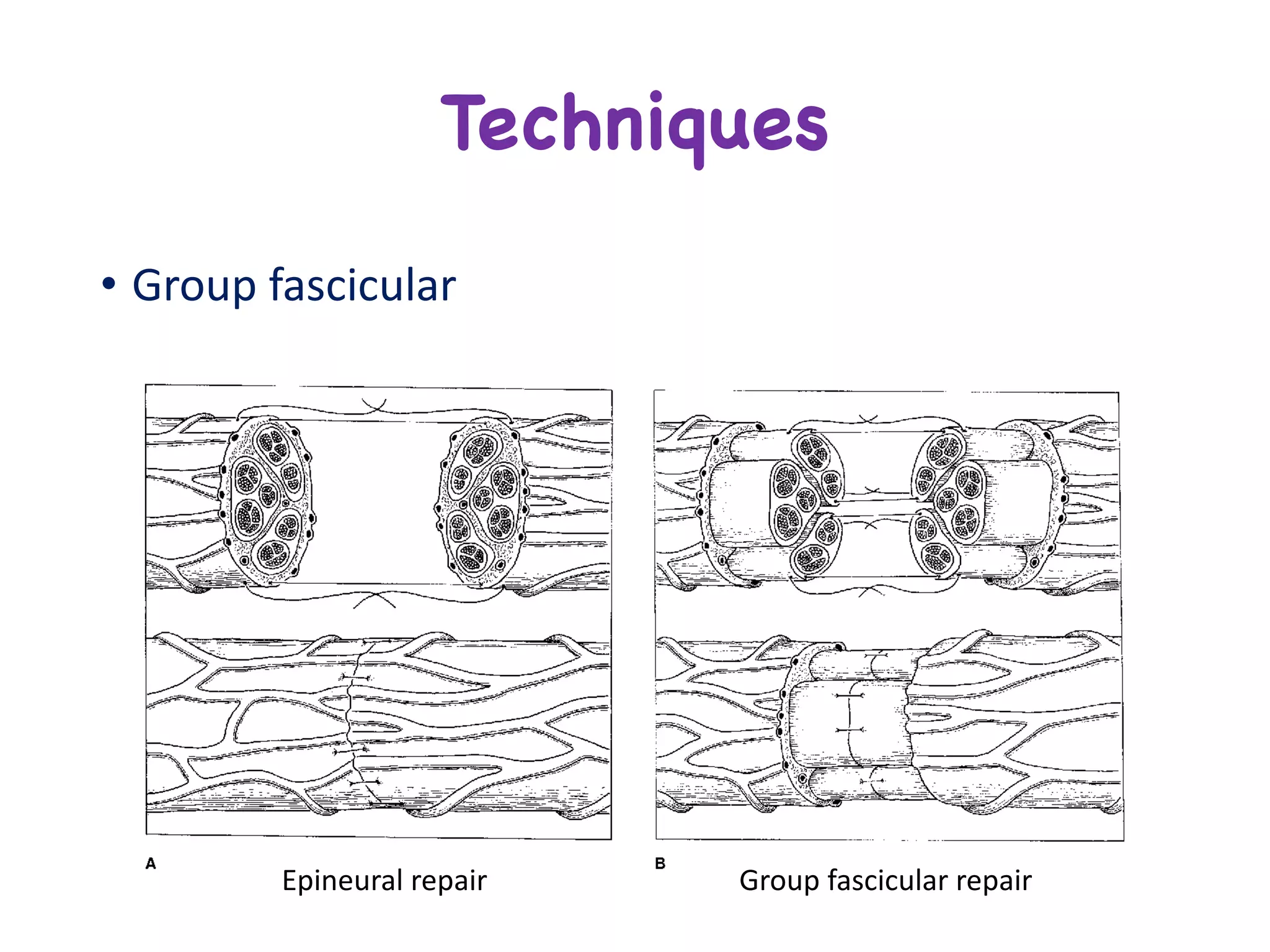
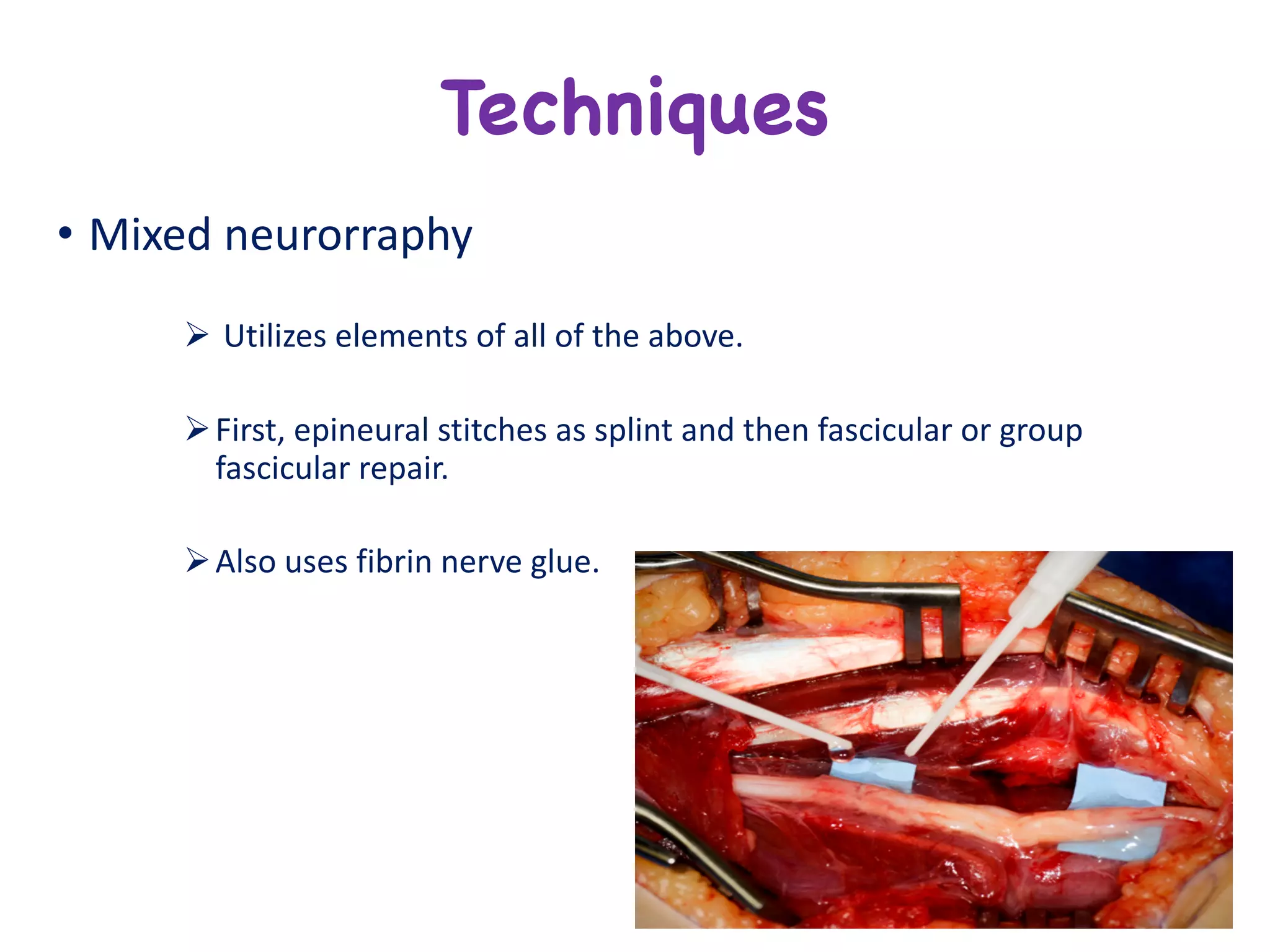
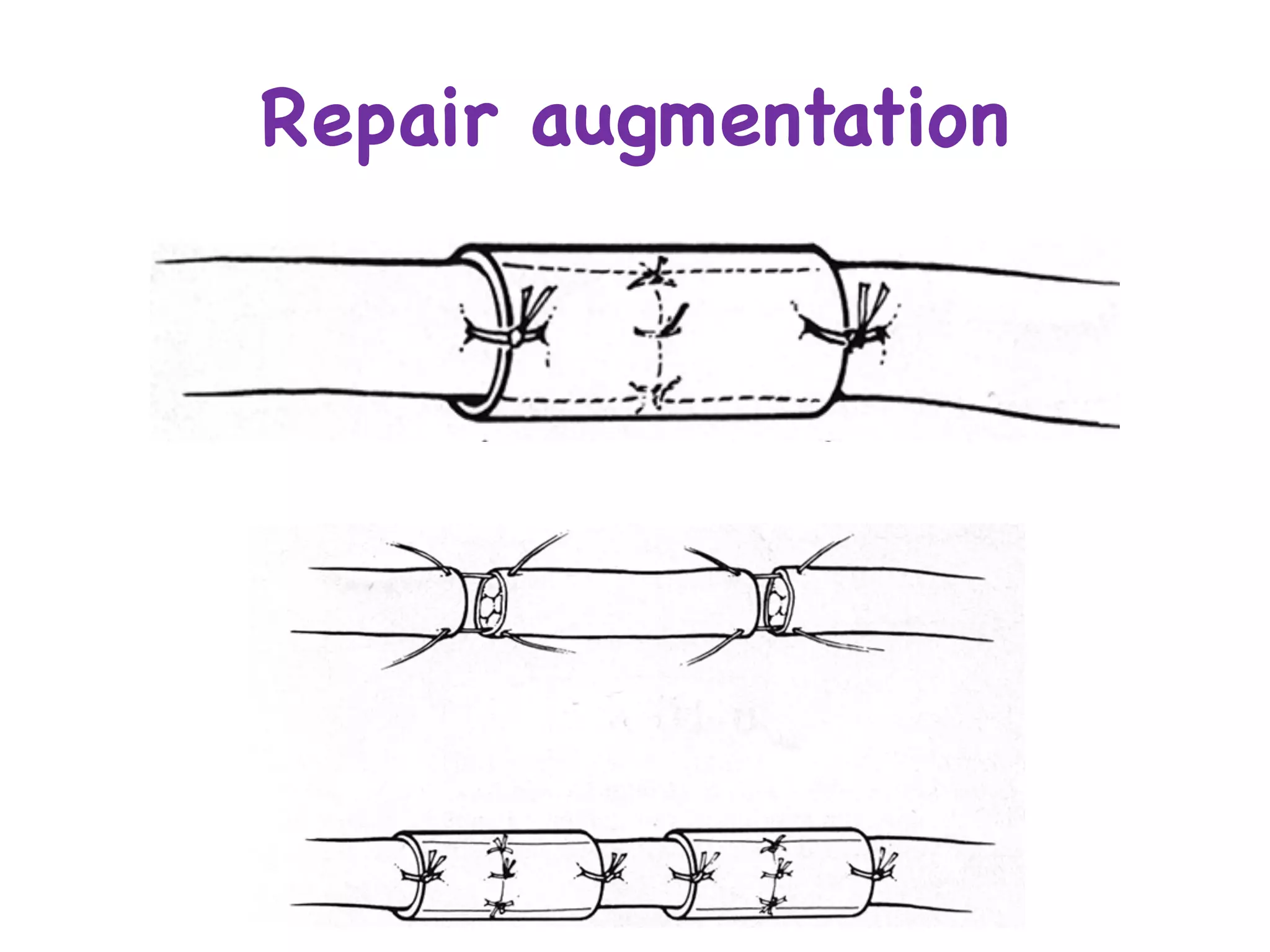
