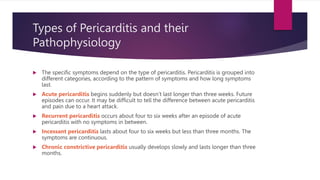
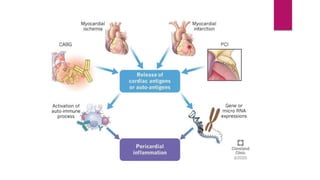
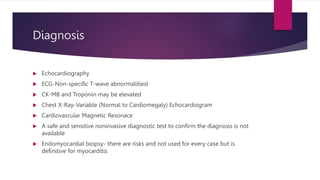
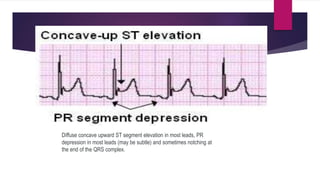
Pericarditis is the inflammation of the pericardium, leading to symptoms such as sharp chest pain, which may improve when sitting up or leaning forward, and is often treated with medications or surgery in severe cases. The condition affects approximately 27.7 per 100,000 individuals annually and can recur in about 30% of patients, with varying forms including acute, recurrent, and chronic constrictive pericarditis. Diagnosis often involves echocardiography and ECG, while complications can include cardiac tamponade, necessitating emergency treatment.


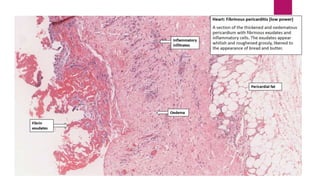
![Classification
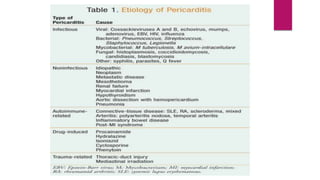
Pericarditis can be classified according to the composition of the fluid that accumulates
around the heart.[22]
Types of pericarditis include the following:[citation needed]
serous
purulent
fibrinous
caseous
hemorrhagic](https://image.slidesharecdn.com/pericarditis-230415224131-eaa977f3/85/Pericarditis-pptx-5-320.jpg)

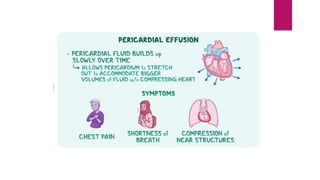





![Amount of Pericarditis
Cardiac Effusion In a healthy individual, the pericardial sac
contains between 15 and 50 milliliters (mL) of serous fluid.
Cardiac Temponade Traditionally, acute cardiac tamponade
is associated with between 200 ml and 300 ml of sudden
accumulation of intrapericardial fluid[1] or, in chronic slowly
evolving accumulation, of volumes between 1000 and 2000
ml](https://image.slidesharecdn.com/pericarditis-230415224131-eaa977f3/85/Pericarditis-pptx-19-320.jpg)