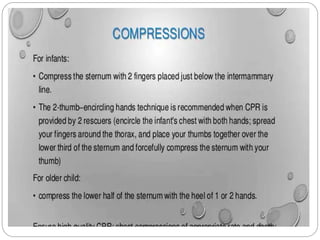
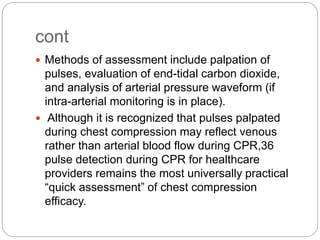
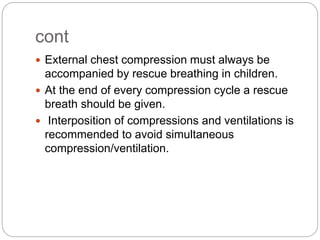
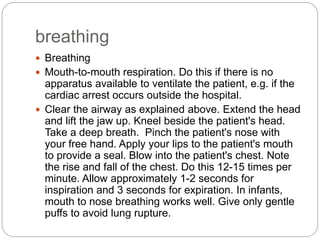
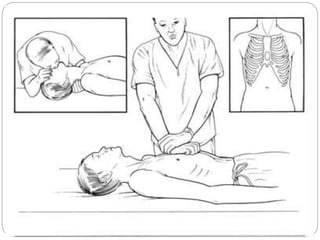
This document discusses resuscitation in children. It defines resuscitation and notes that the age of the victim guides treatment decisions. Discriminating based solely on age is inadequate, as there is no single parameter separating infants, children, and adults. Factors like size, illness, and rescuer strength should also be considered. The document then discusses various aspects of pediatric resuscitation, including airway management, breathing, chest compressions, defibrillation, and foreign body removal. It emphasizes the importance of ventilation for children and the need to tailor treatment based on the victim's age.









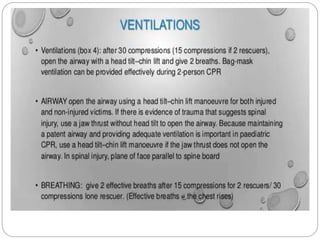
![cont
In general, pediatric pre hospital arrest has been
characterized as hypoxic, hypercarbic arrest with
respiratory arrest preceding asystolic cardiac
arrest.
Therefore, a focus on early ventilation and early
CPR (rather than early emergency medical
services [EMS] activation and/or defibrillation)
appears to be warranted.](https://image.slidesharecdn.com/resuscitationinchildren-220104135111/85/Resuscitation-in-children-16-320.jpg)