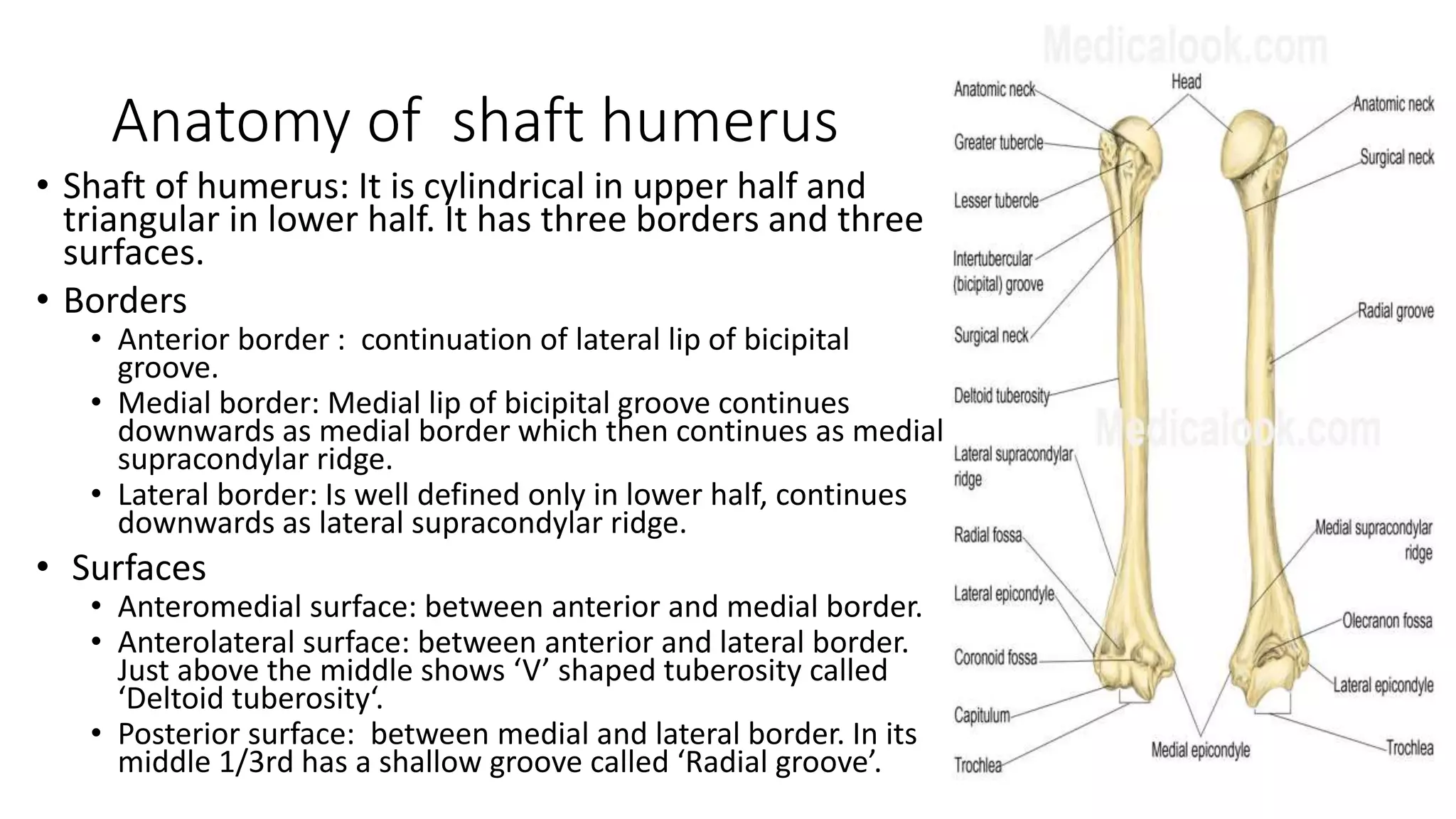
The document discusses fractures of the humerus that are complicated by radial nerve injury. It begins by describing the anatomy of the humerus shaft and radial nerve. Radial nerve injuries are common with humerus fractures due to the nerve's close proximity in the spiral groove. Management involves classifying the nerve injury and addressing the fracture. Early exploration of the nerve is recommended in certain cases like open fractures or secondary nerve palsy. Surgical options for nerve repair include neurography, nerve grafting, and tendon transfers depending on factors like injury location and duration.