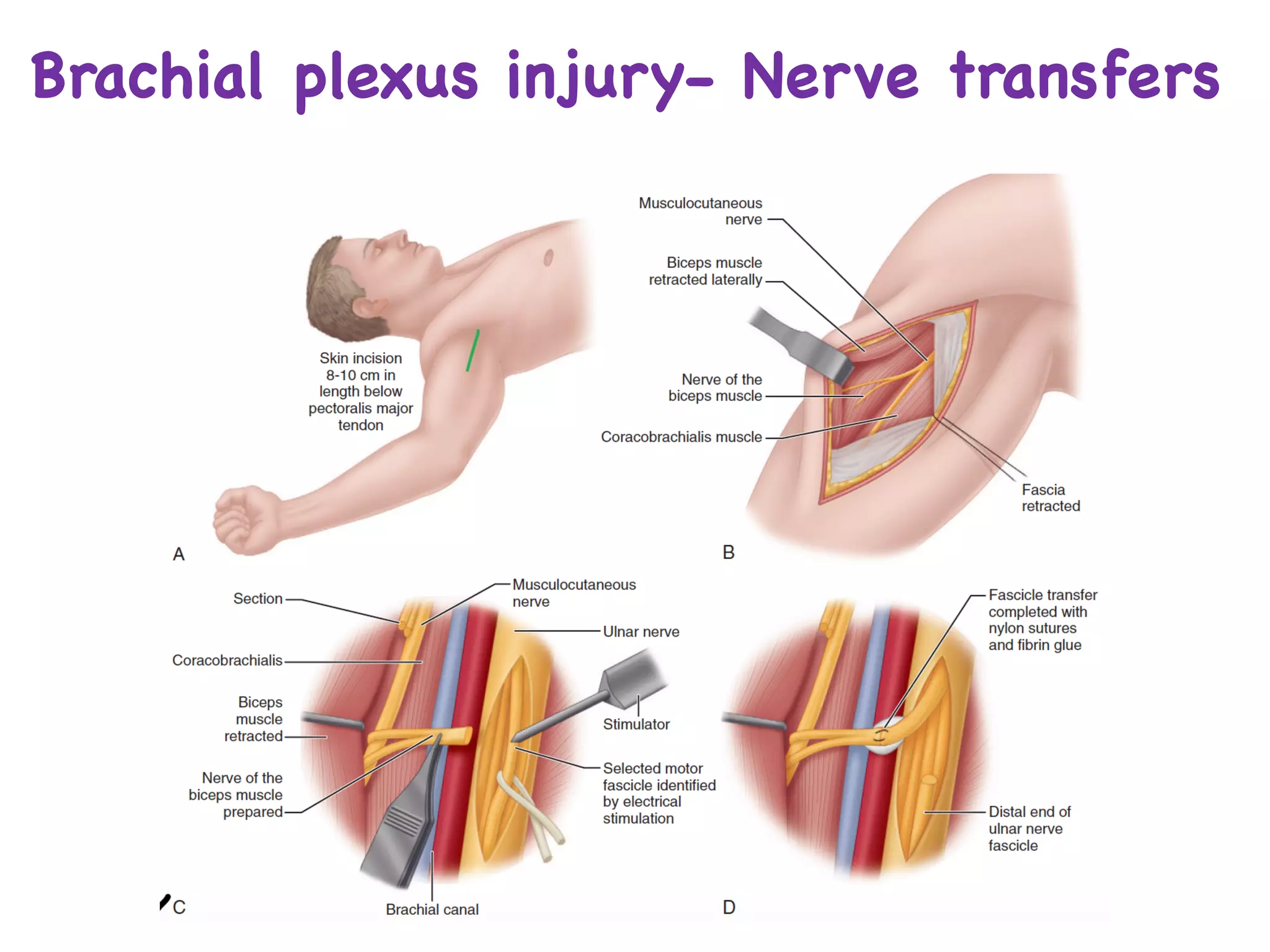
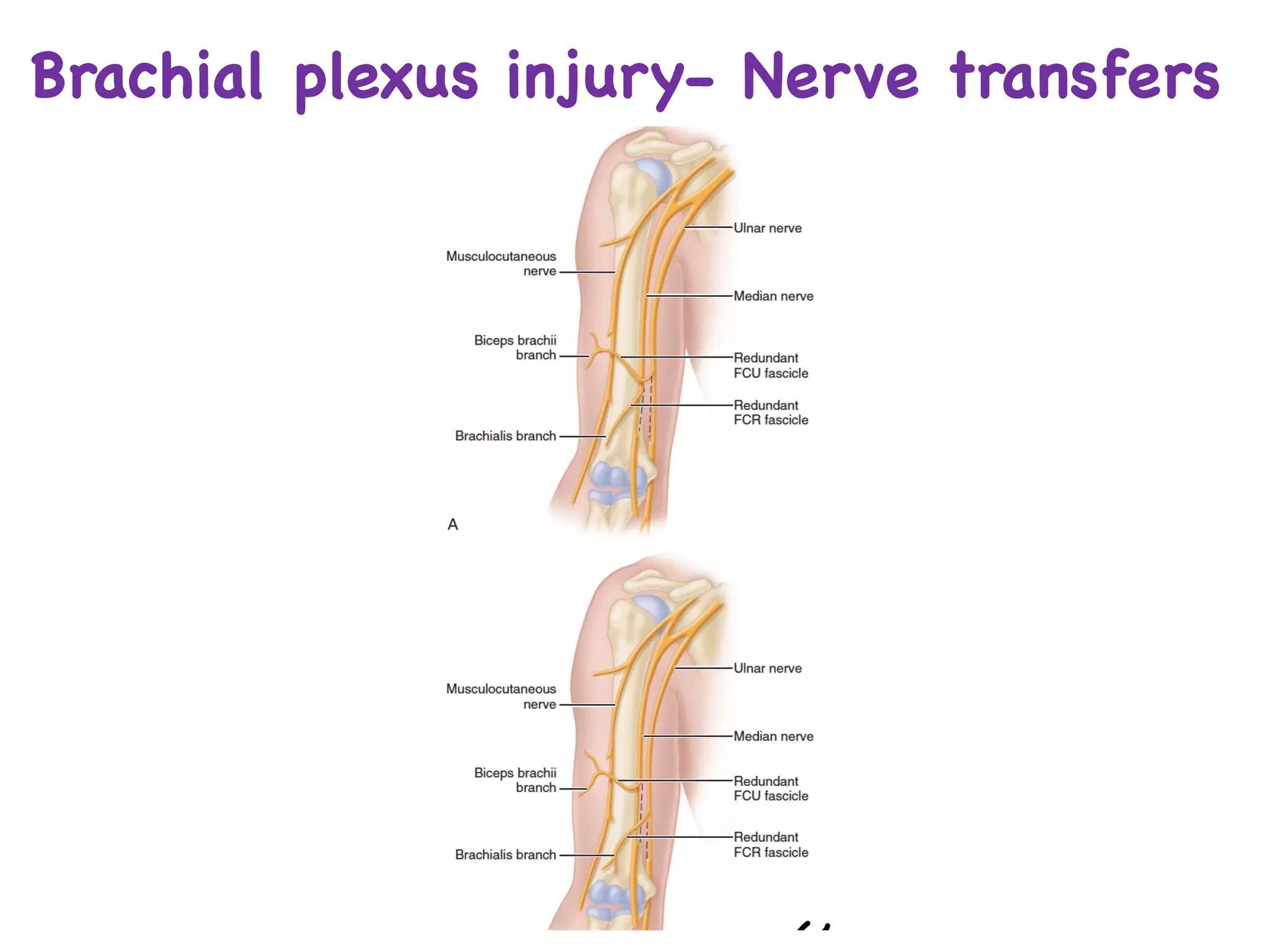
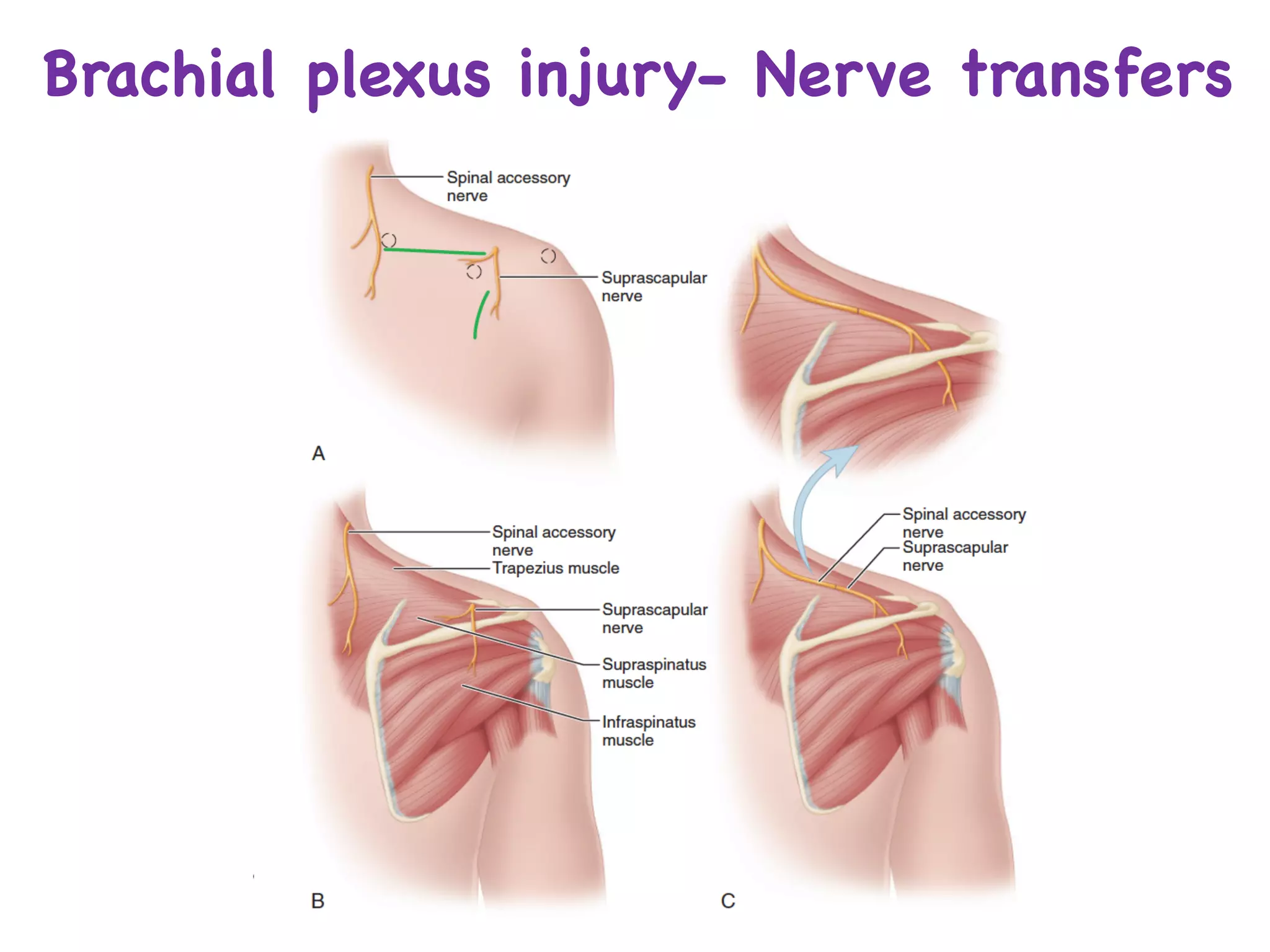
