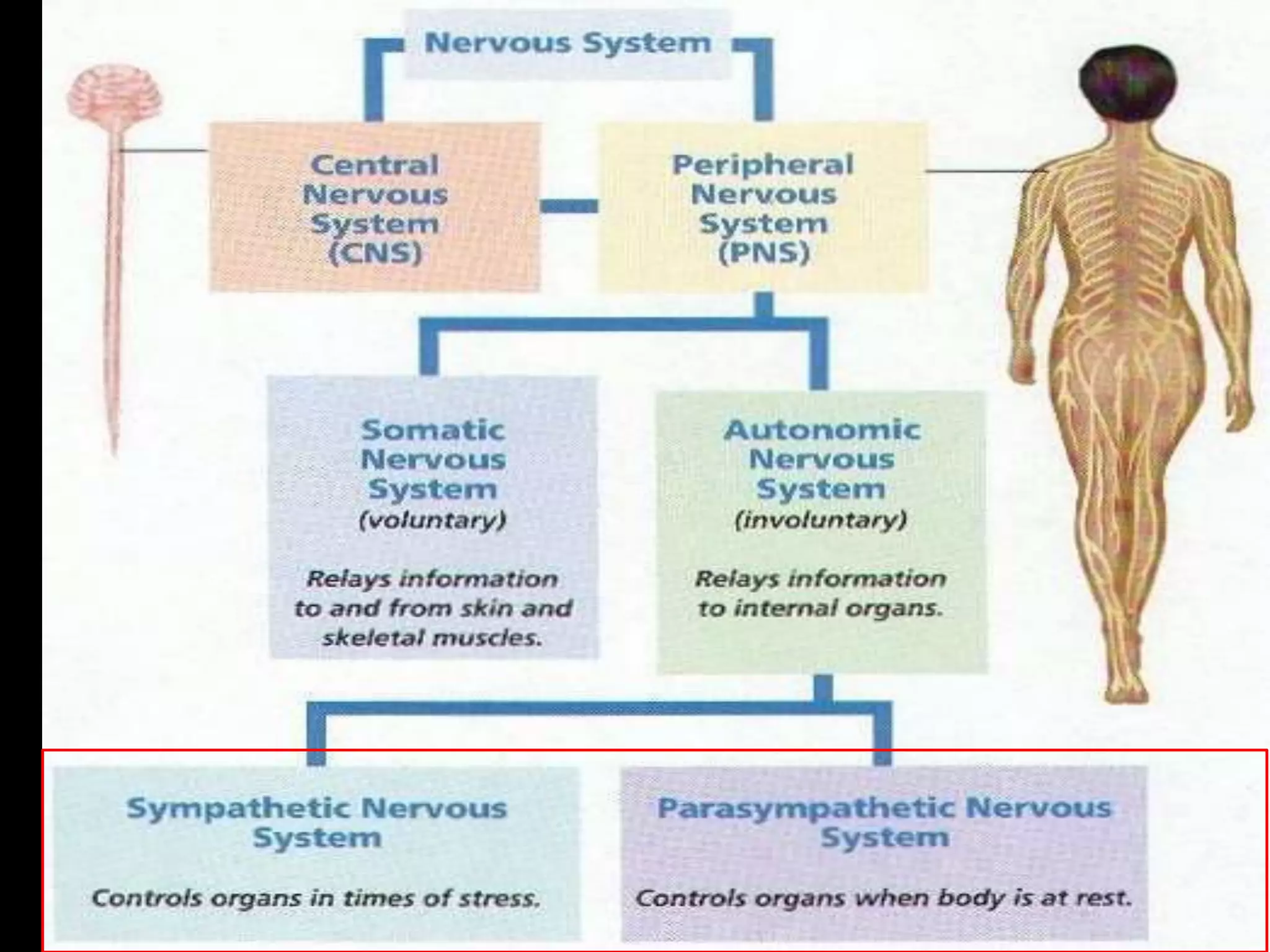
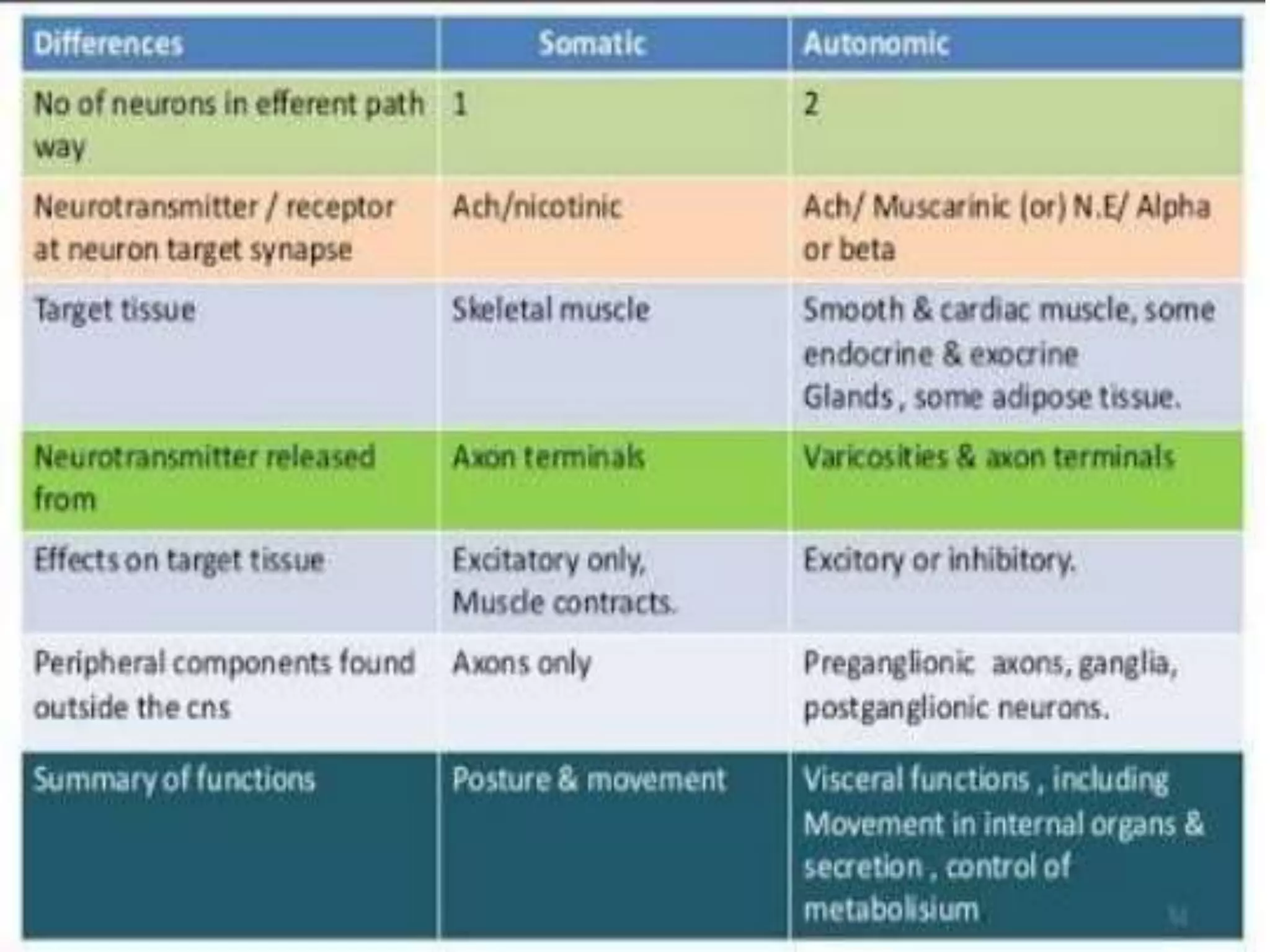
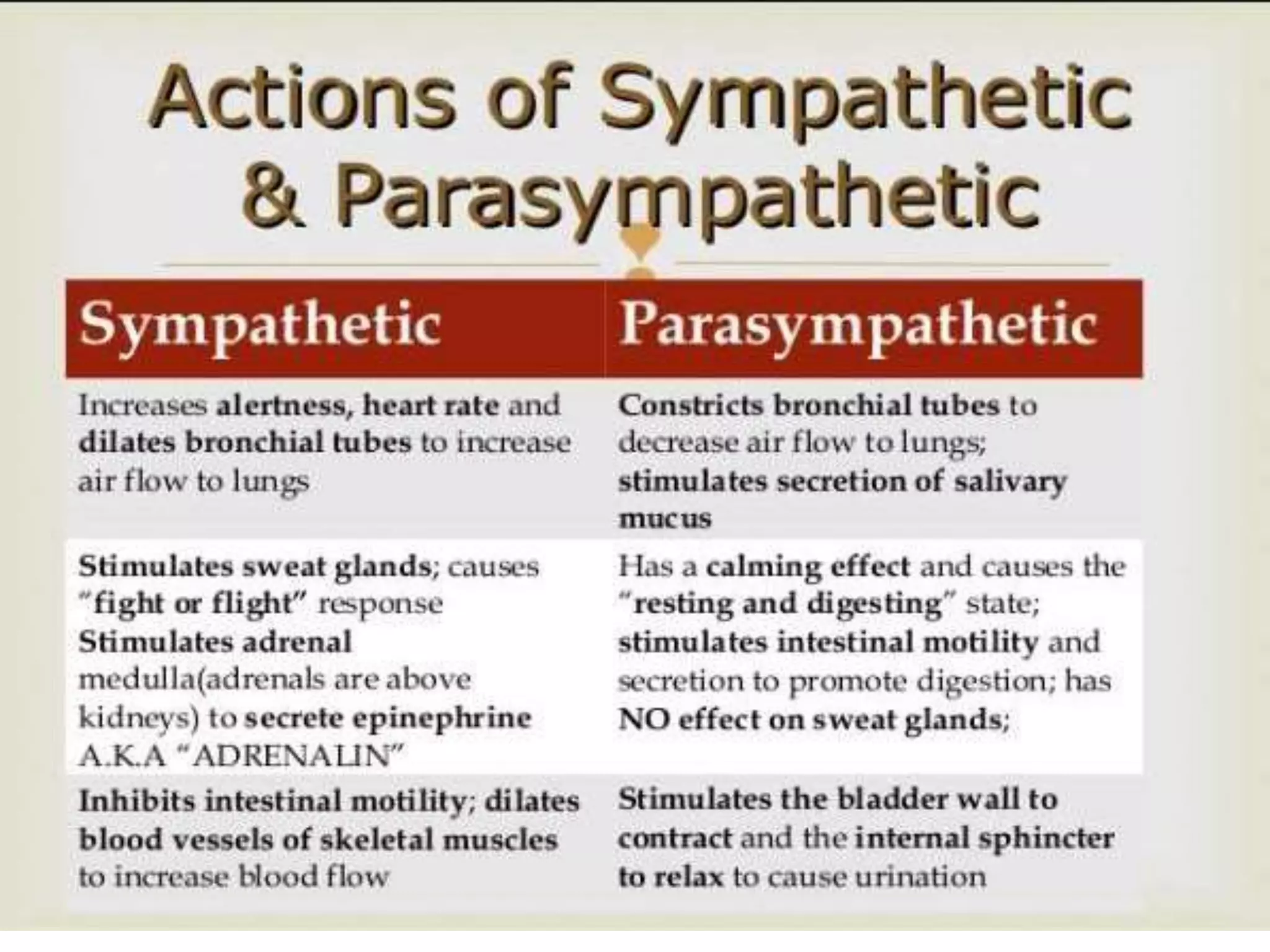
