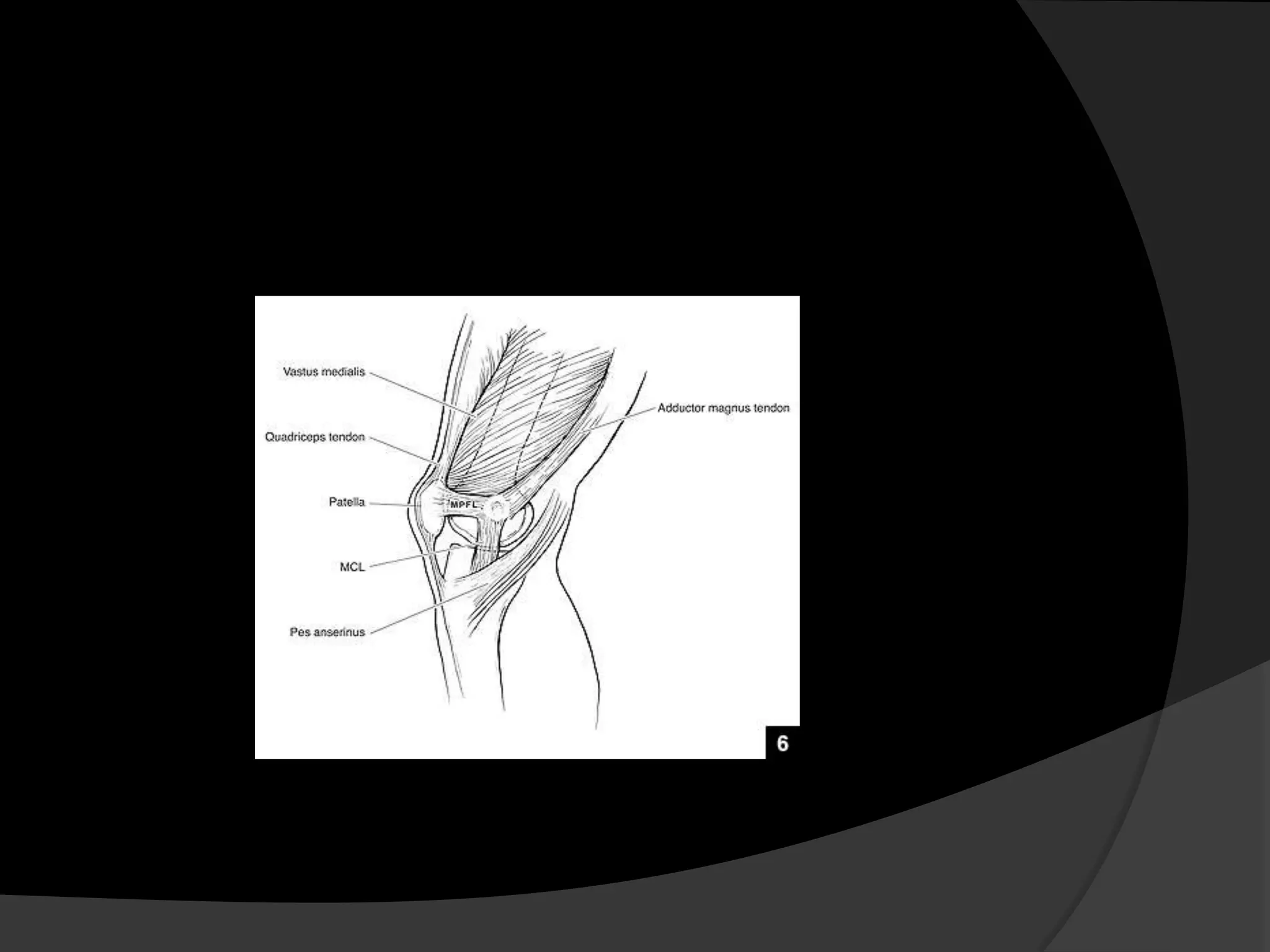
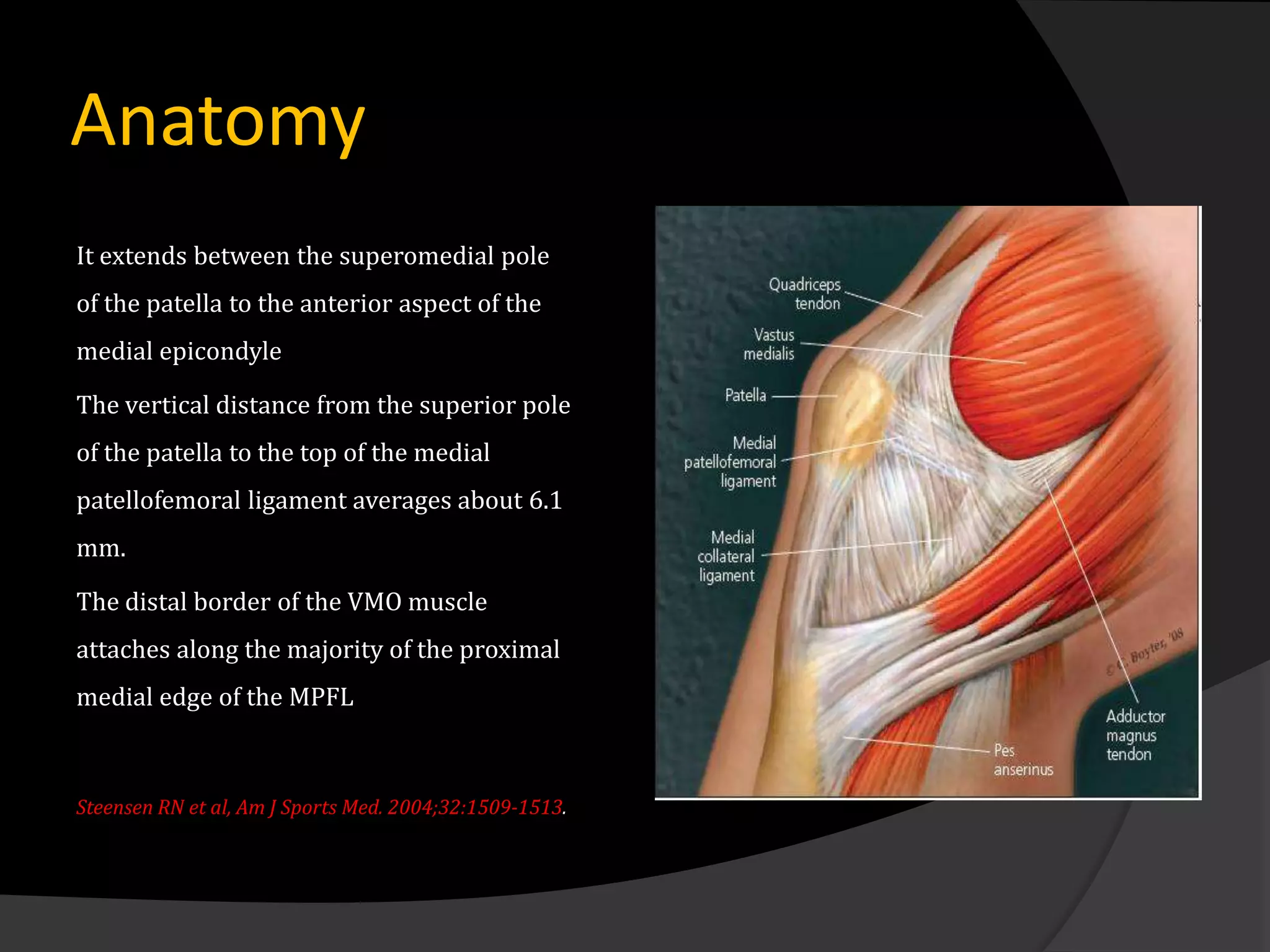
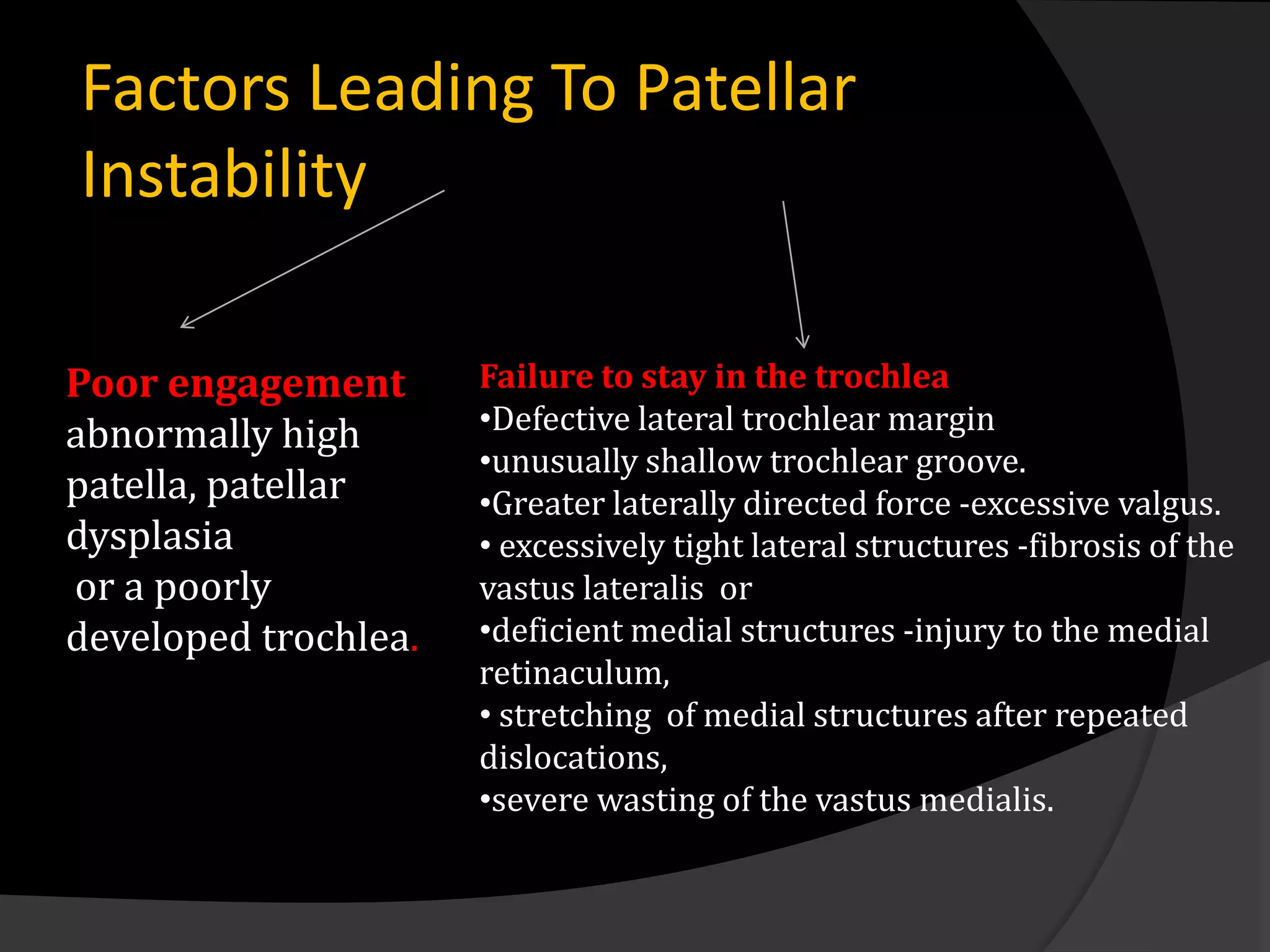
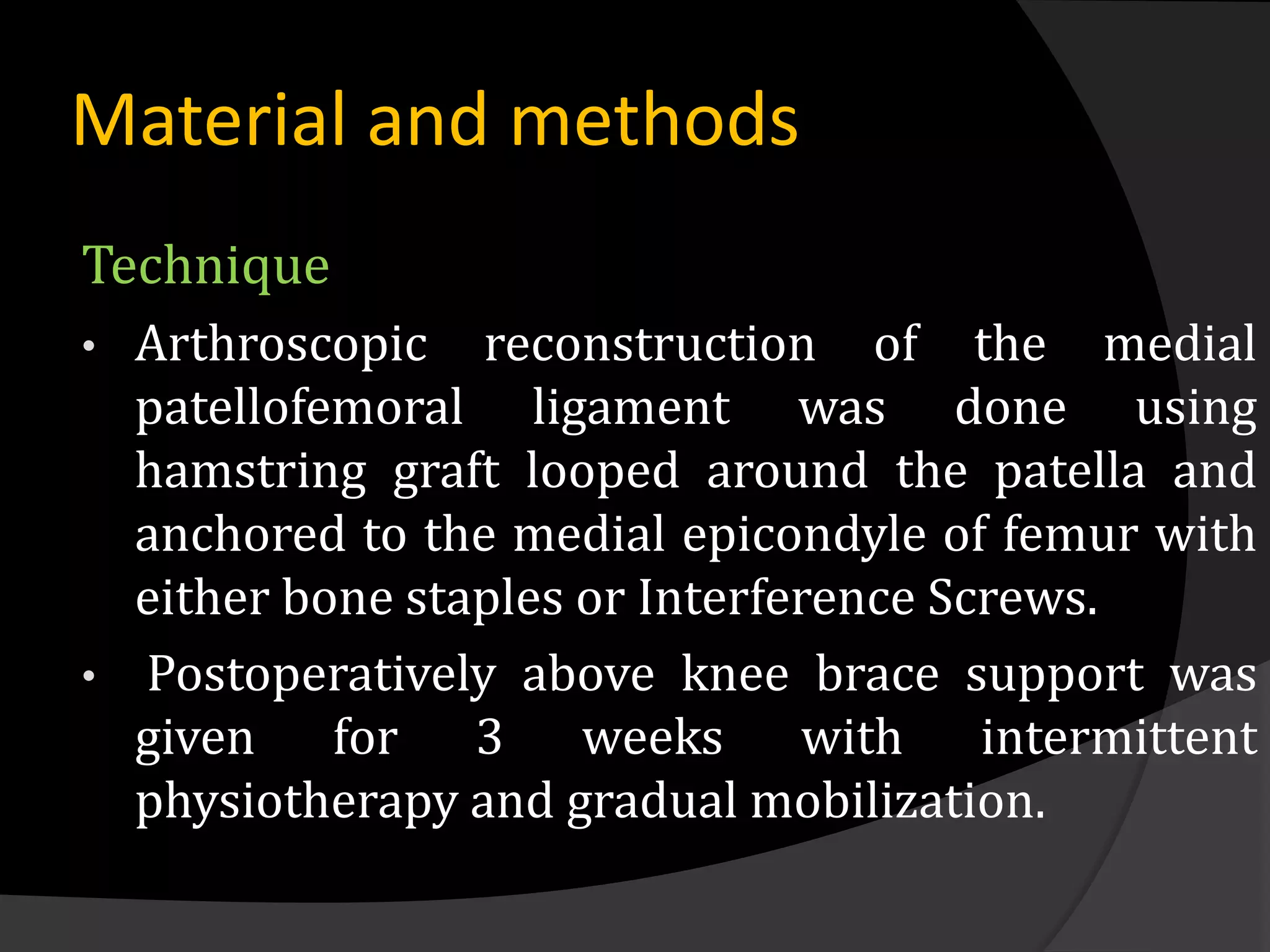
