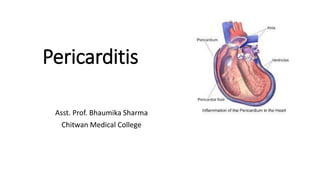
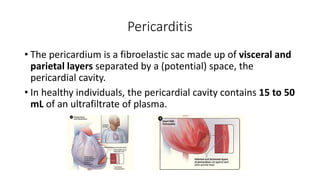
1. Pericarditis is inflammation of the pericardium and can be caused by viral infections, autoimmune diseases, uremia, or other conditions.
2. It presents clinically as chest pain, pericardial friction rub, dyspnea, or fever and is diagnosed using echocardiogram, ECG, or pericardiocentesis.
3. Treatment involves identifying the cause, administering medications like NSAIDs or steroids, and monitoring for complications like cardiac tamponade.