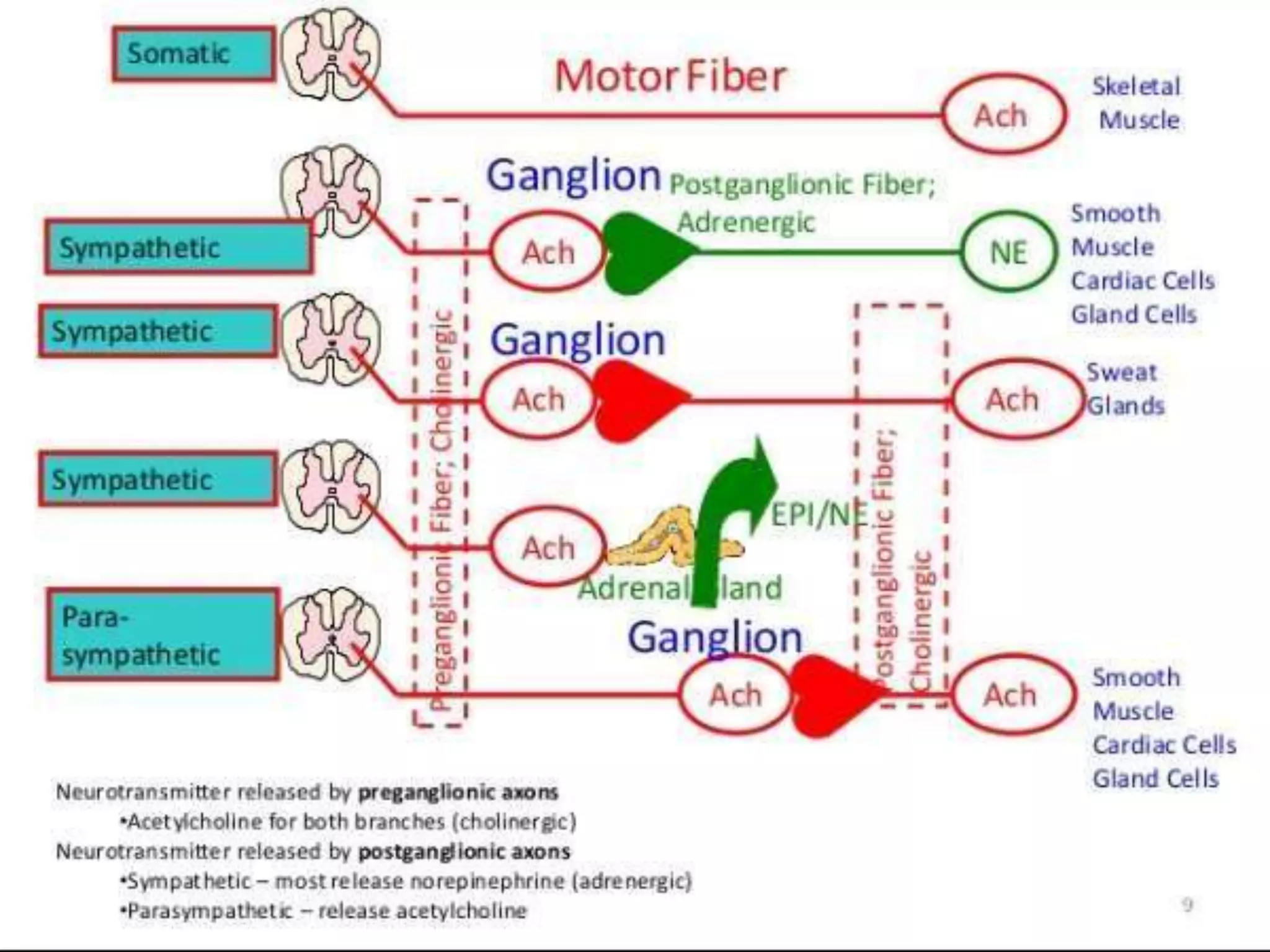
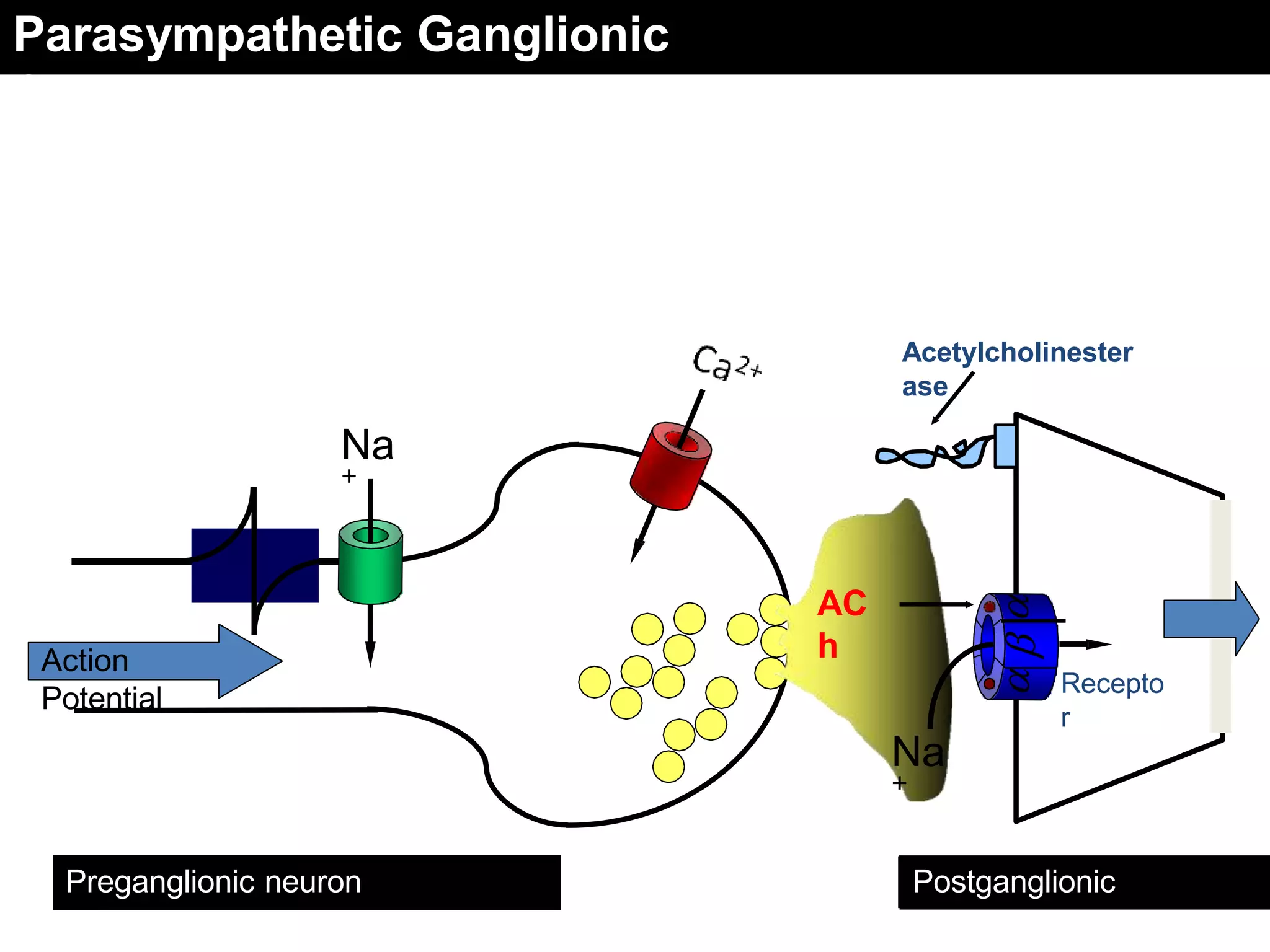
