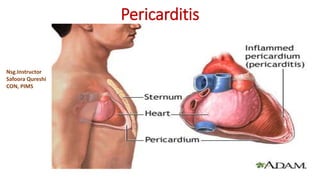
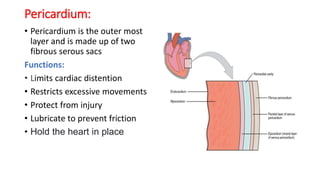
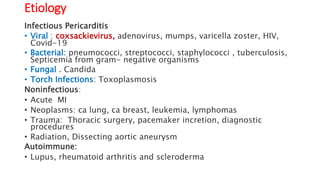
Pericarditis is inflammation of the pericardium, causing sharp chest pain and potentially leading to complications like pericardial effusion and cardiac tamponade. The condition can be infectious or noninfectious, with various causes including viruses, bacteria, trauma, and autoimmune diseases. Diagnosis includes a physical examination, ECG, and imaging tests, with treatment options ranging from NSAIDs and antibiotics to pericardiocentesis in severe cases.