The document discusses the parasympathetic nervous system and parasympathomimetic drugs. It provides details on:
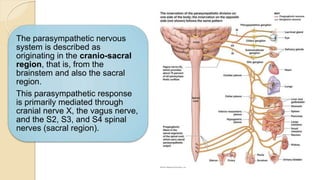
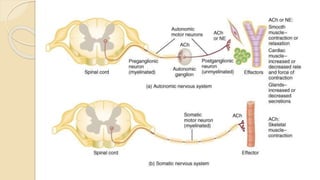
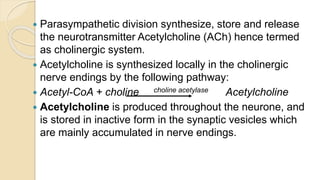
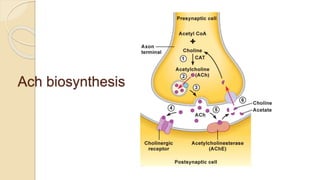
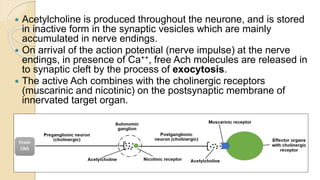
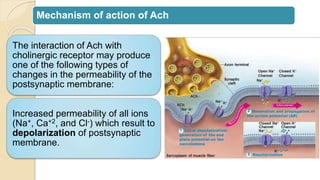
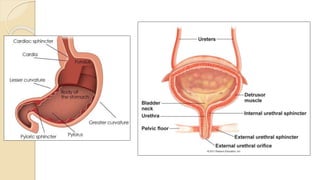
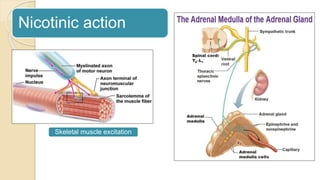
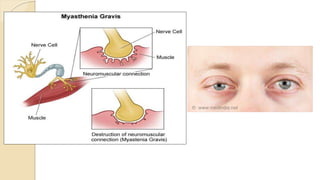
- The parasympathetic nervous system originates from the brainstem and sacral region and uses acetylcholine as a neurotransmitter.
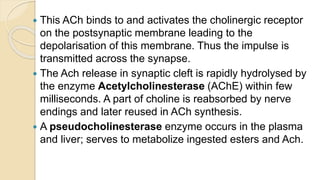
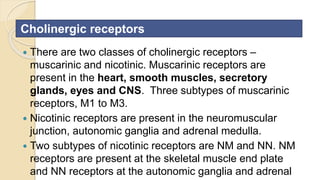
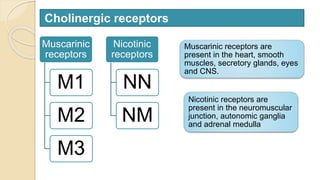
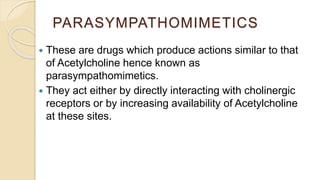
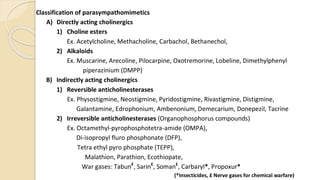
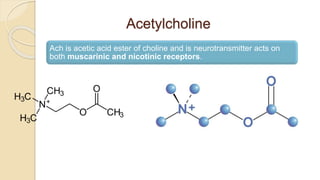
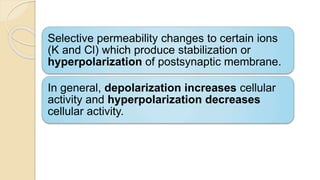
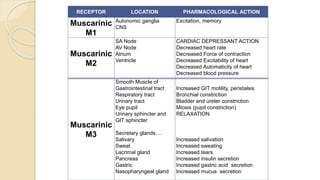
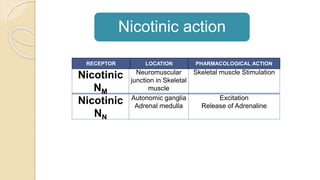
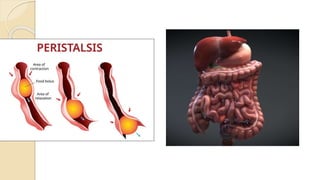
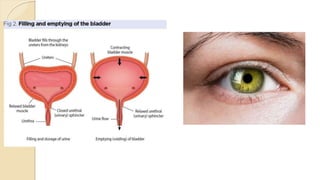
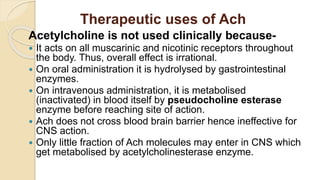
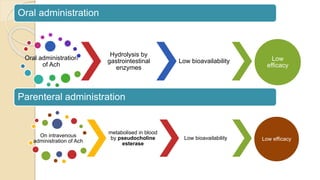
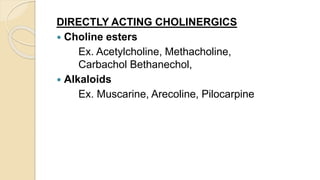
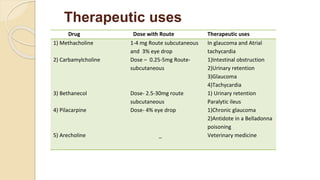
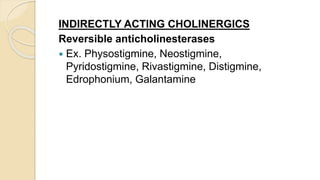