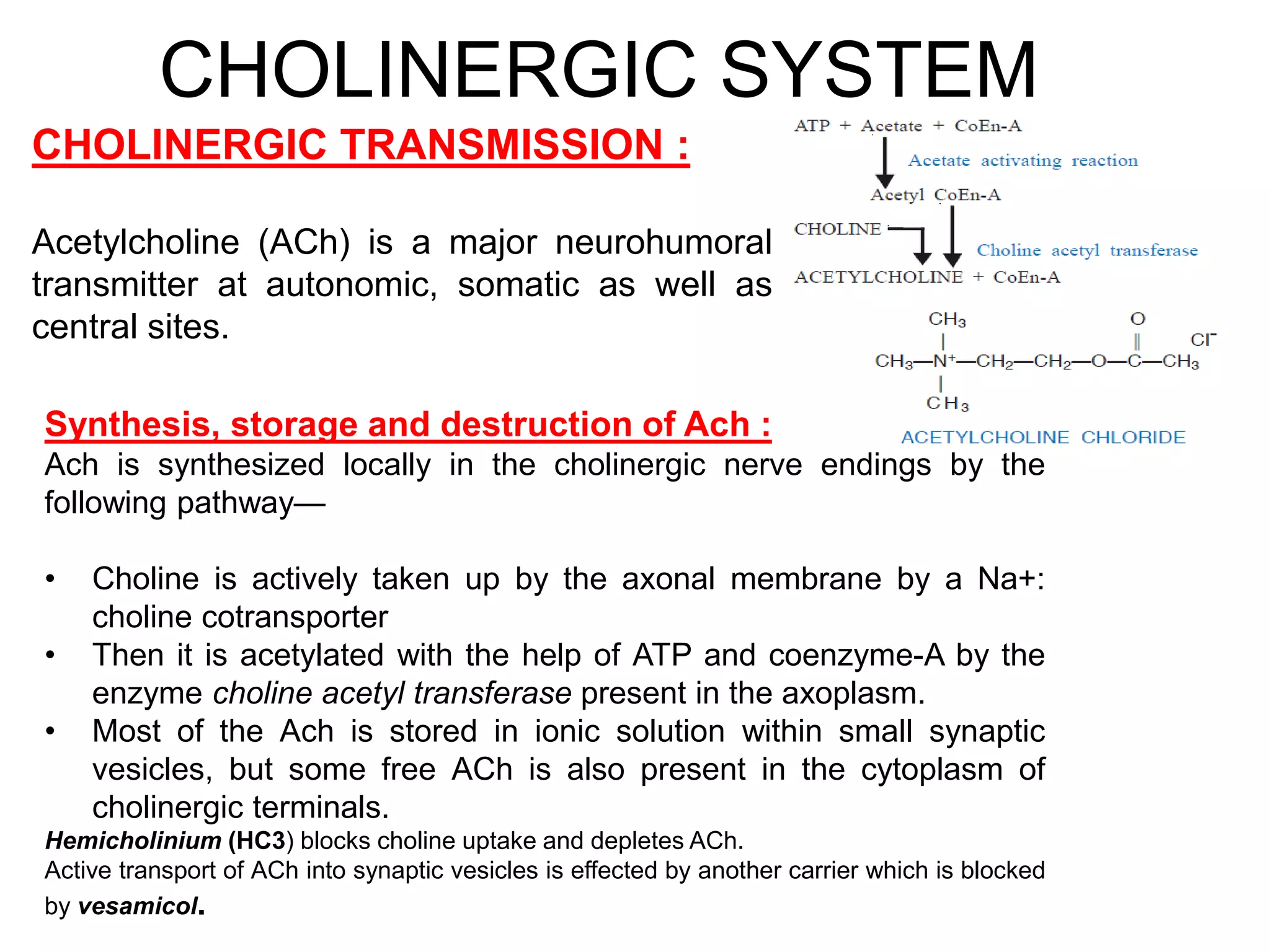
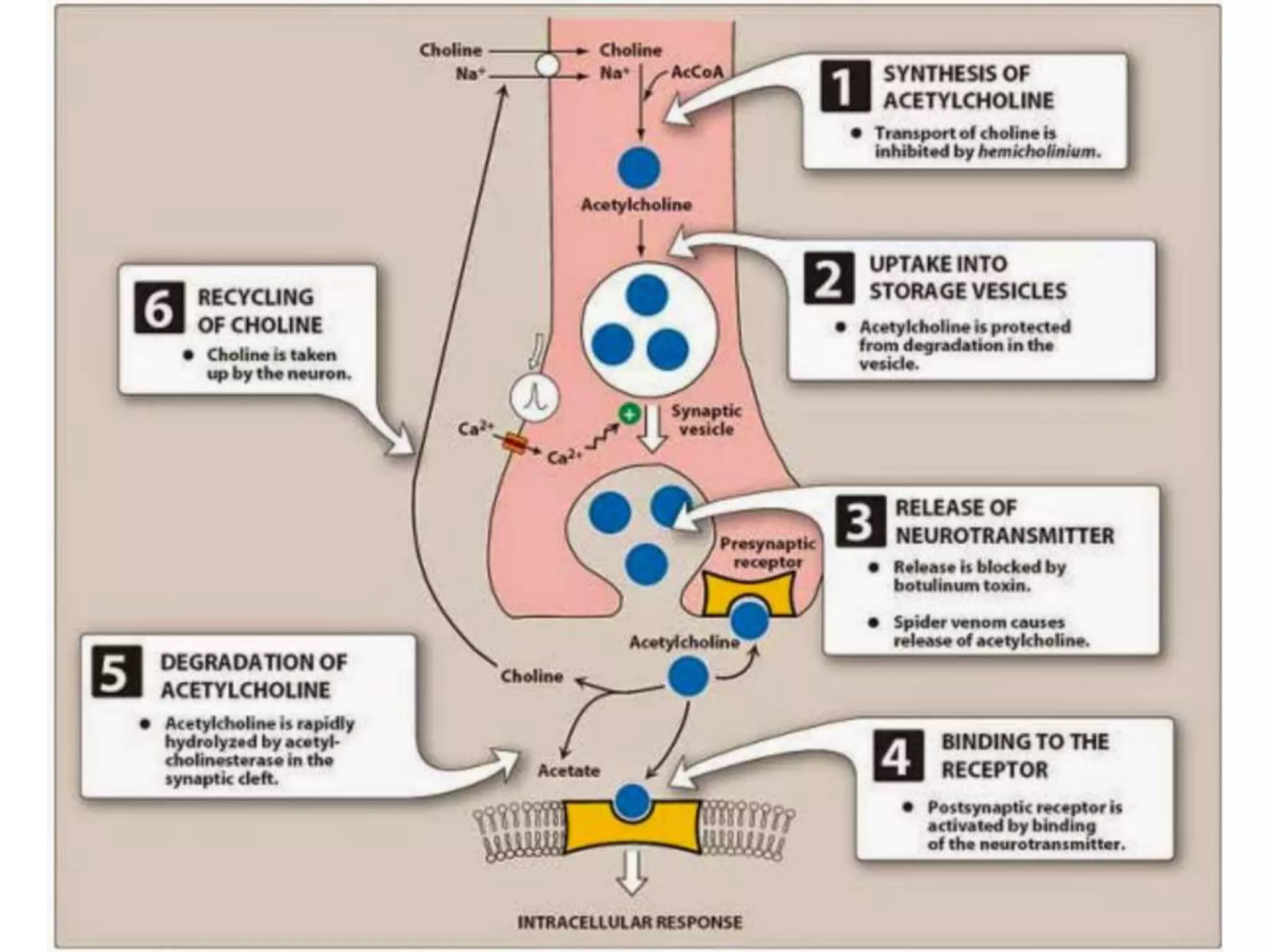
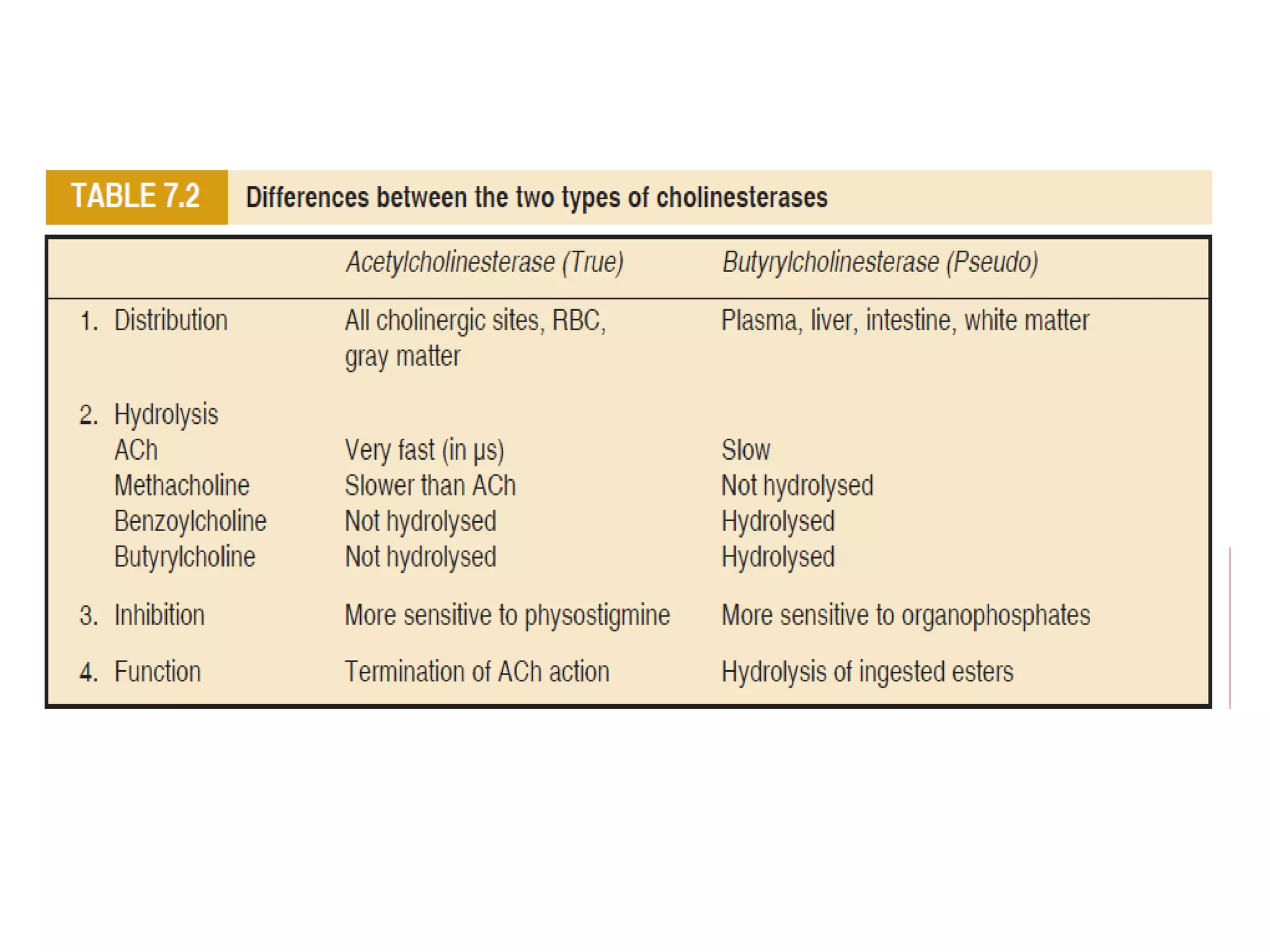