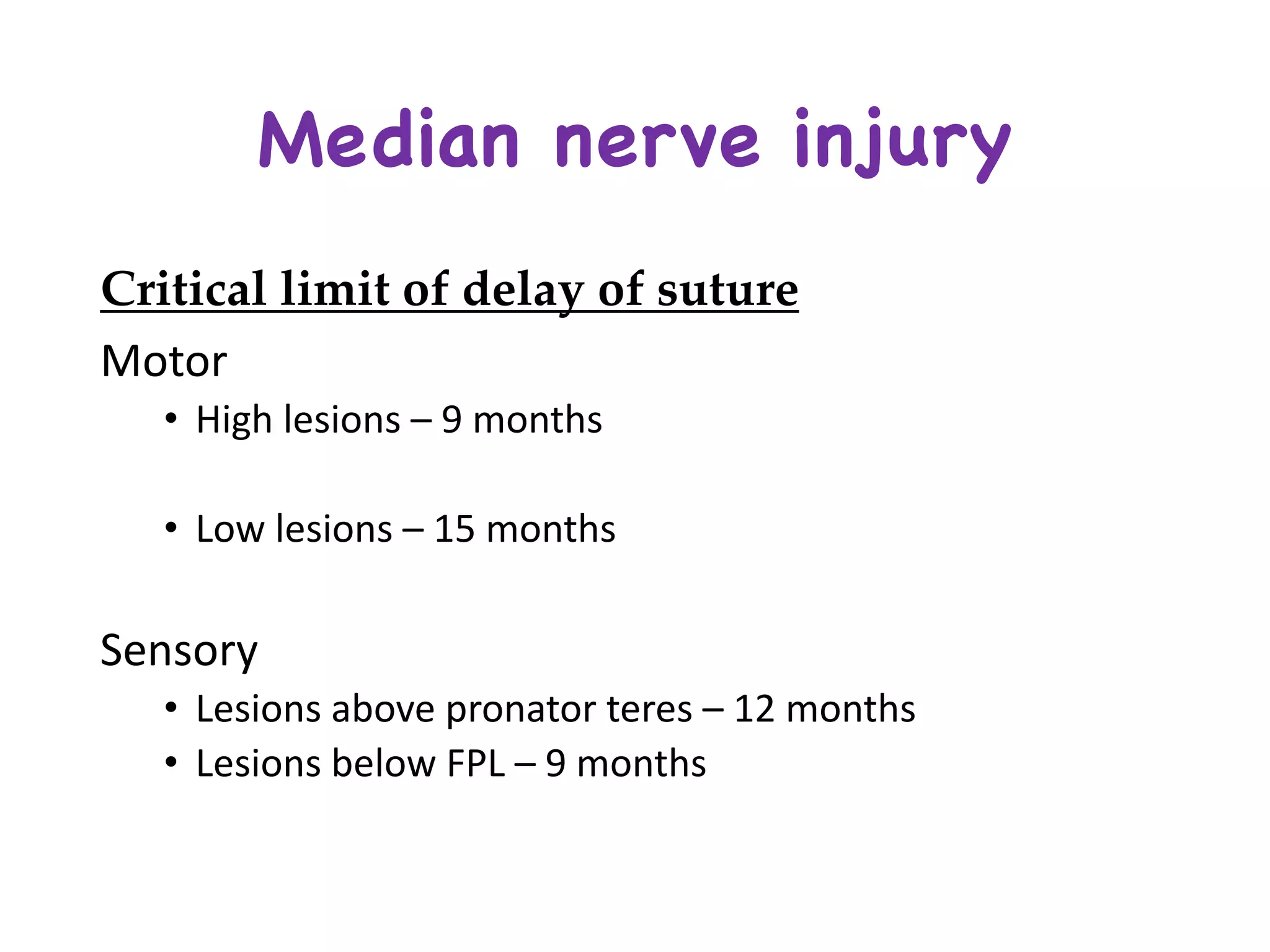
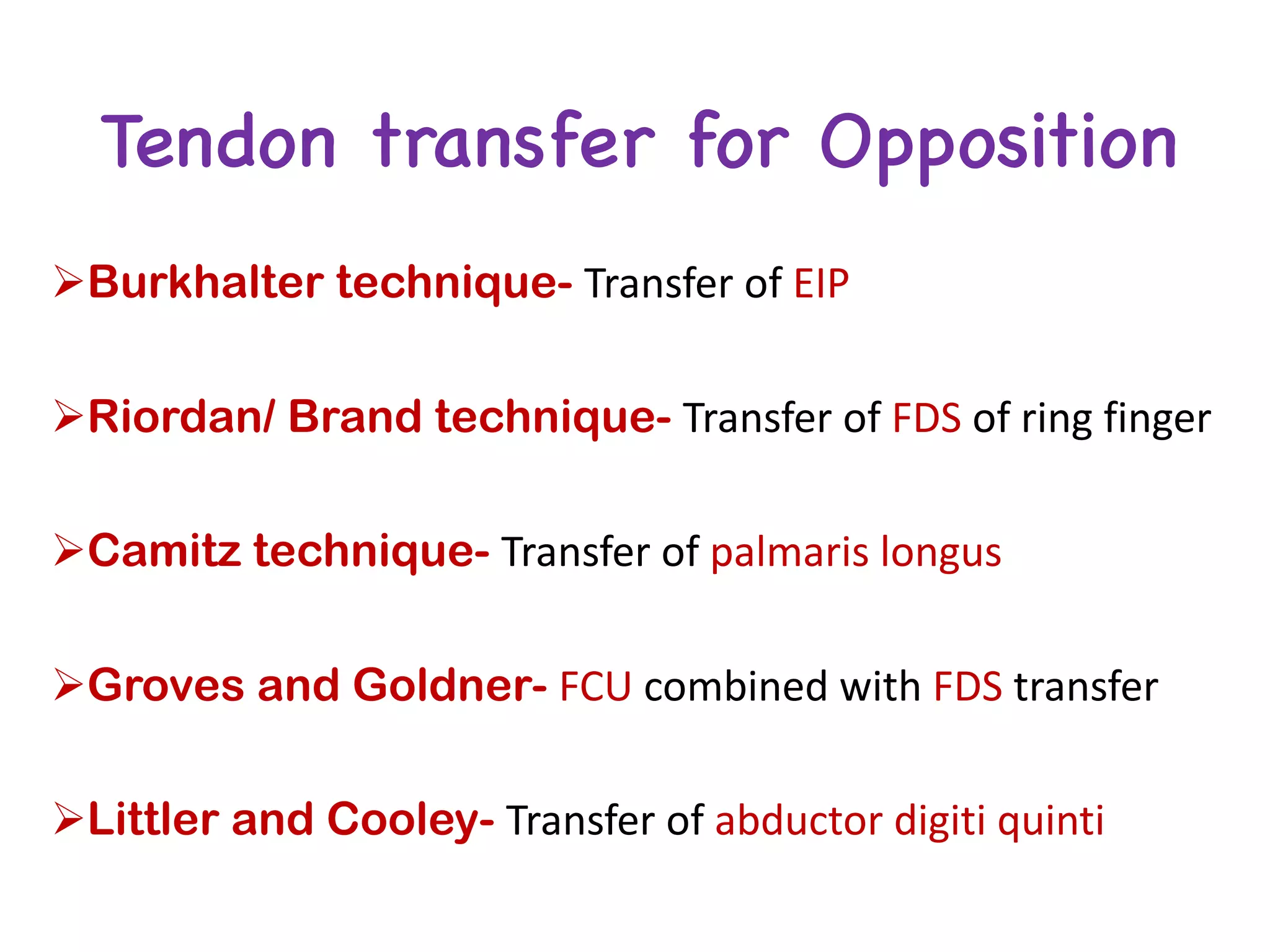
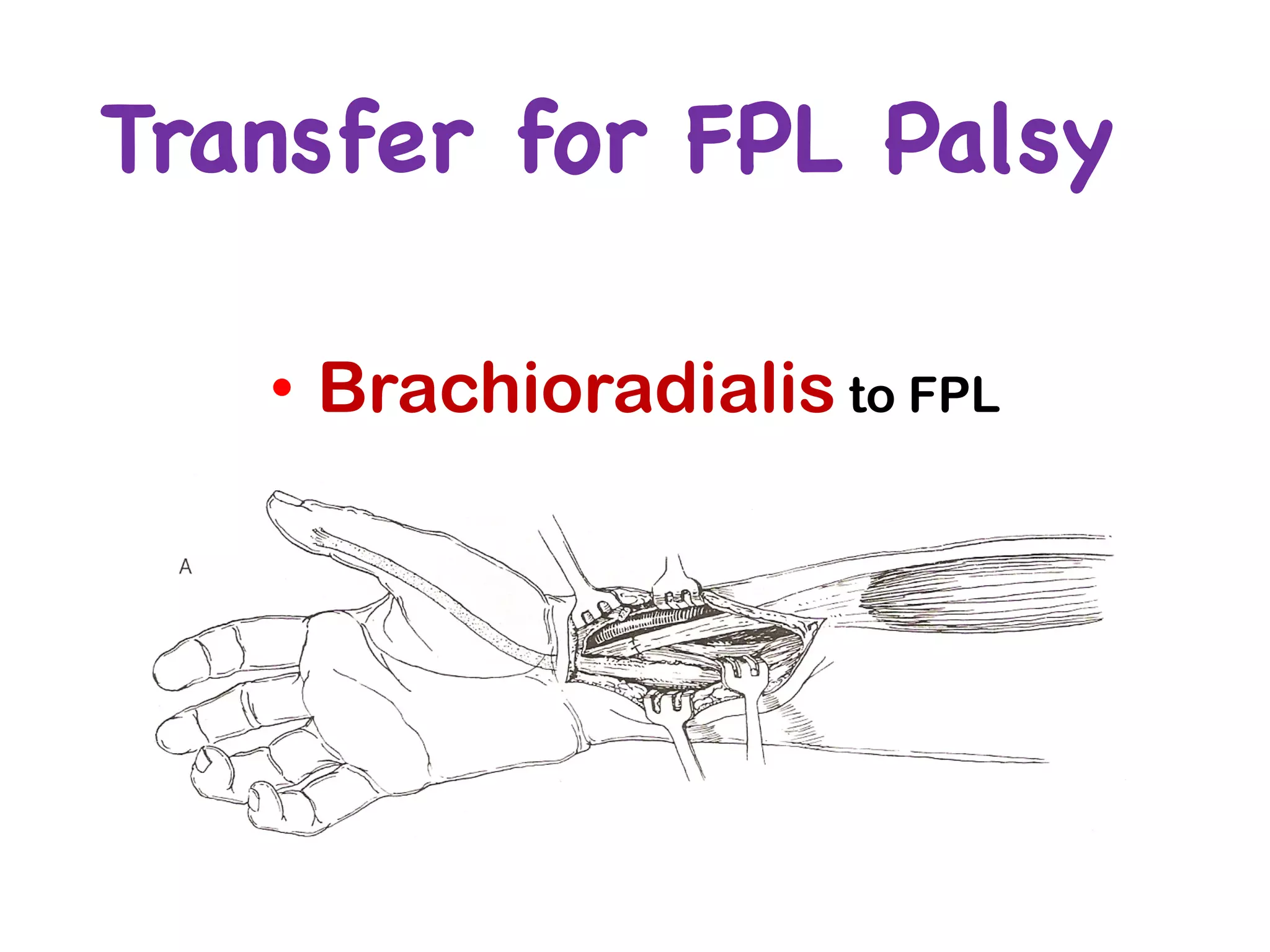