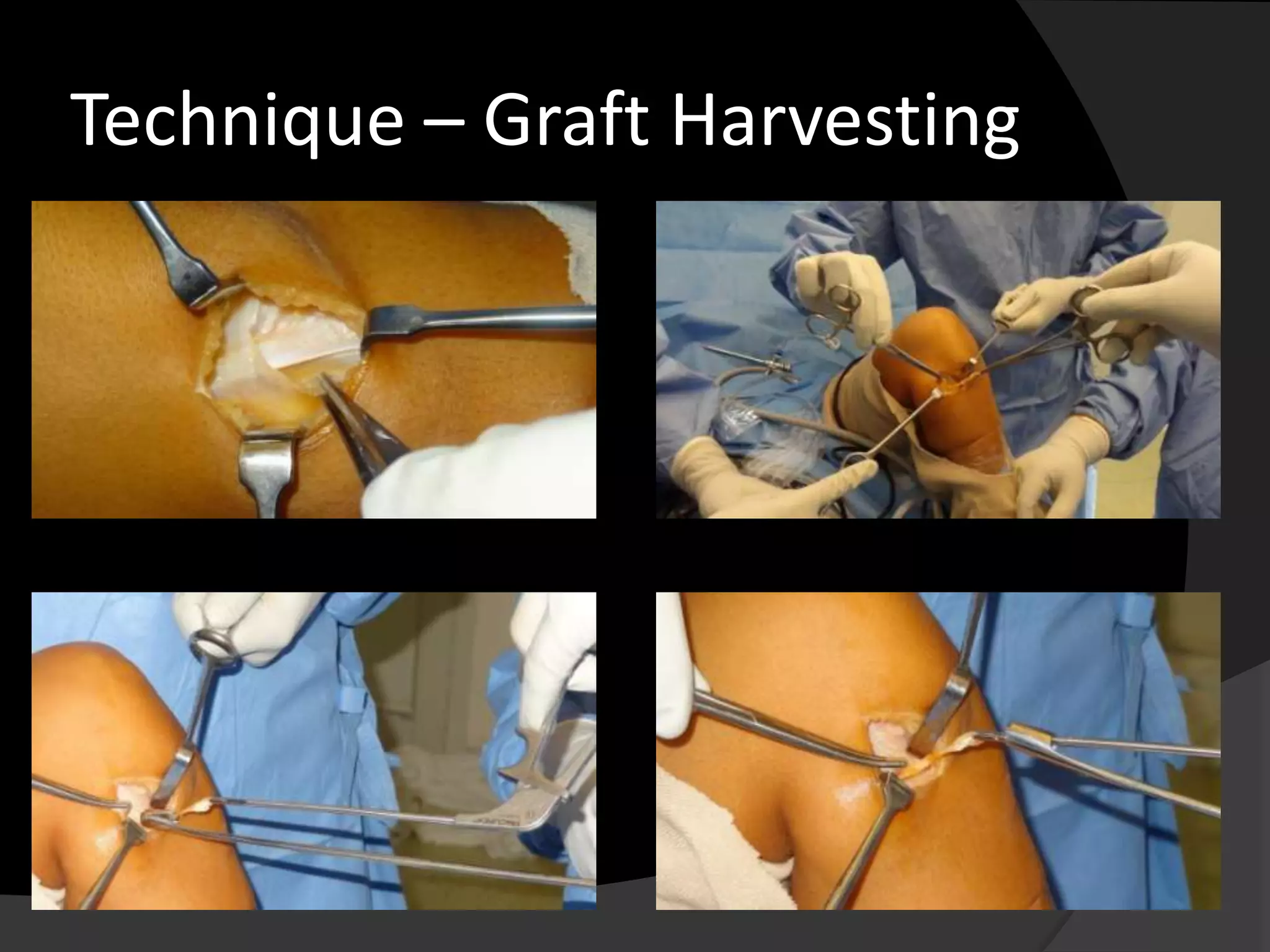
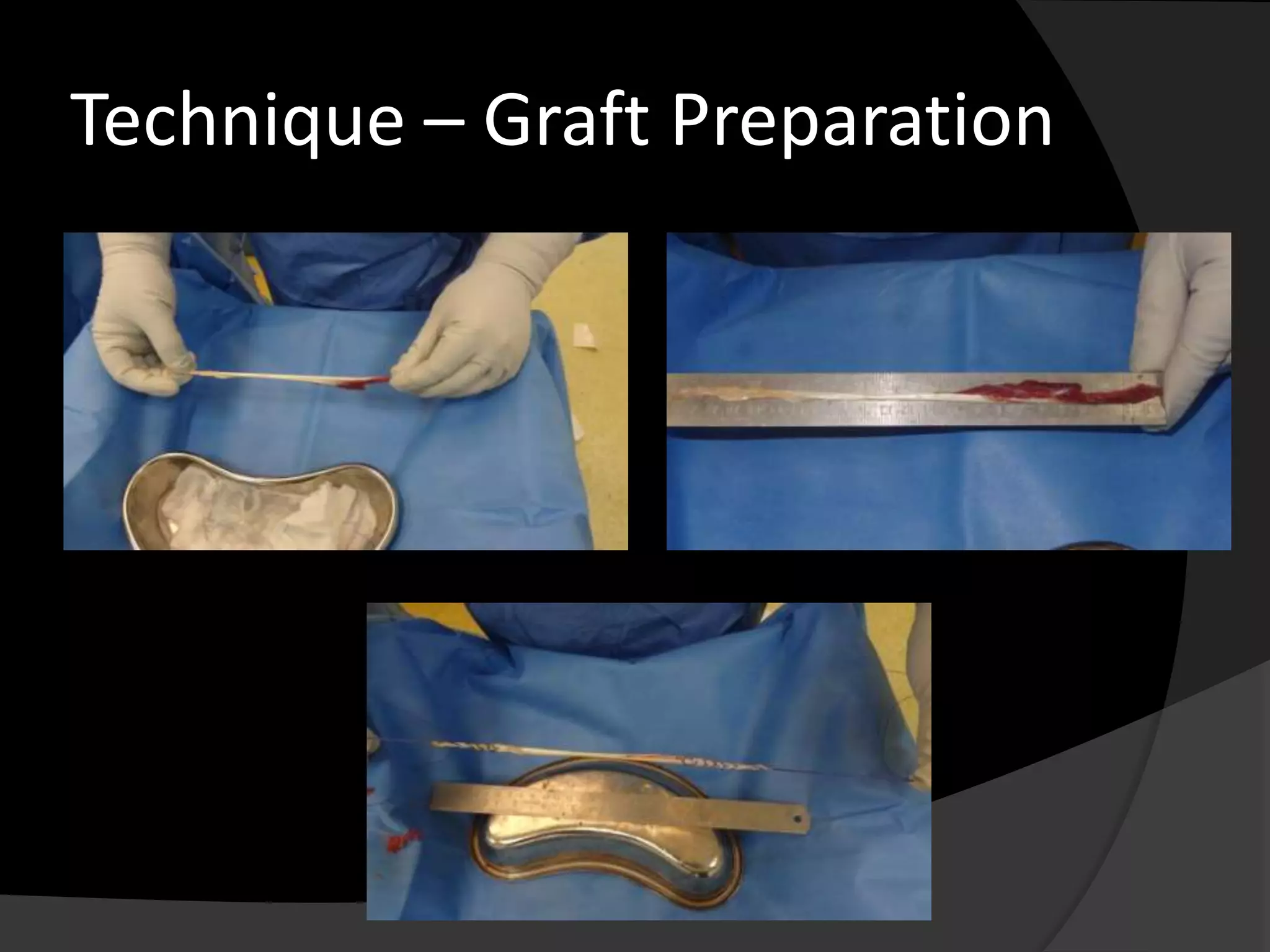
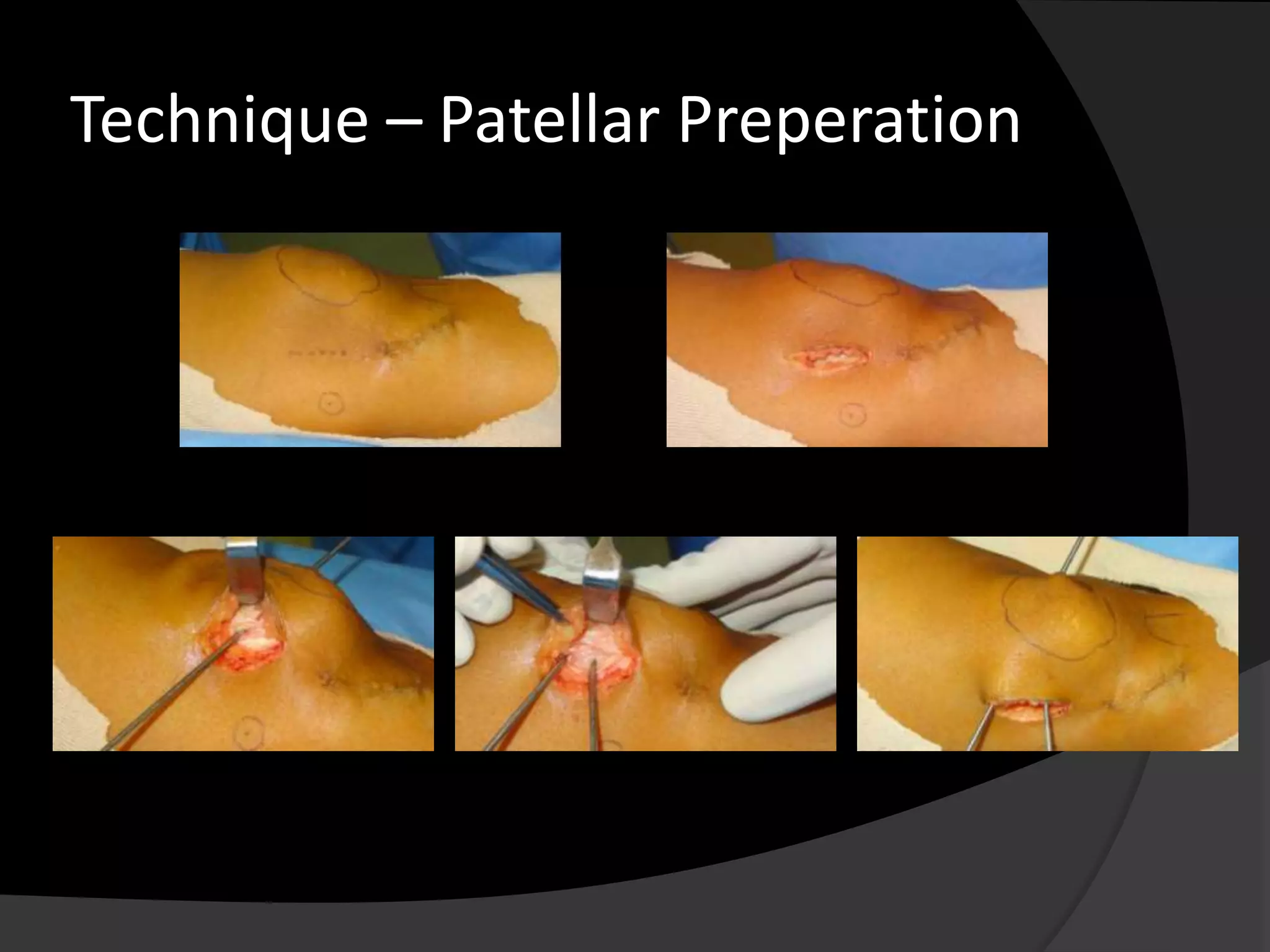
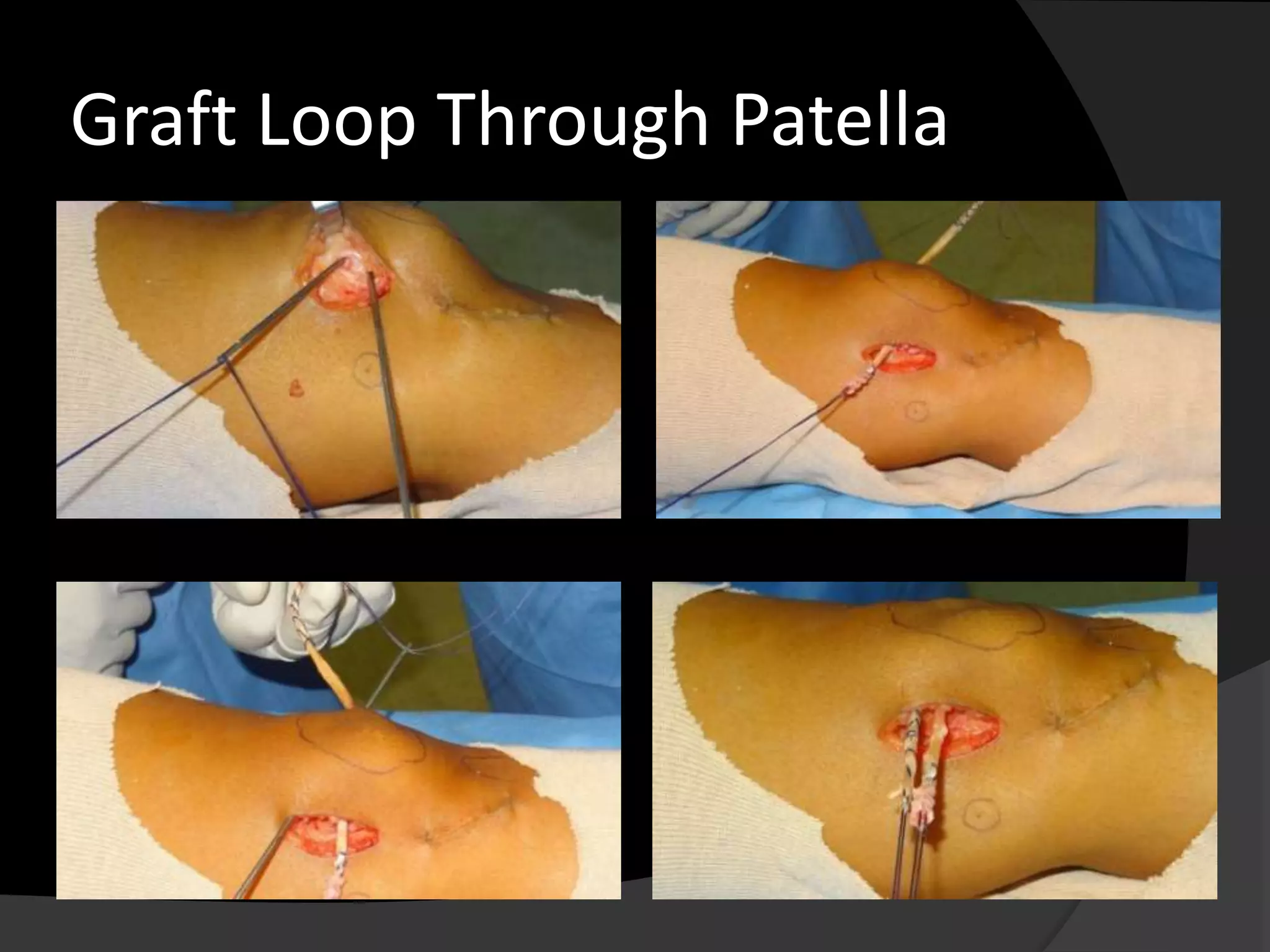