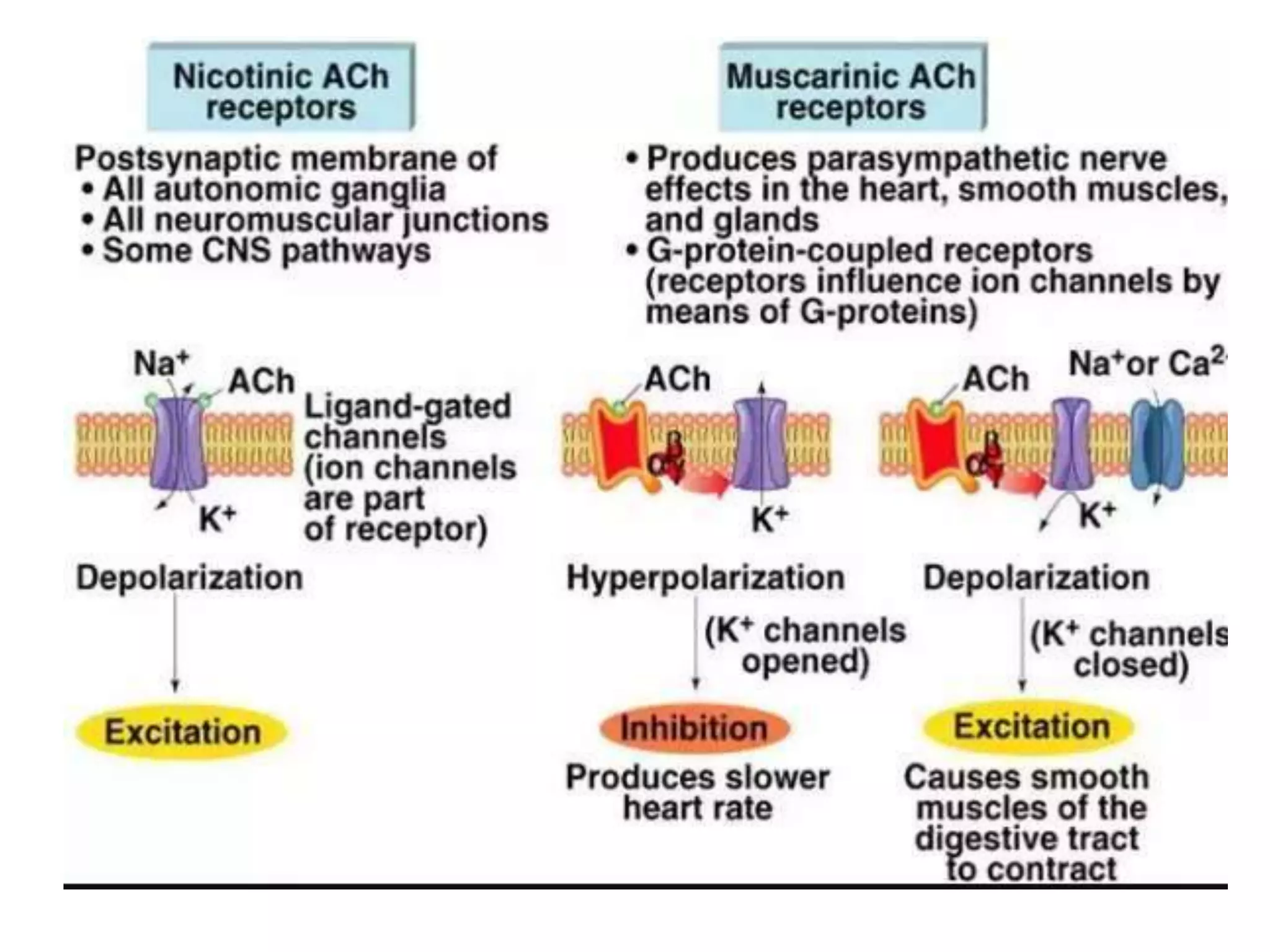
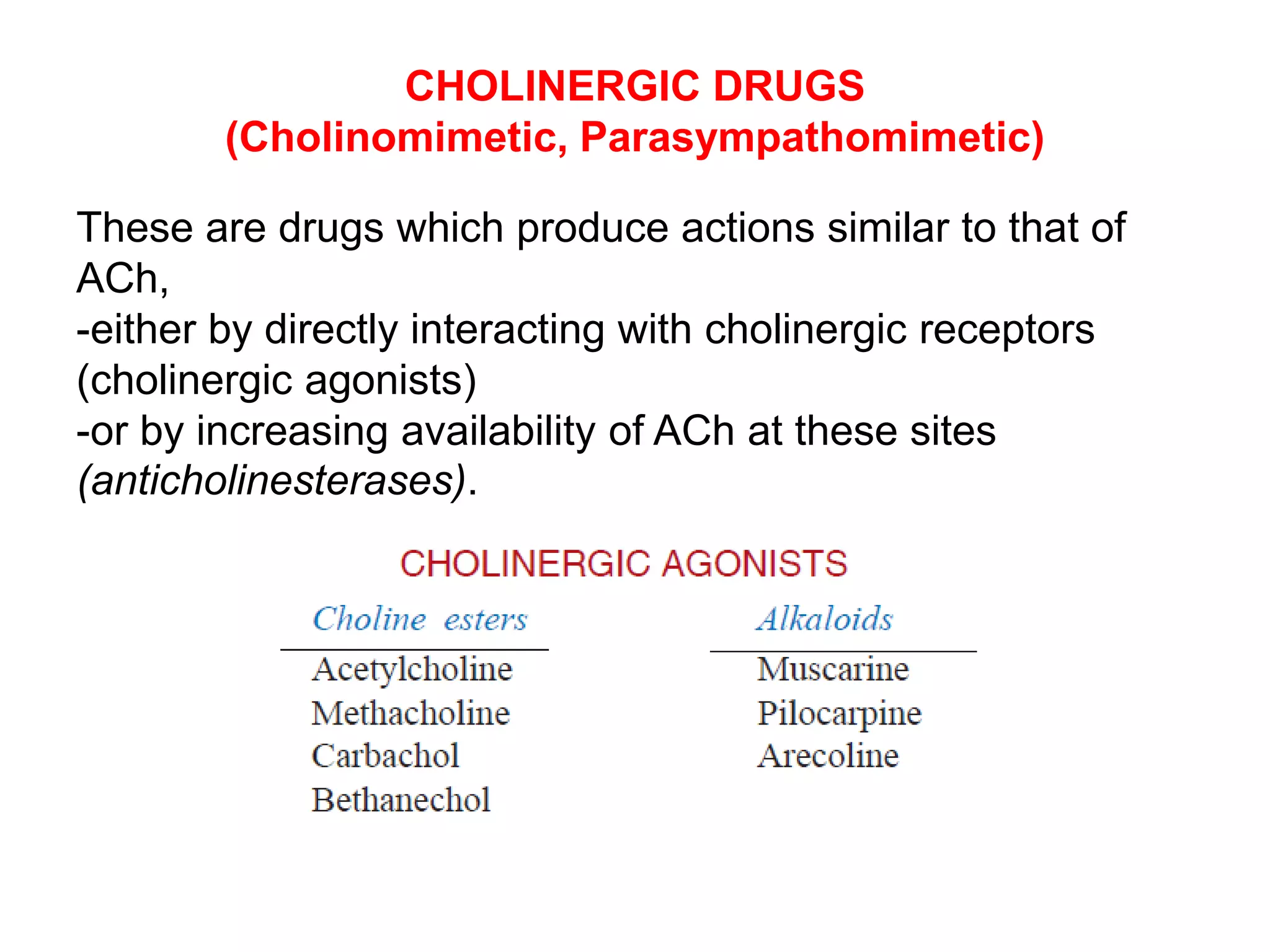
