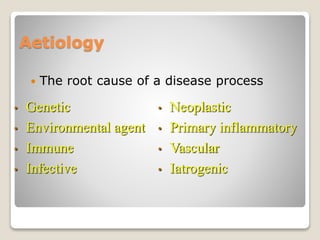
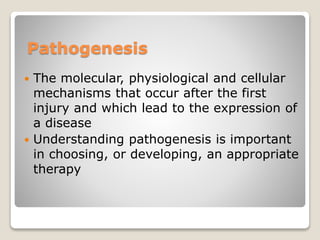
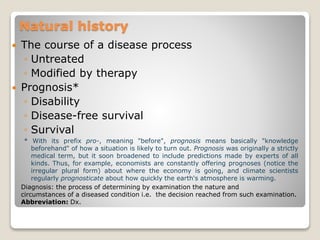
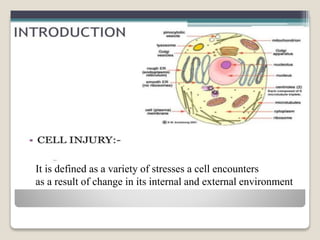
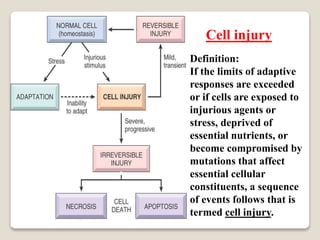
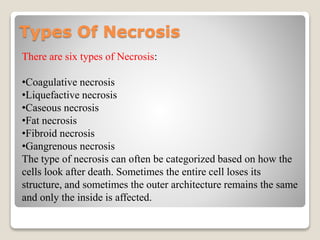
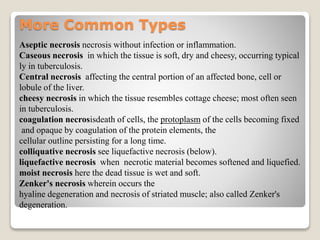
Pathology is the study of the nature and causes of diseases, focusing on their origins, mechanisms, and effects on structures and functions. Key aspects include the etiology of diseases, pathogenesis, diagnosis, and the consequences such as sequelae. Additionally, it encompasses various diagnostic tools and branches, including histopathology and genetics, to understand and manage diseases effectively.