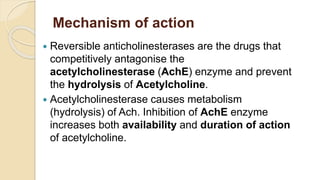
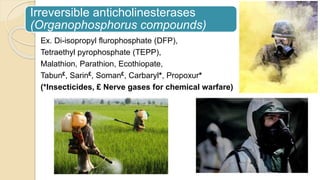
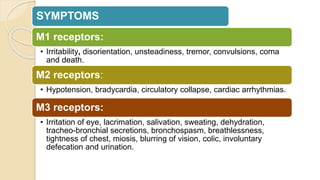
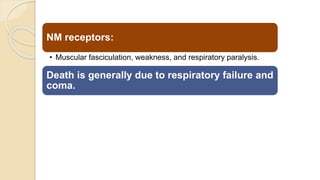
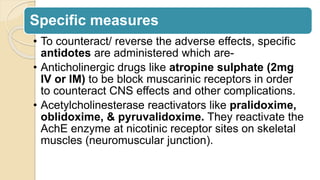
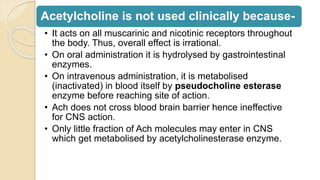
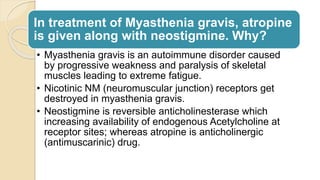
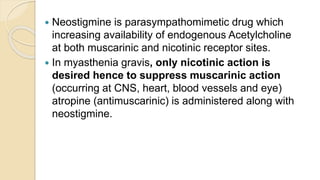
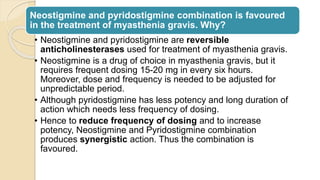
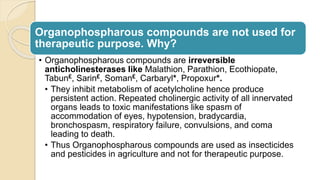
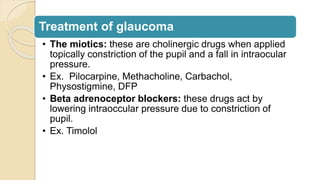
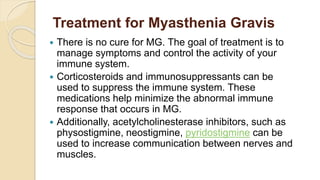
- Parasympathomimetic drugs like acetylcholine, muscarine, and anticholinesterases act to stimulate parasympathetic responses. Direct acting drugs activate cholinergic receptors while indirect drugs inhibit acetylcholinesterase.
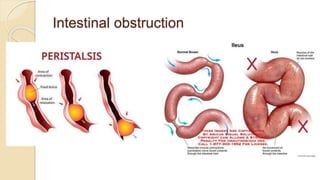
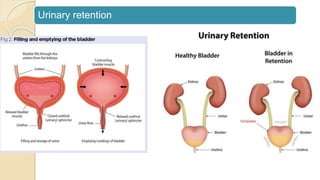
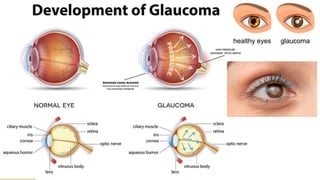
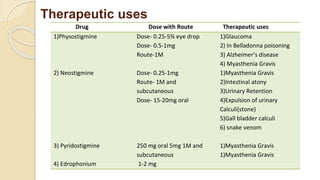
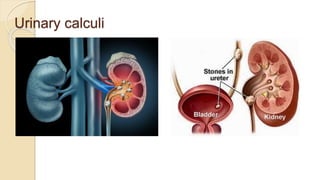
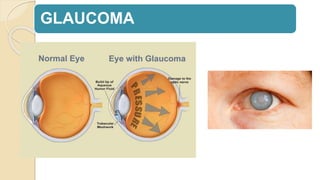
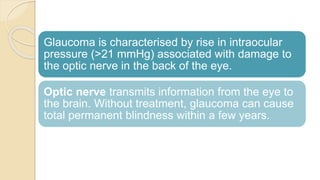
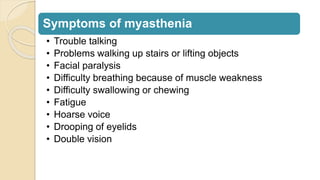
- These drugs have therapeutic uses for conditions like glaucoma, urinary retention, and myasthenia gravis. Combinations of drugs are sometimes used to achieve optimal effects while minimizing side effects.