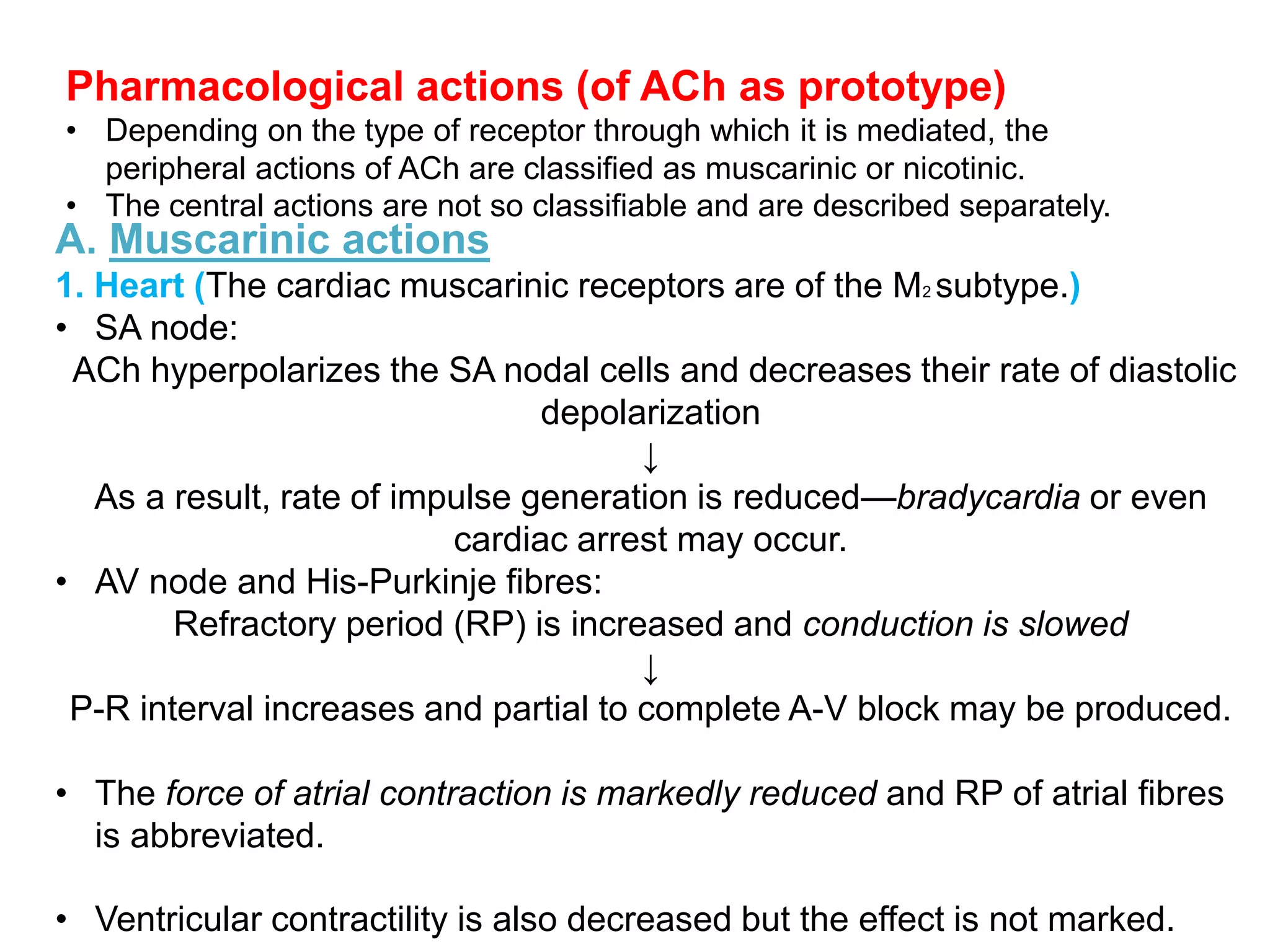
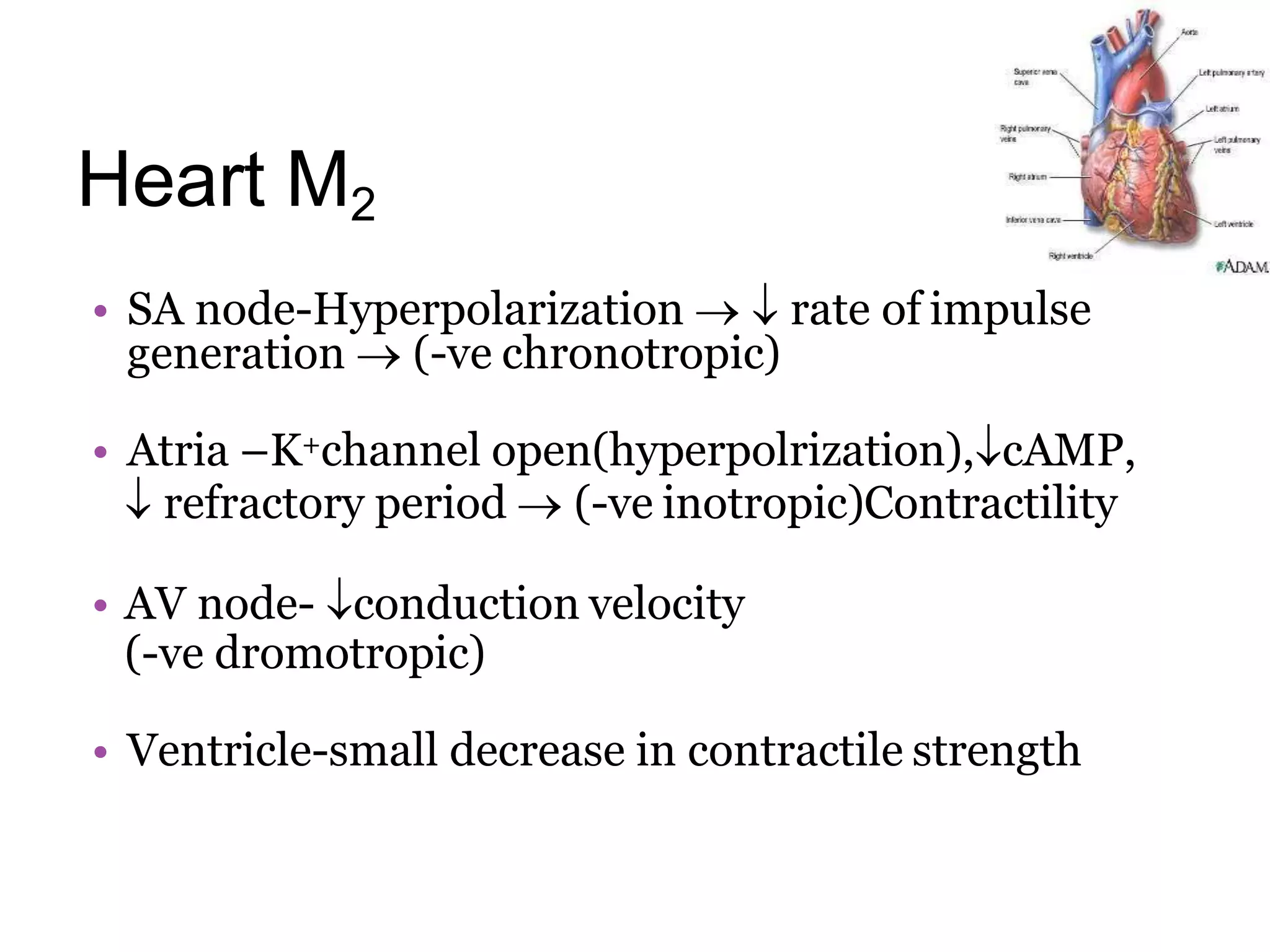
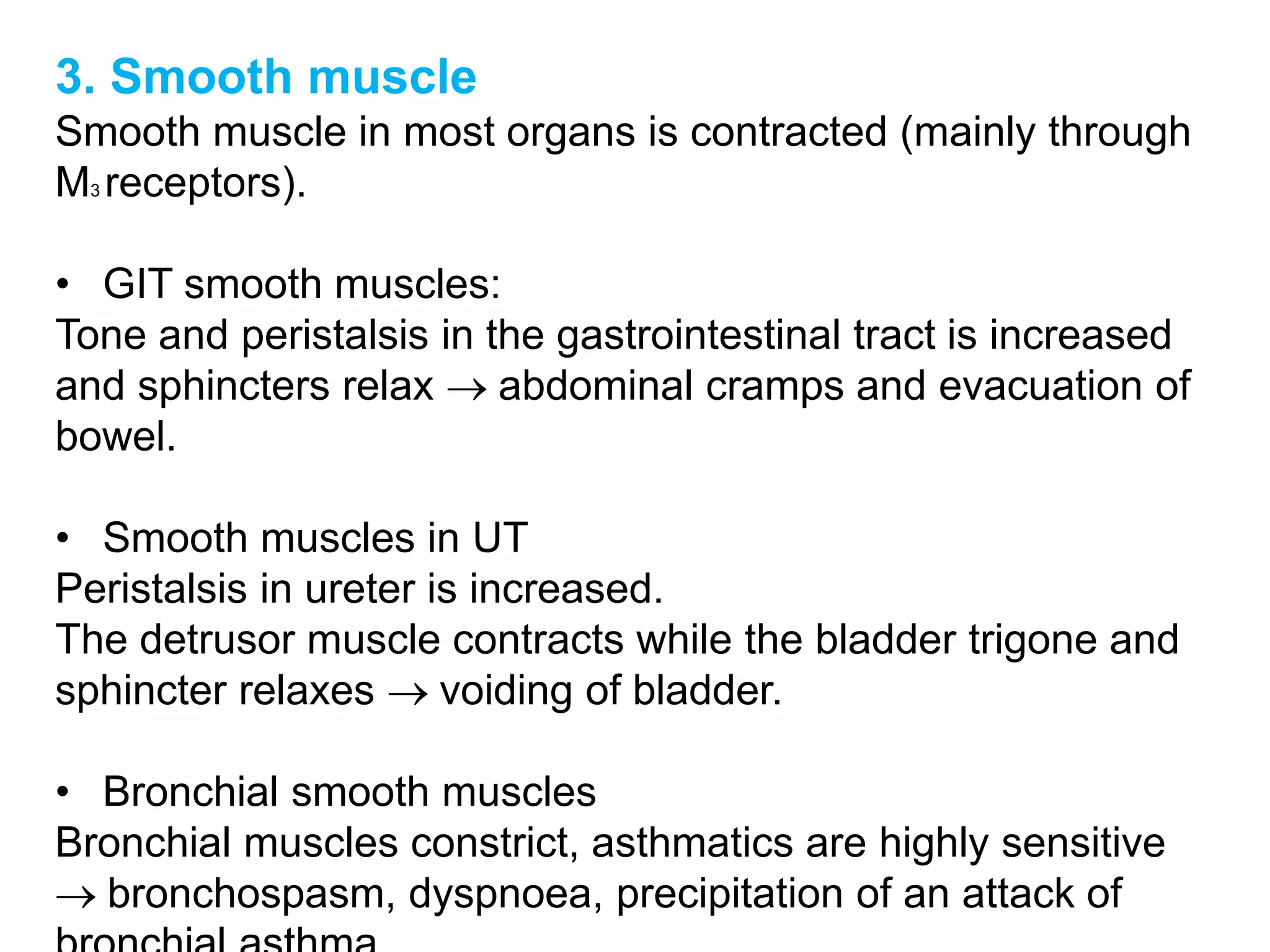