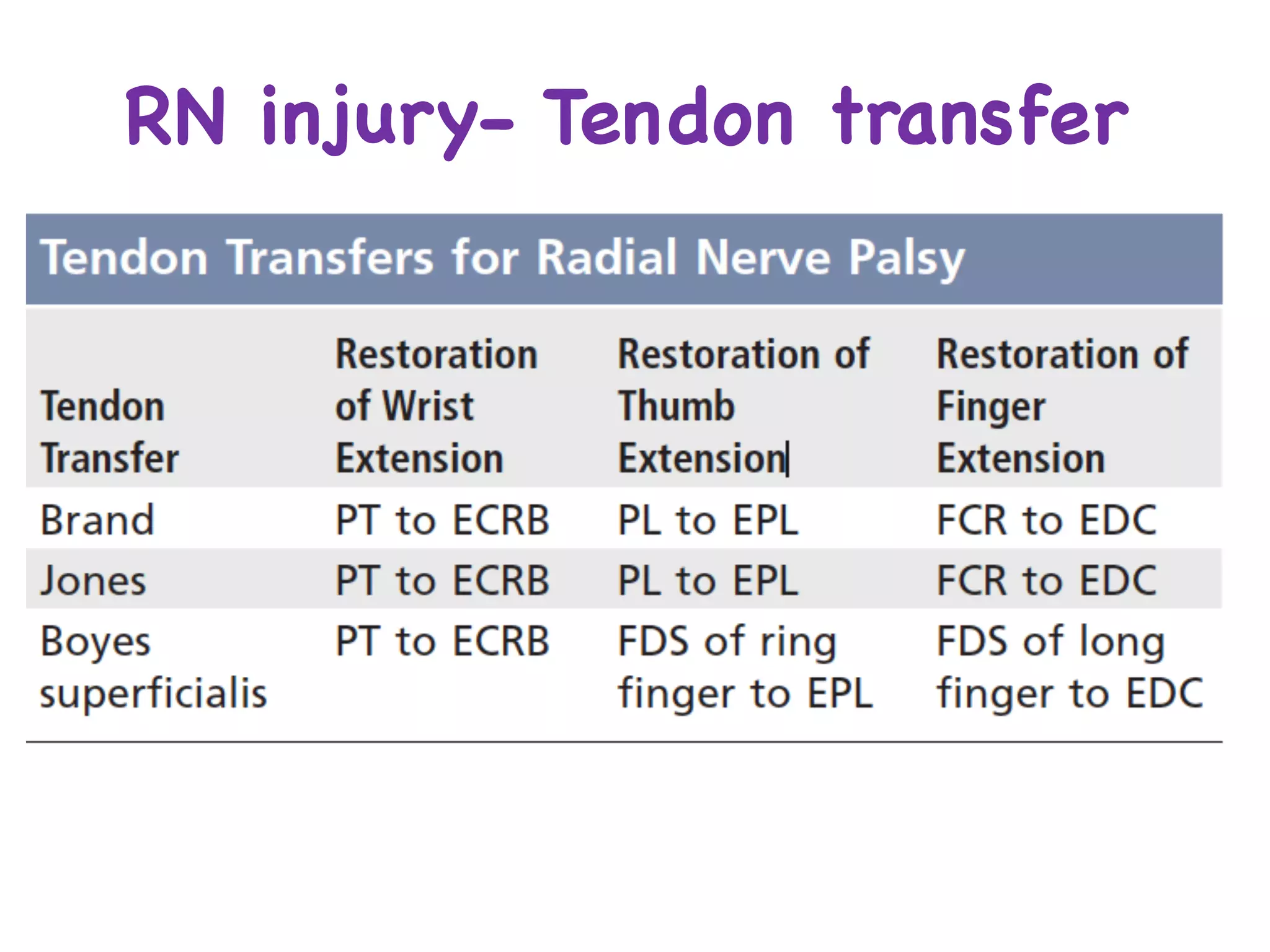
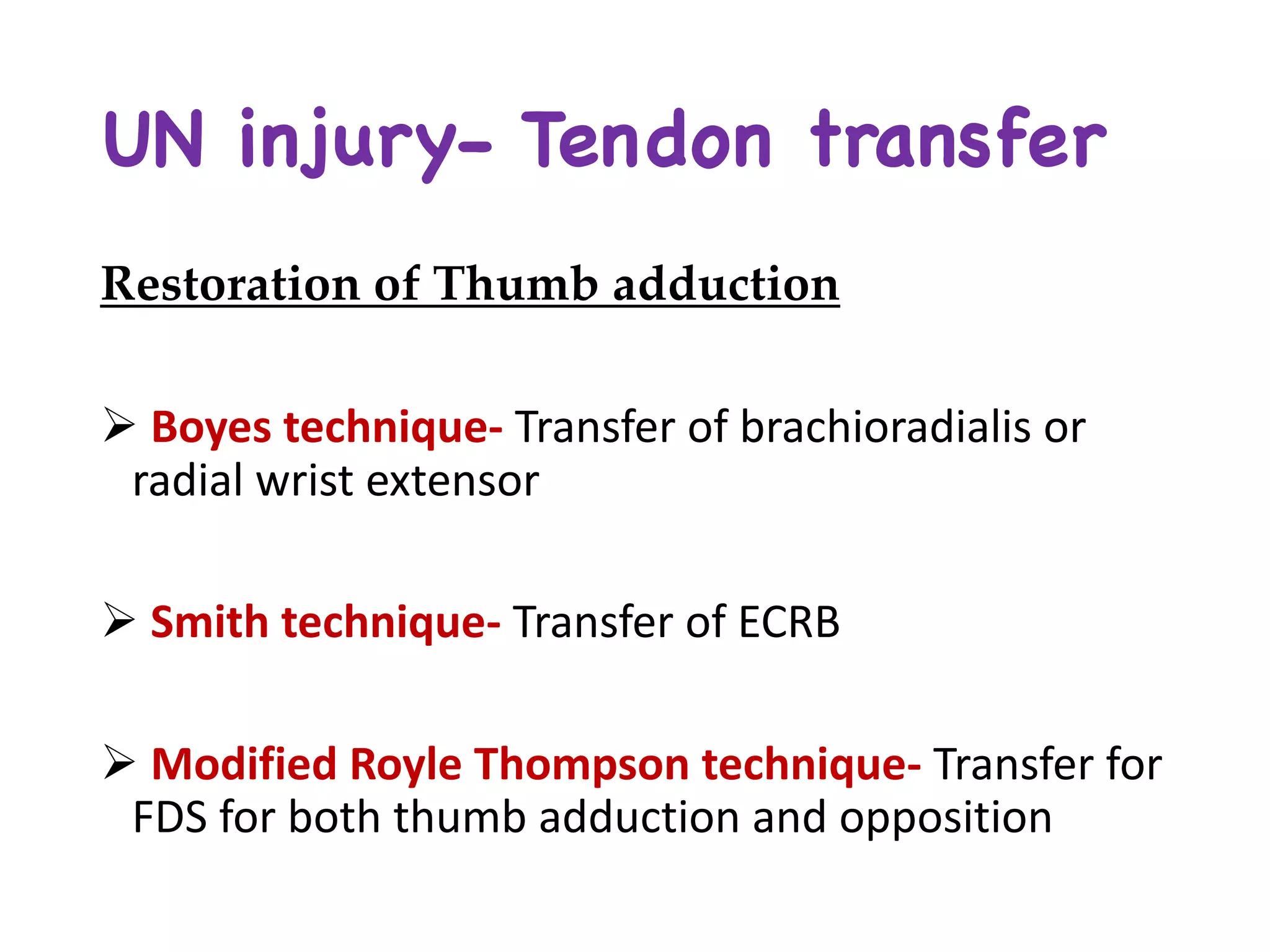
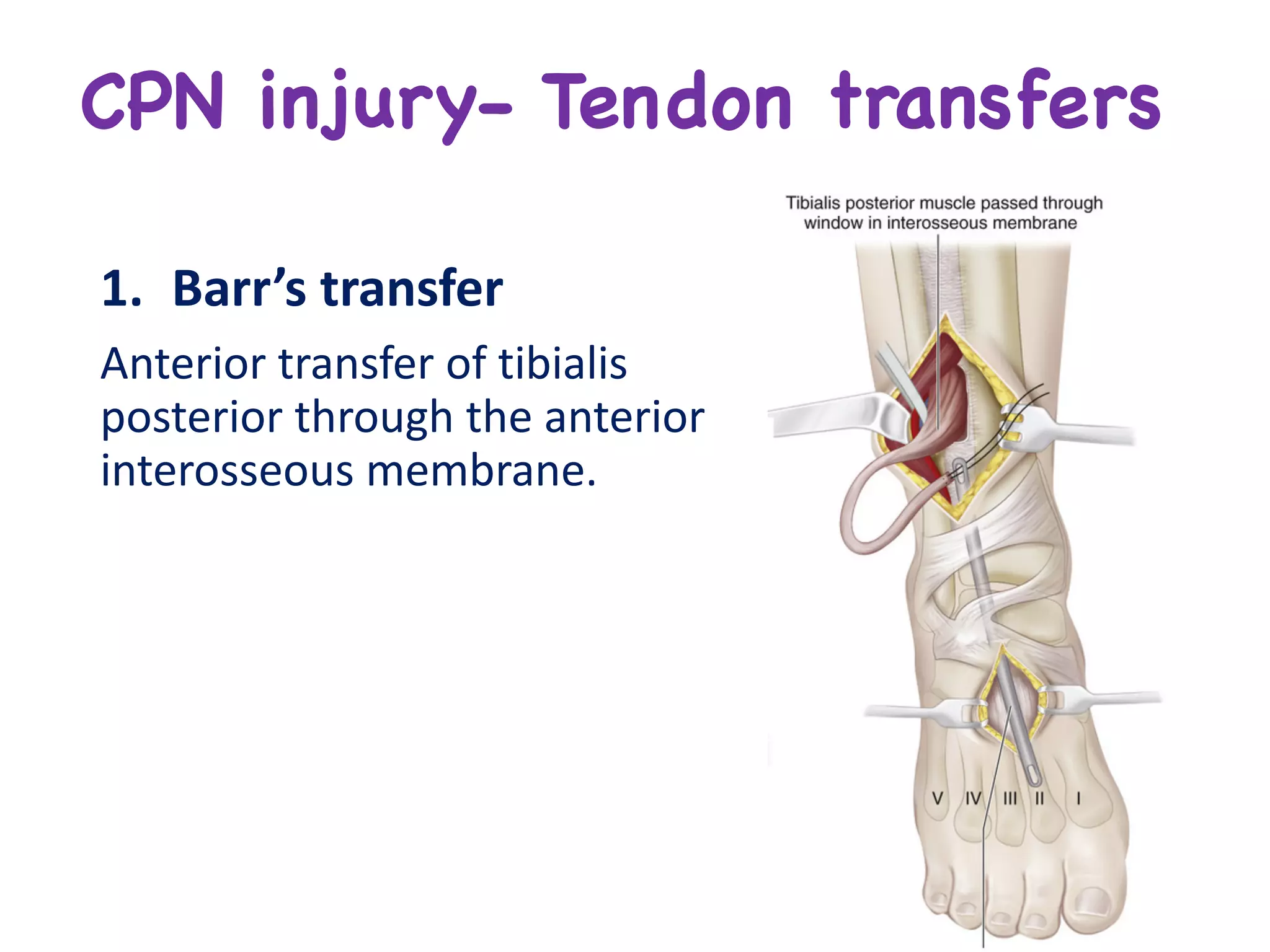
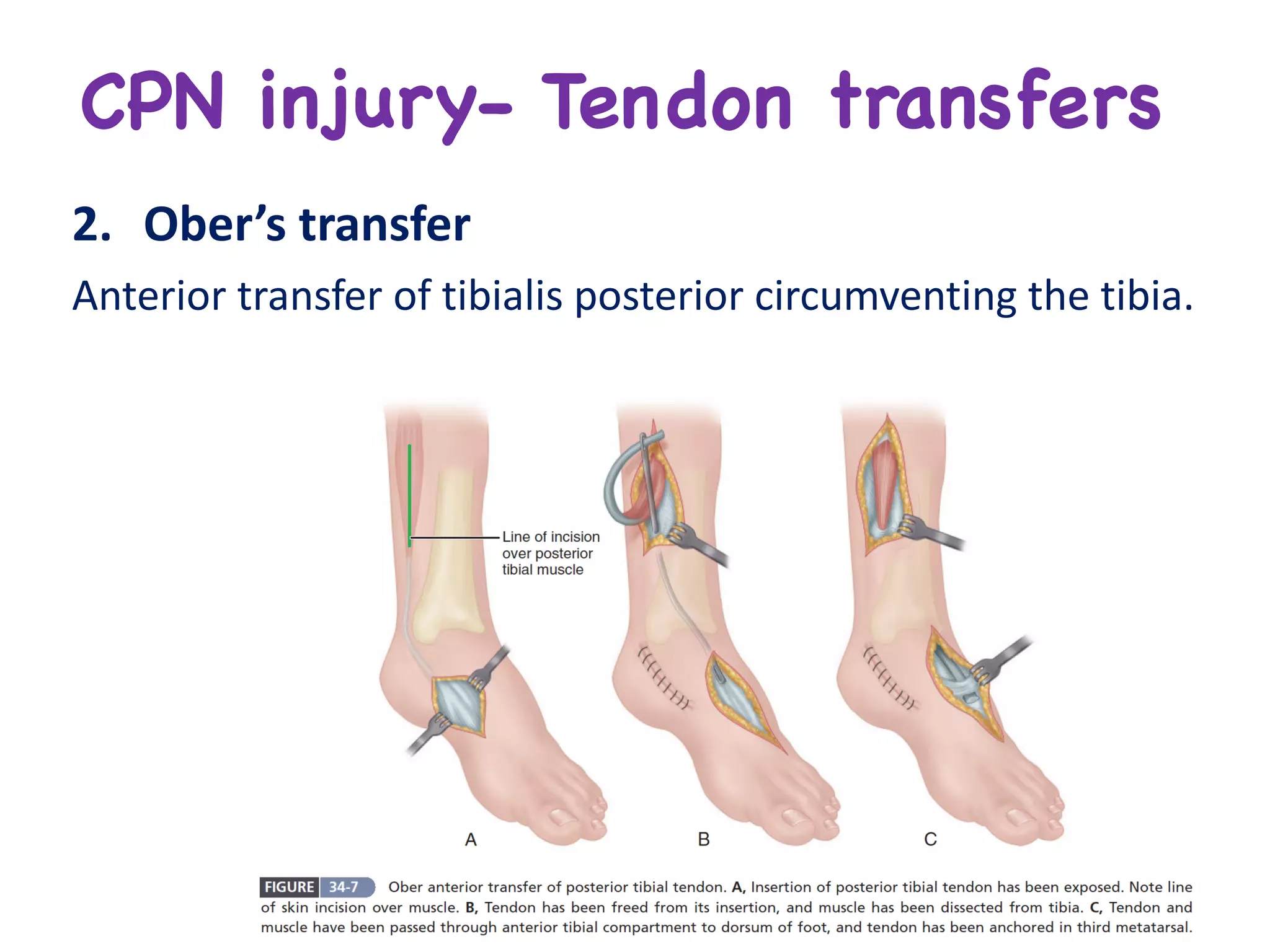
This document discusses the management of peripheral nerve injuries. It covers diagnostic tests such as imaging, electrodiagnostic studies, and clinical tests. General treatment considerations are presented for both open and closed injuries. Surgical techniques for nerve repair include primary repair, nerve grafting, and tendon transfers. Factors that influence nerve regeneration are also outlined. Specific techniques are described for managing brachial plexus injuries and median nerve injuries.