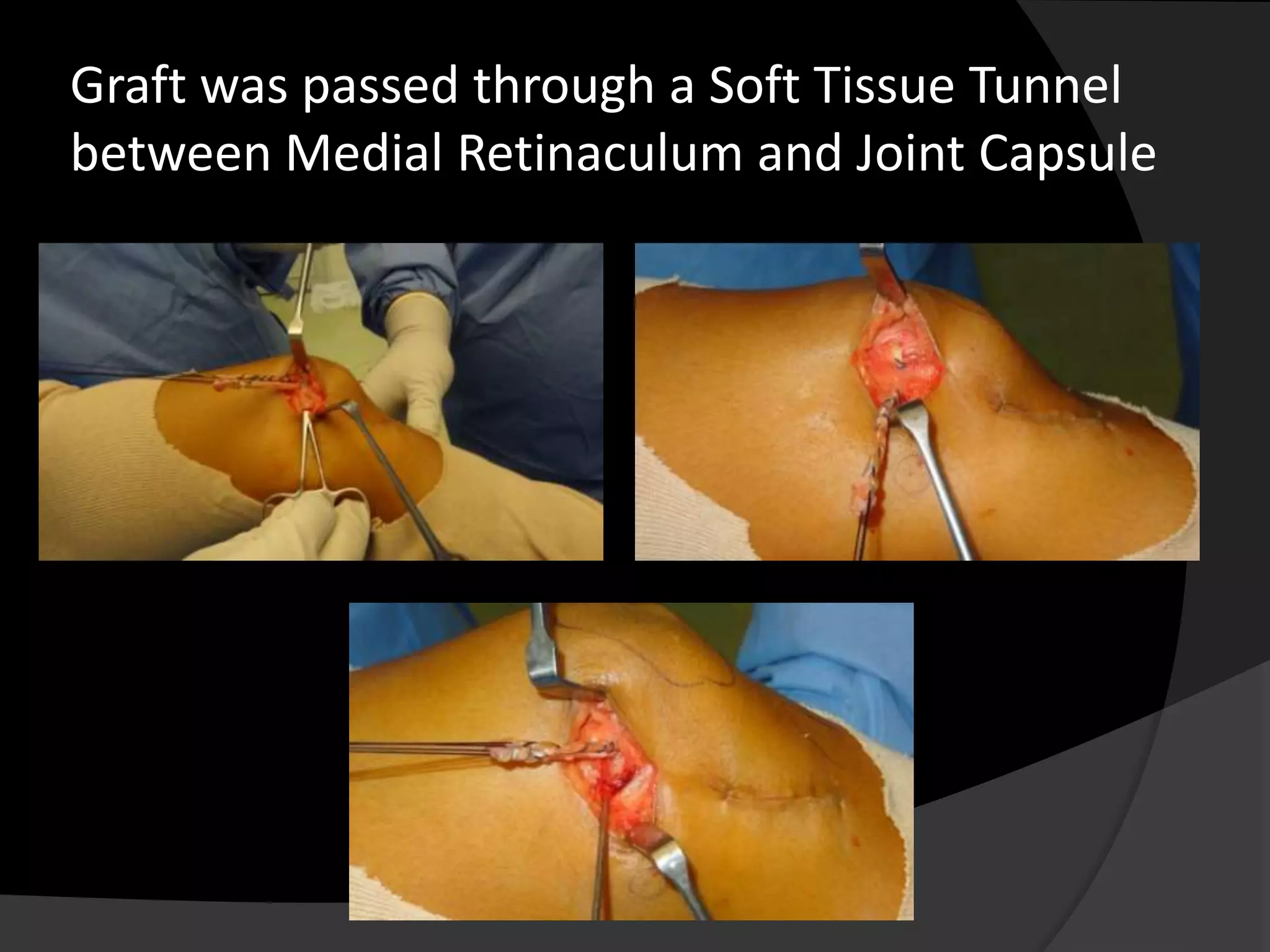
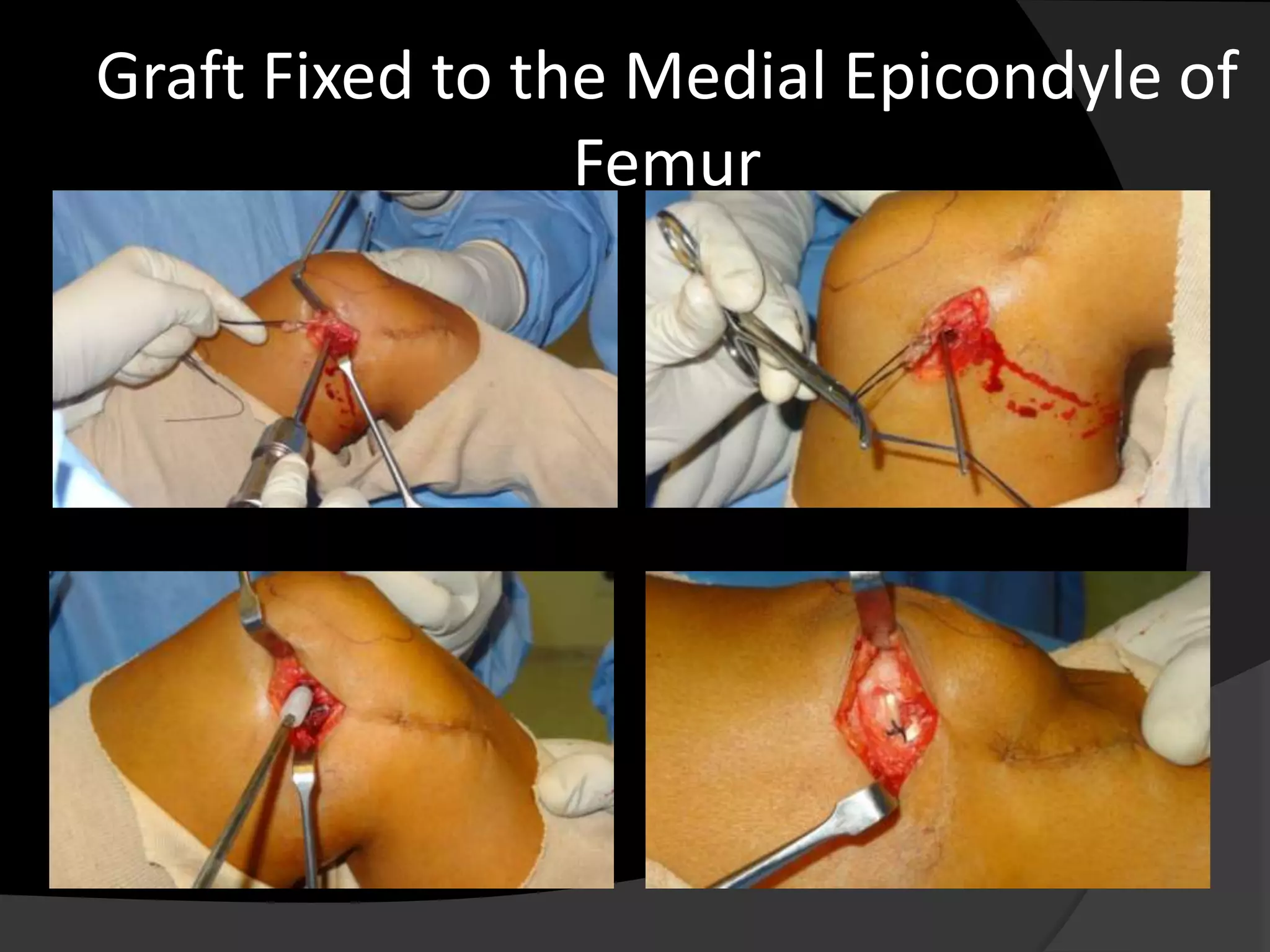
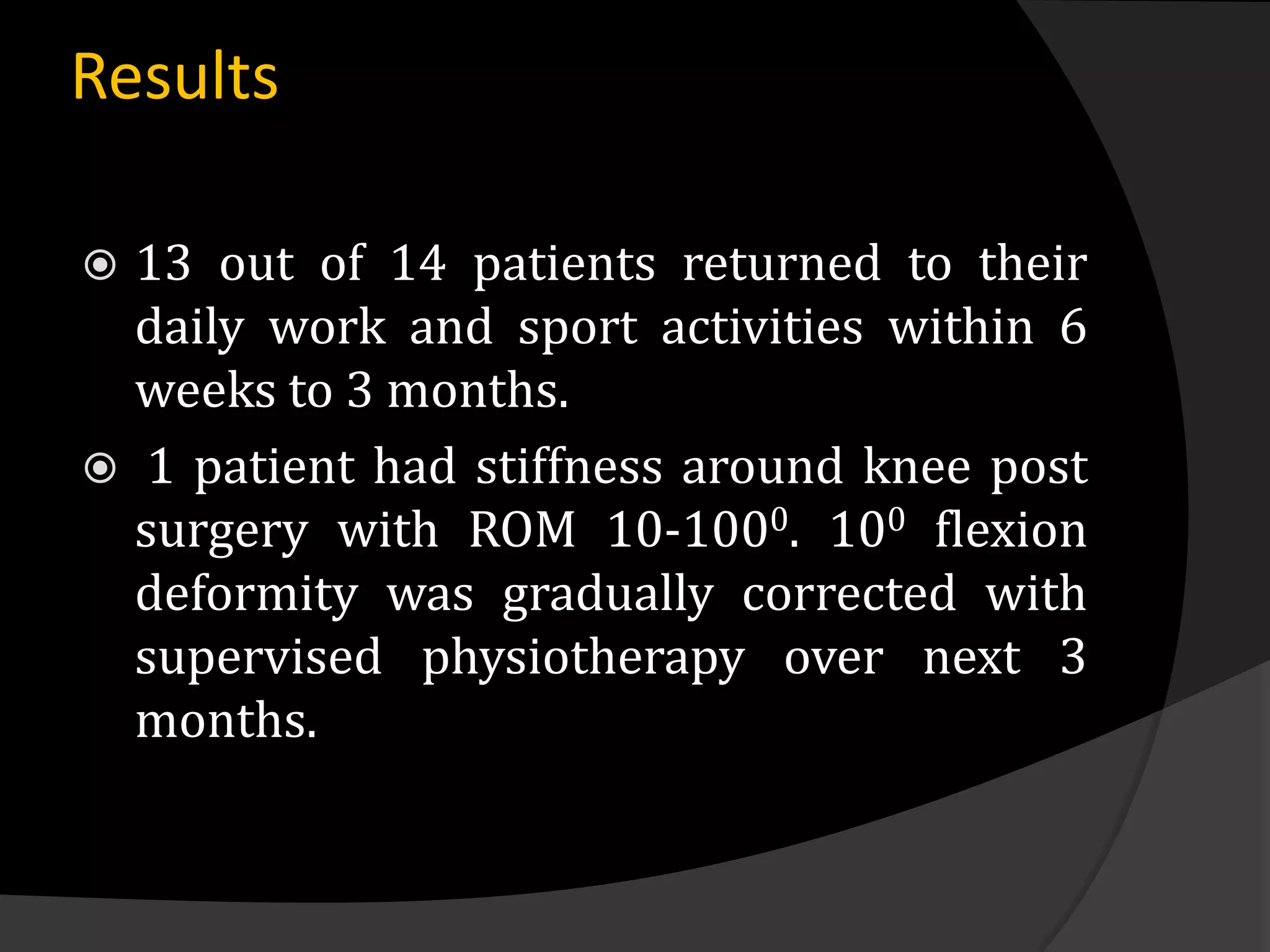
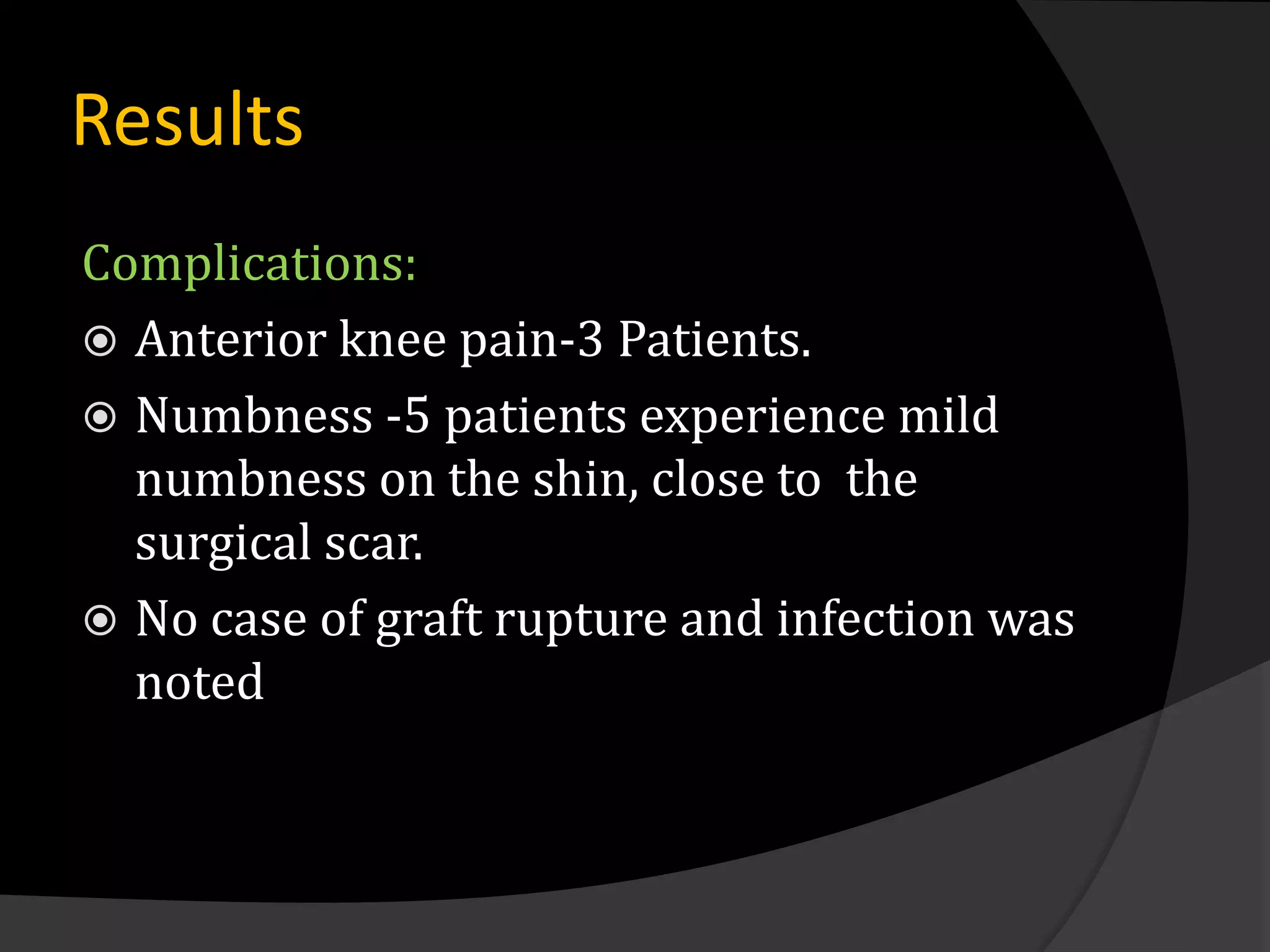
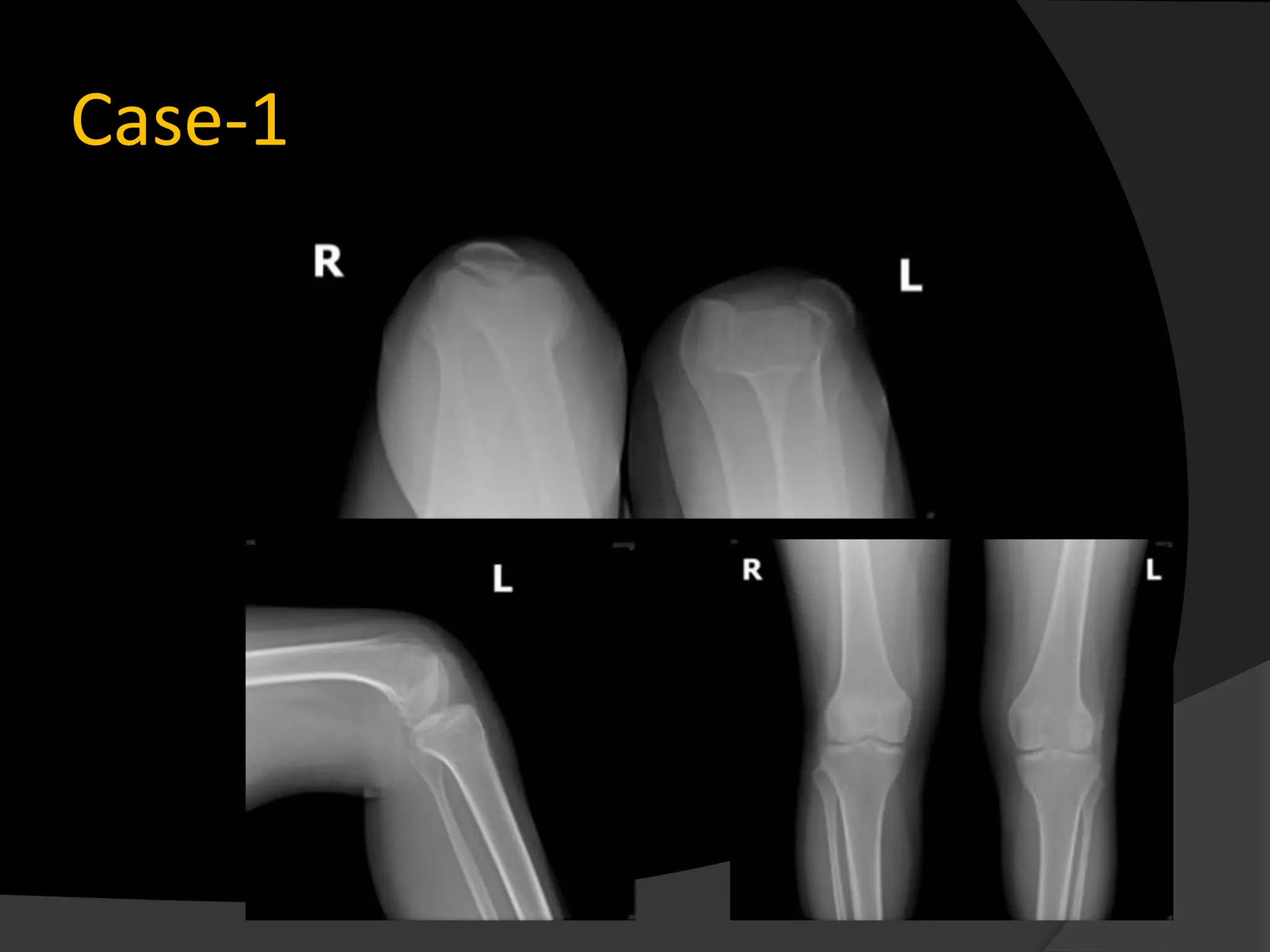