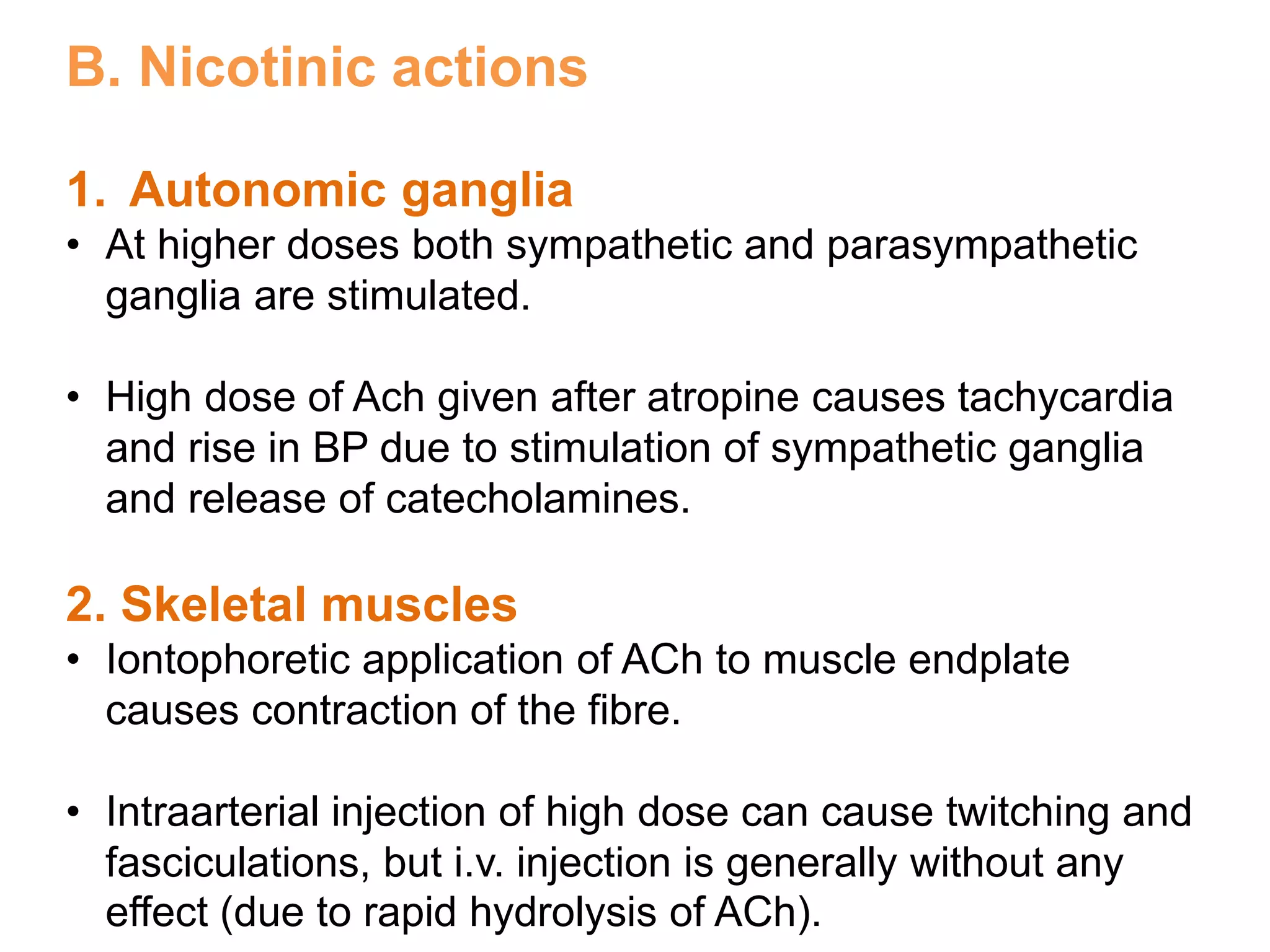
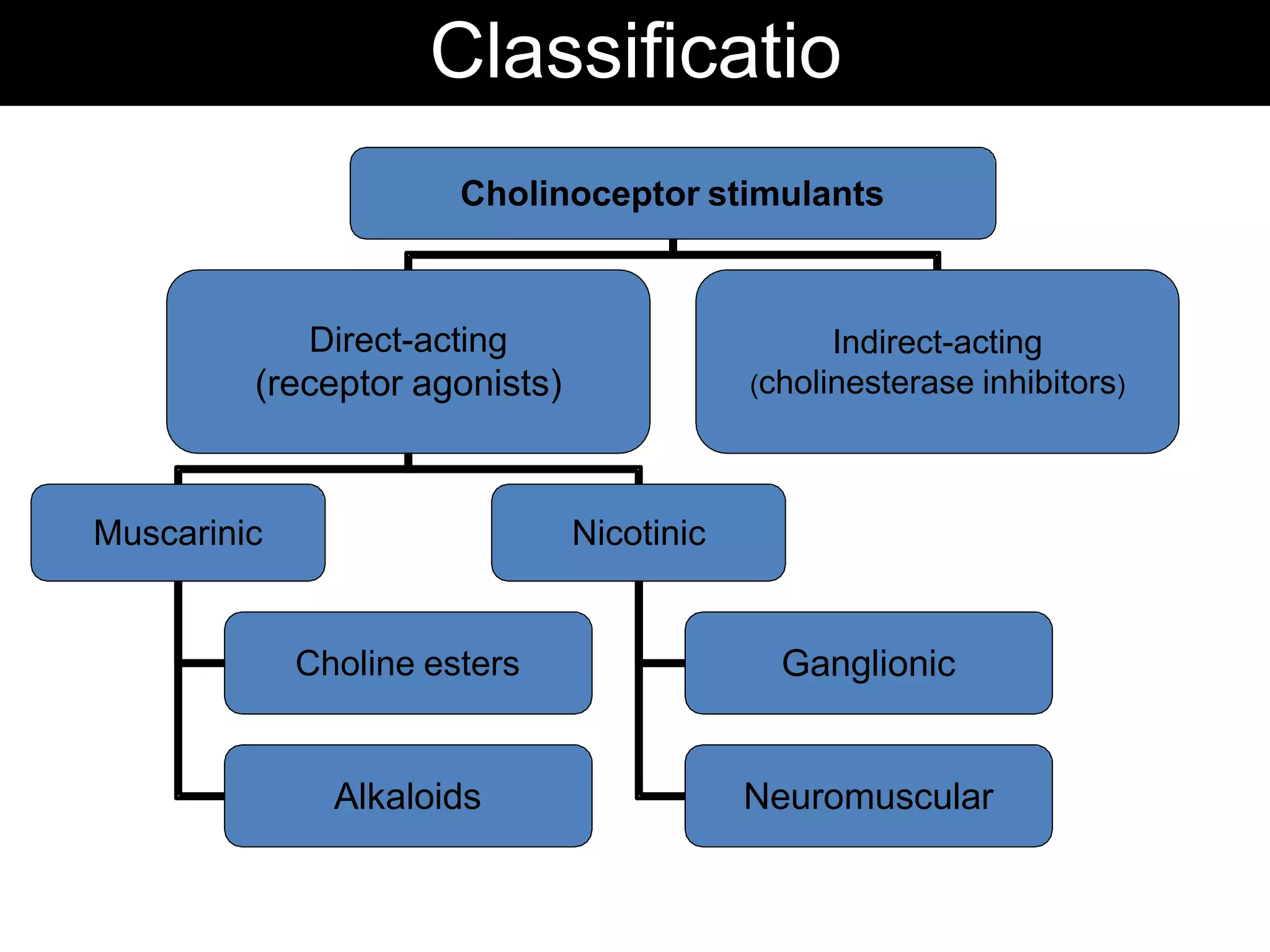
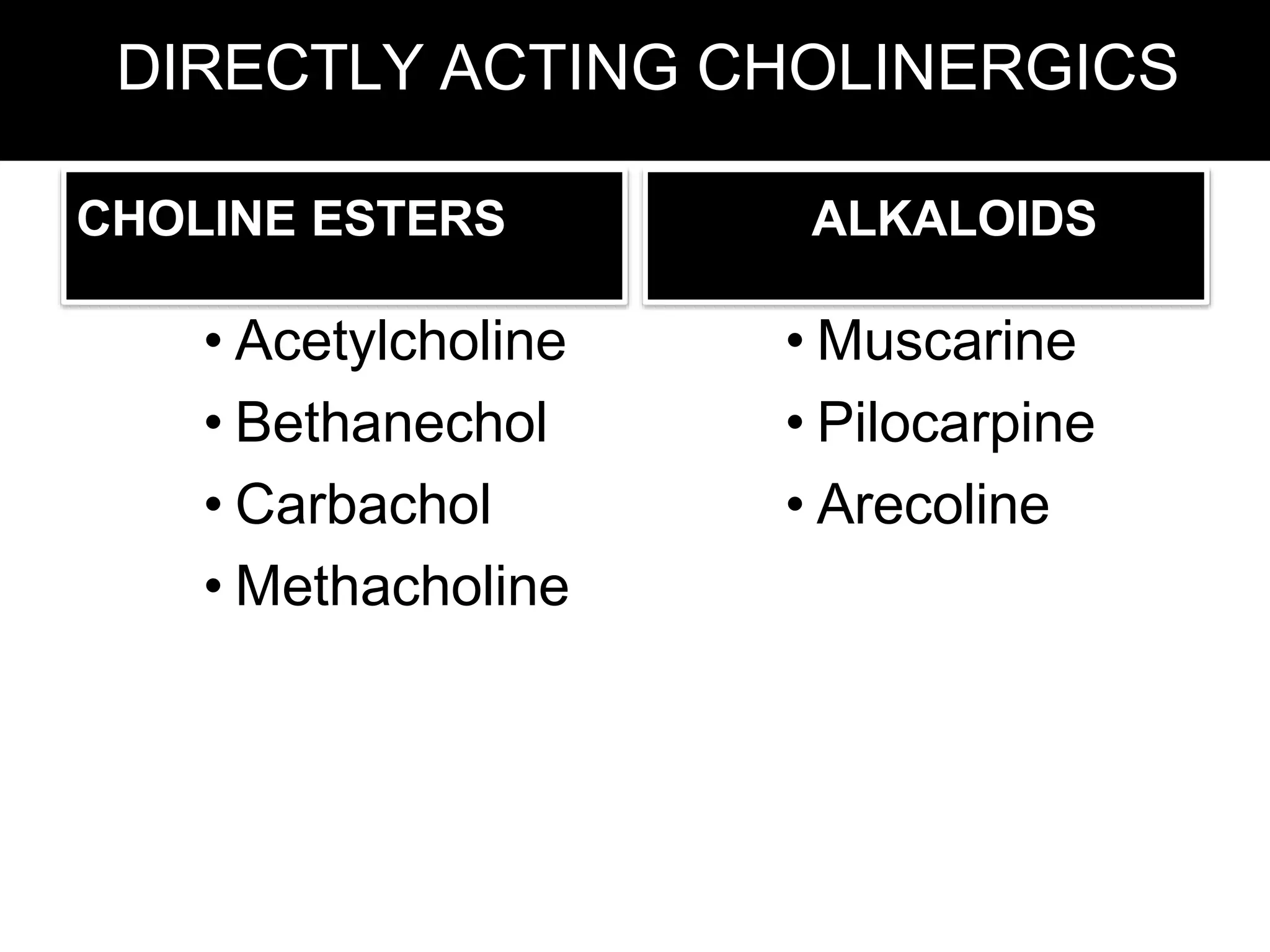
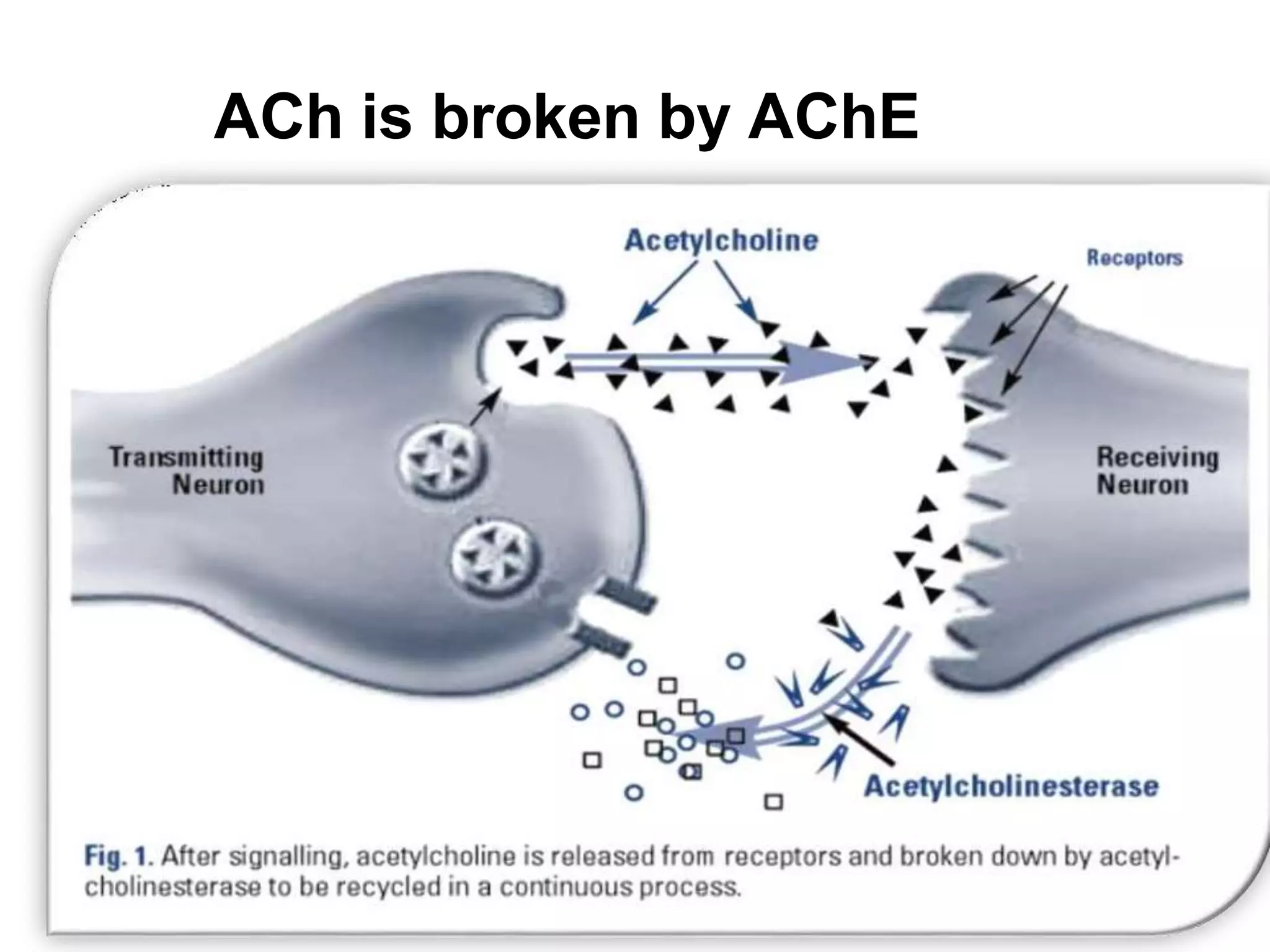
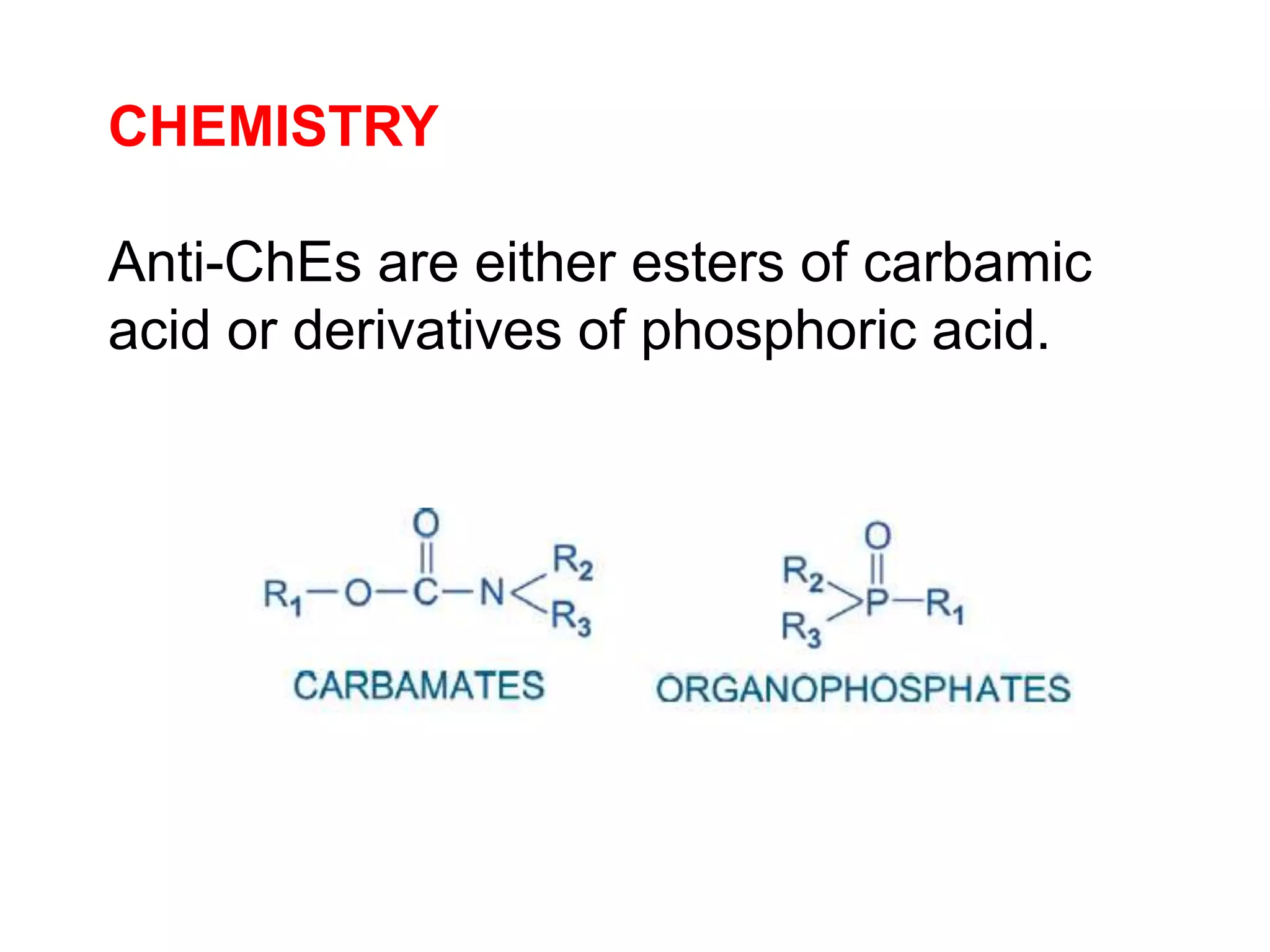