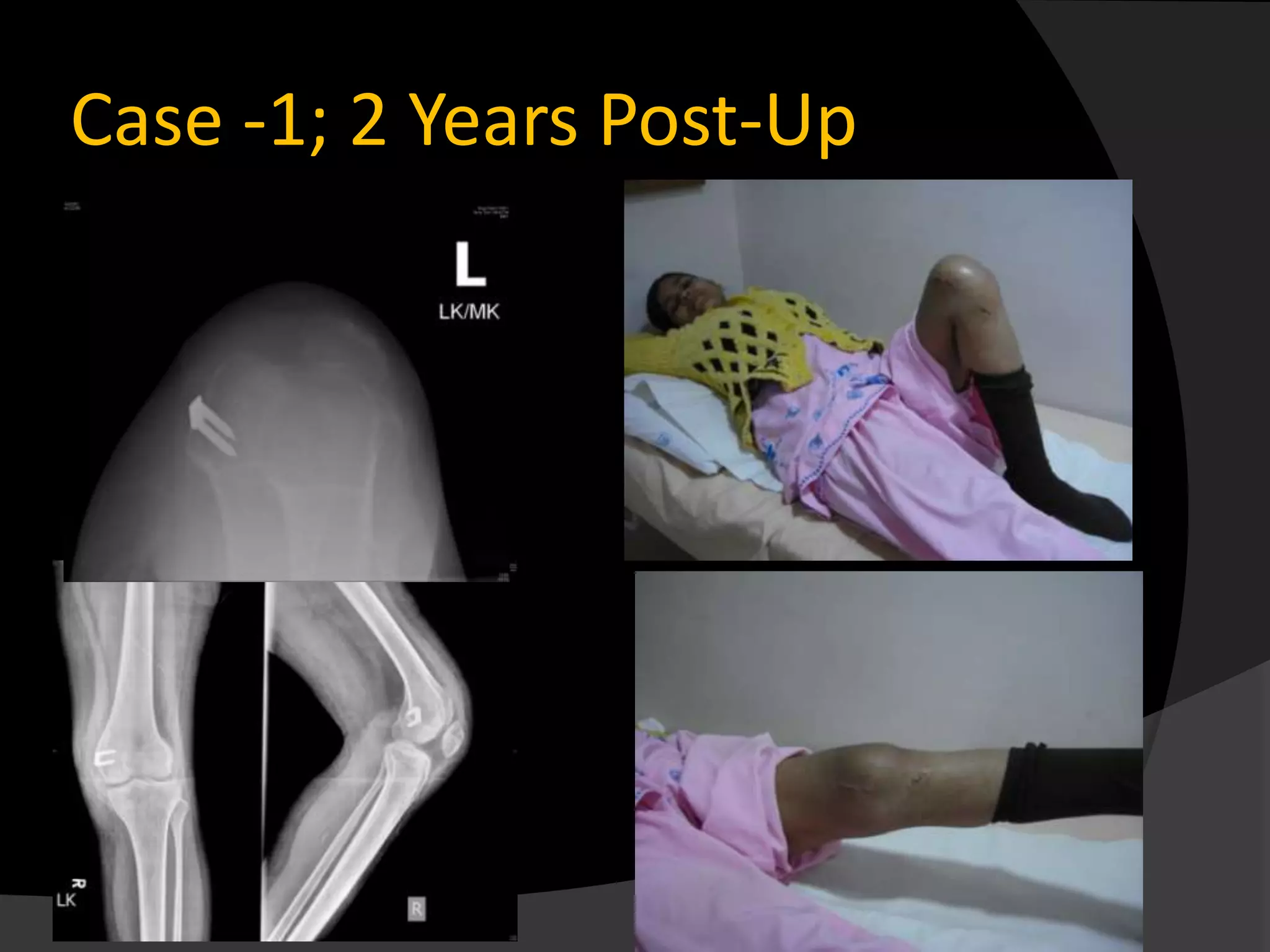
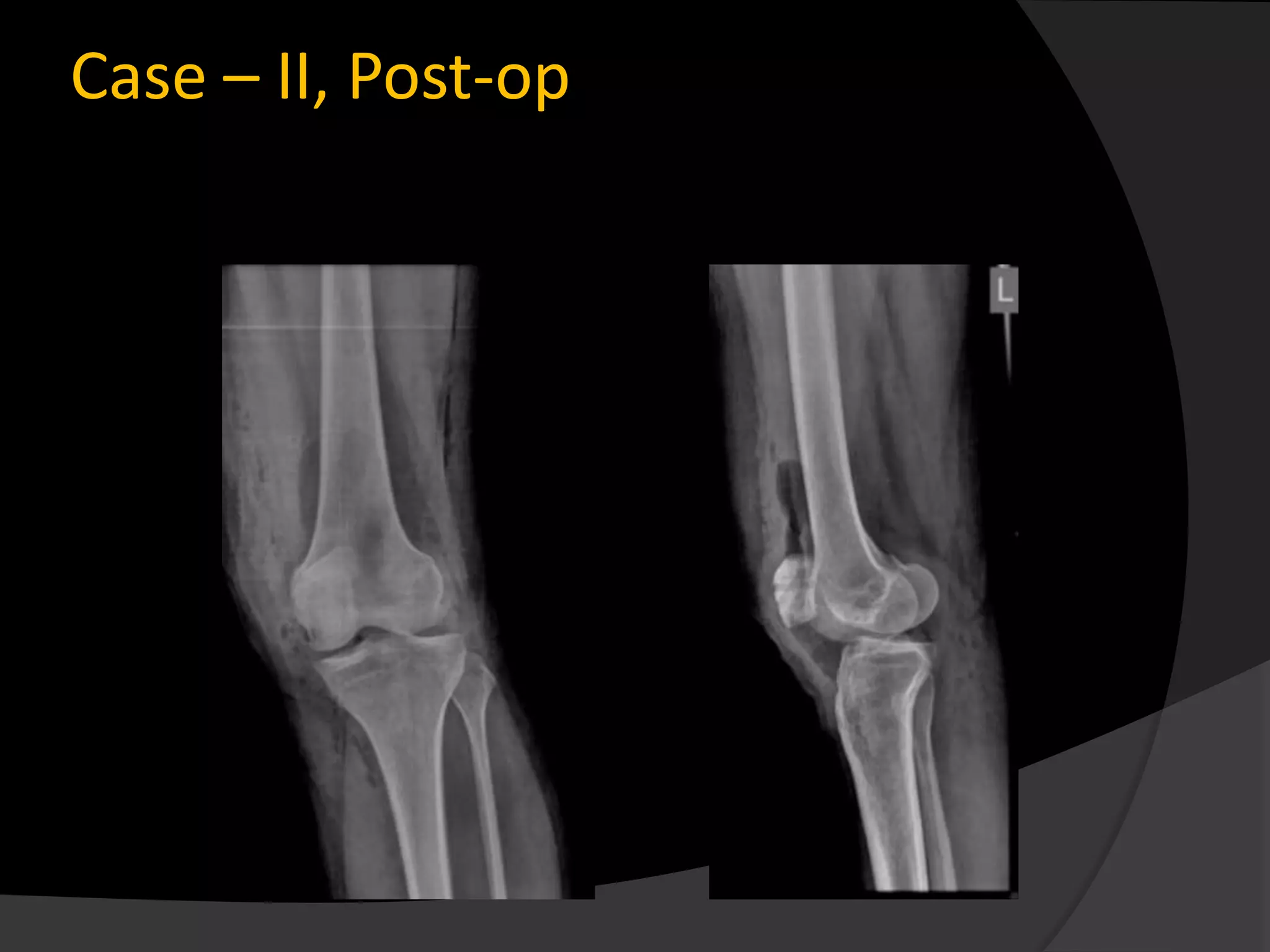
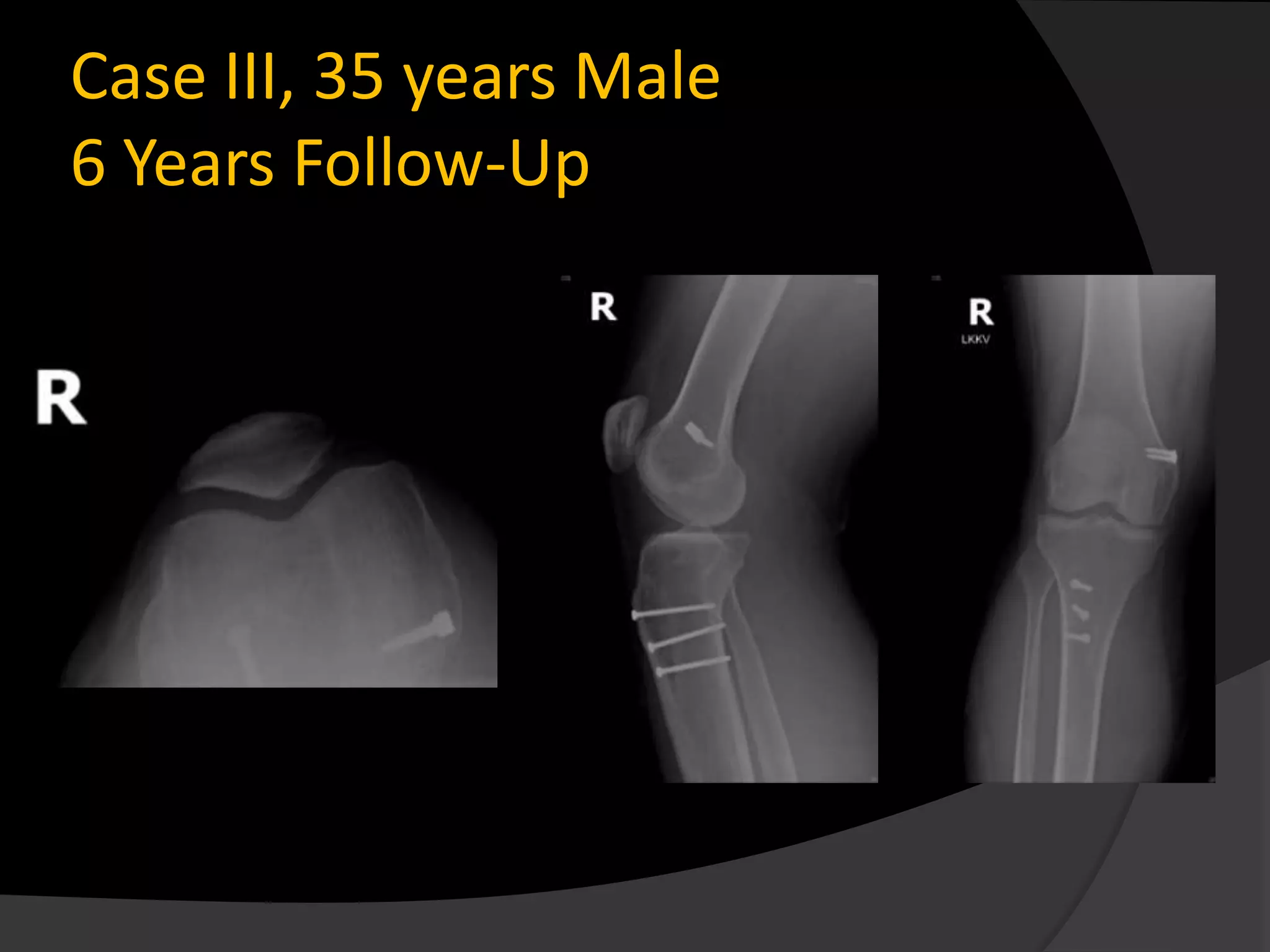
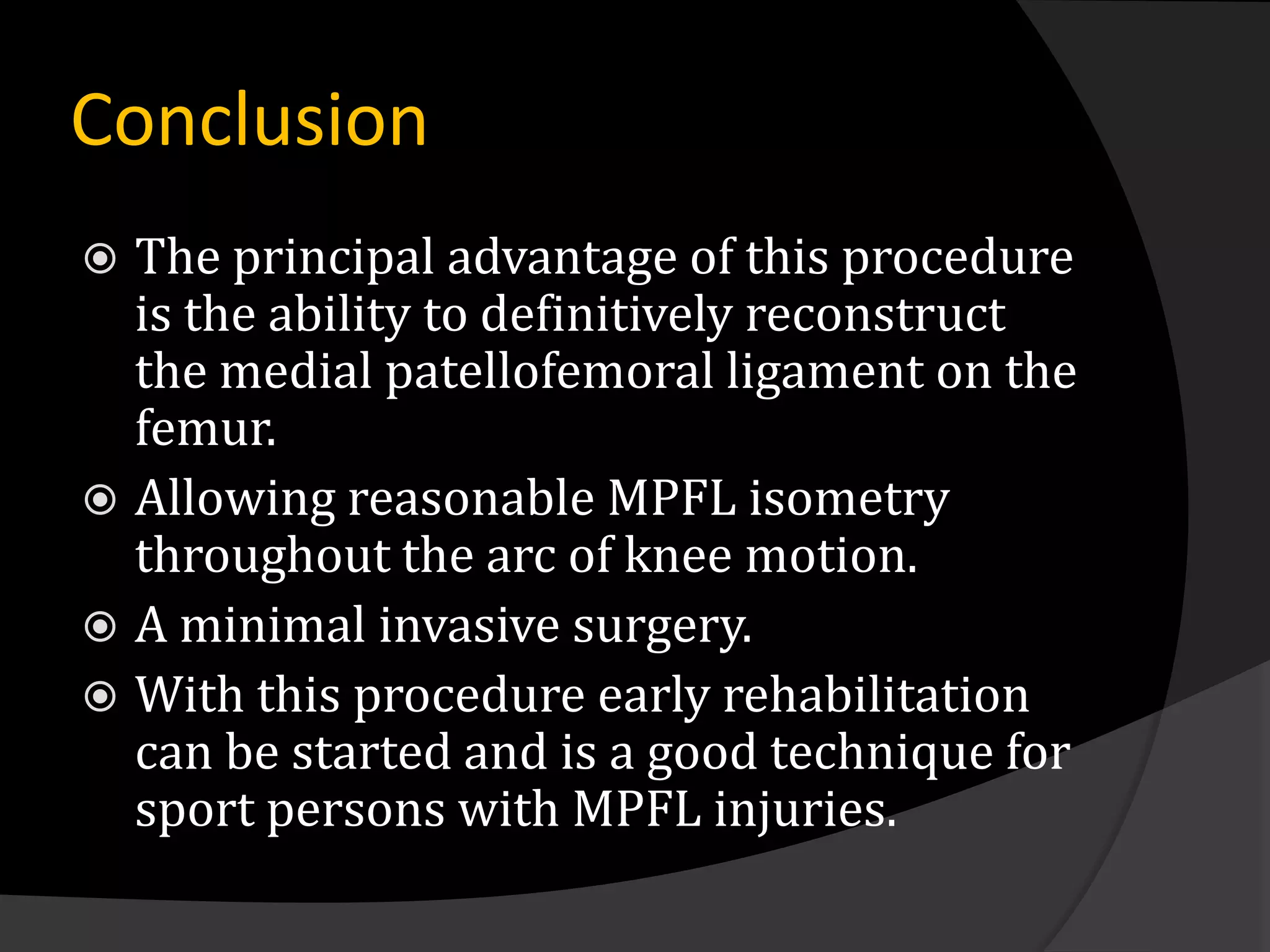
The document discusses patterns of patellar dislocation including recurrent dislocation, recurrent subluxation, and habitual dislocation. It then summarizes the anatomy and biomechanics of the medial patellofemoral ligament (MPFL), which is the primary soft tissue restraint preventing abnormal lateral displacement of the patella. Surgical reconstruction of the MPFL has gained popularity for treating recurrent patellar instability due to studies showing good postoperative outcomes with normalization of patellofemoral tracking and no recurrence of instability. The document presents the technique and results for MPFL reconstruction in 14 patients with patellar instability.