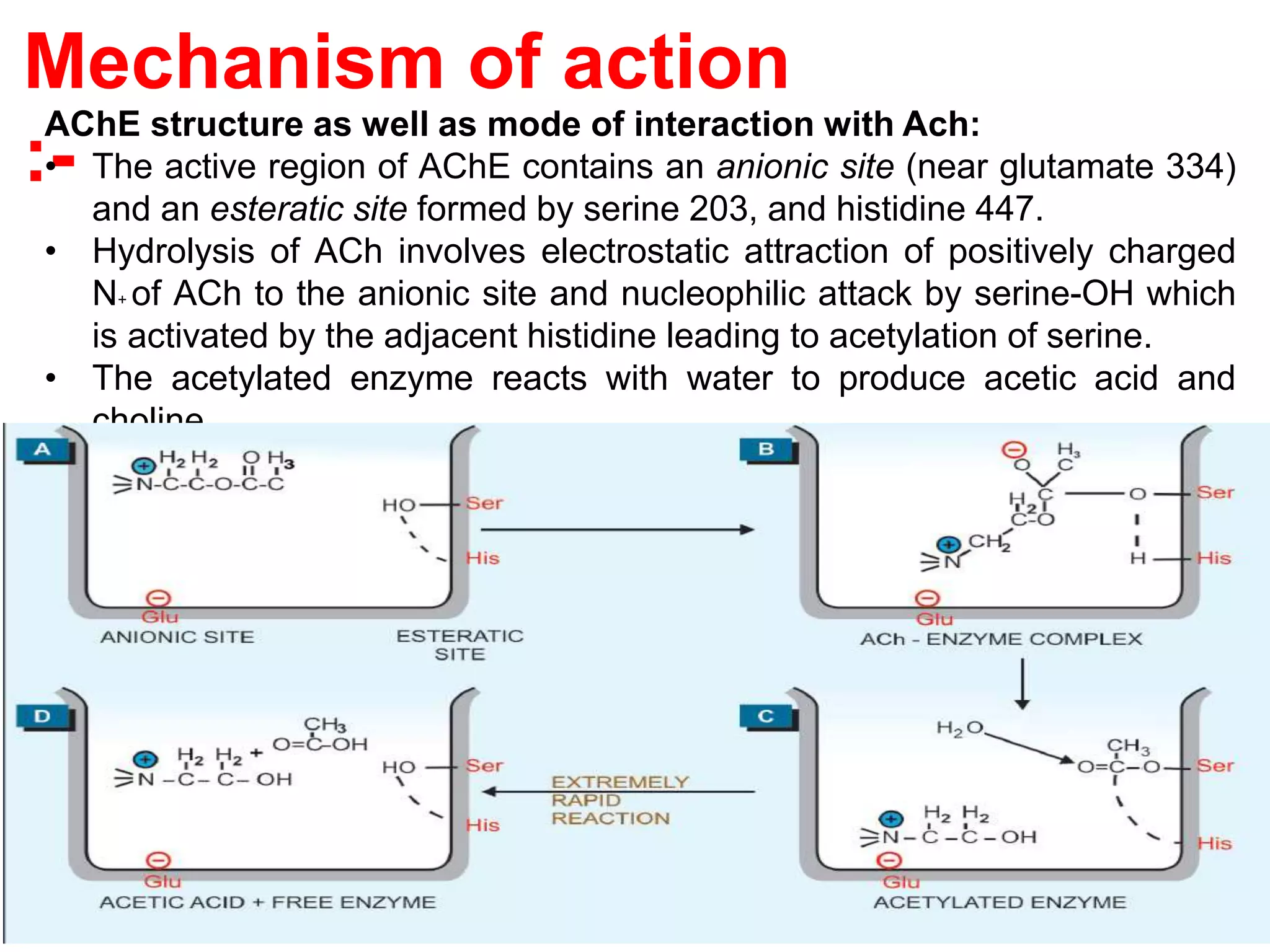
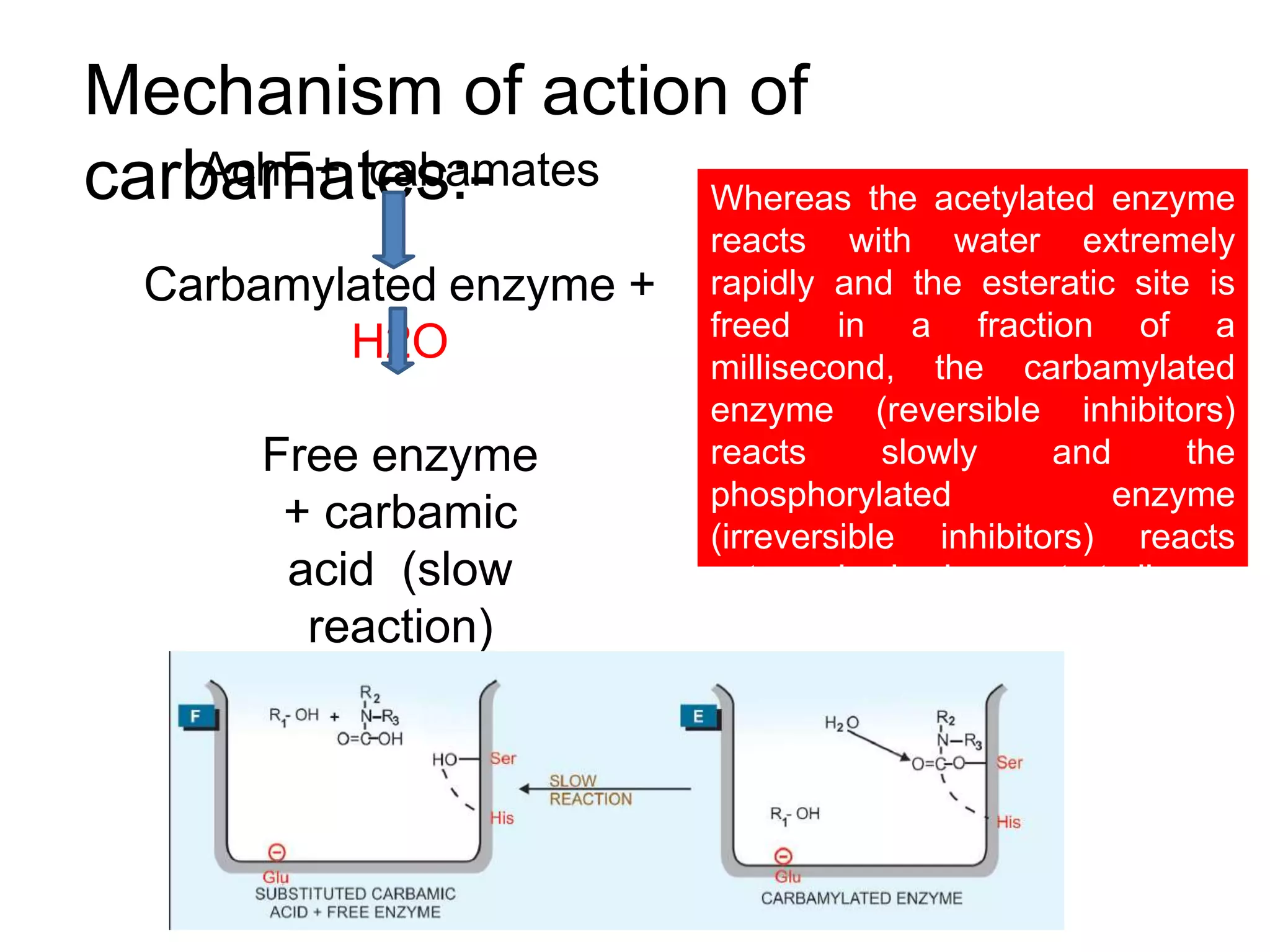
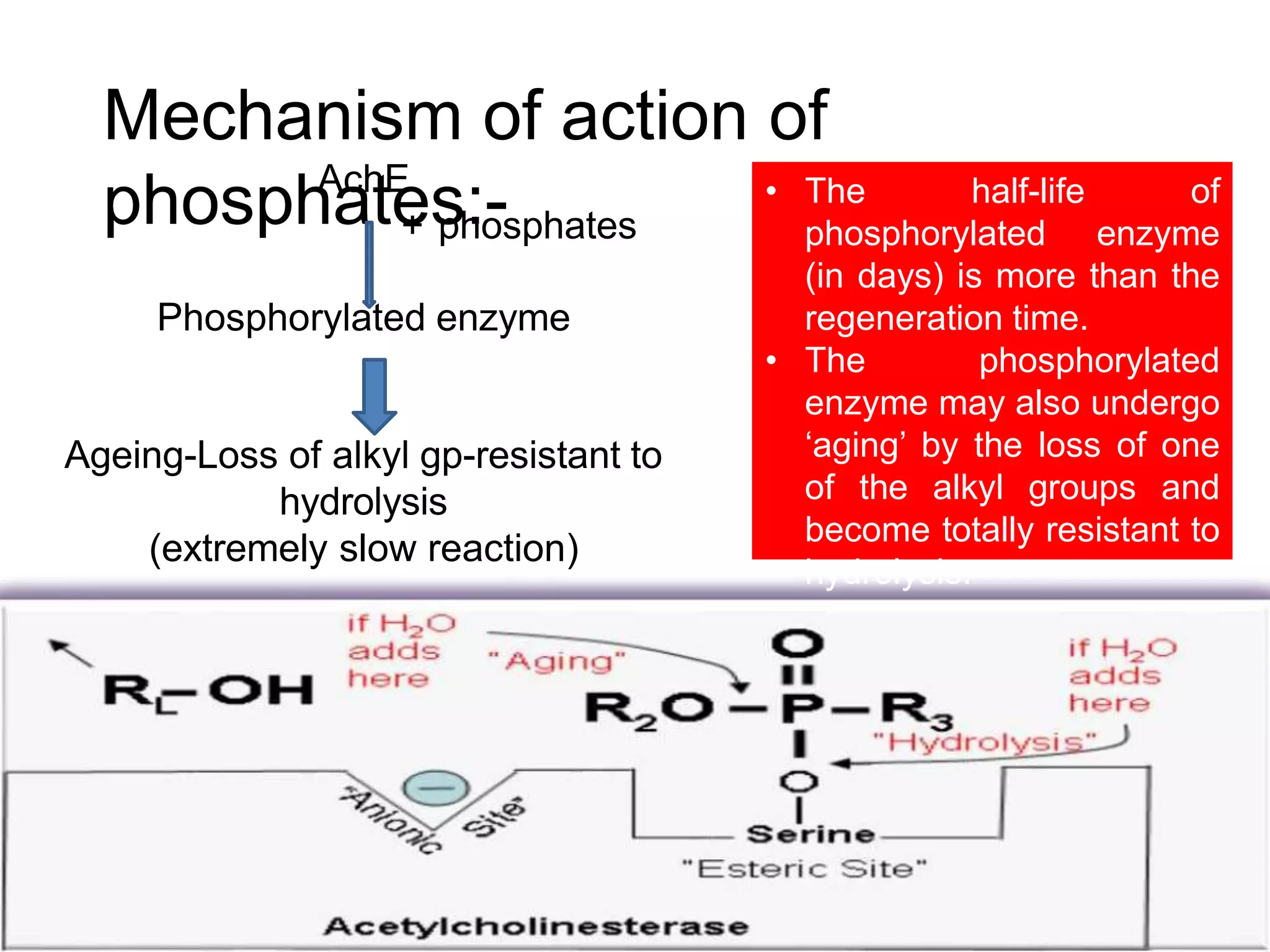
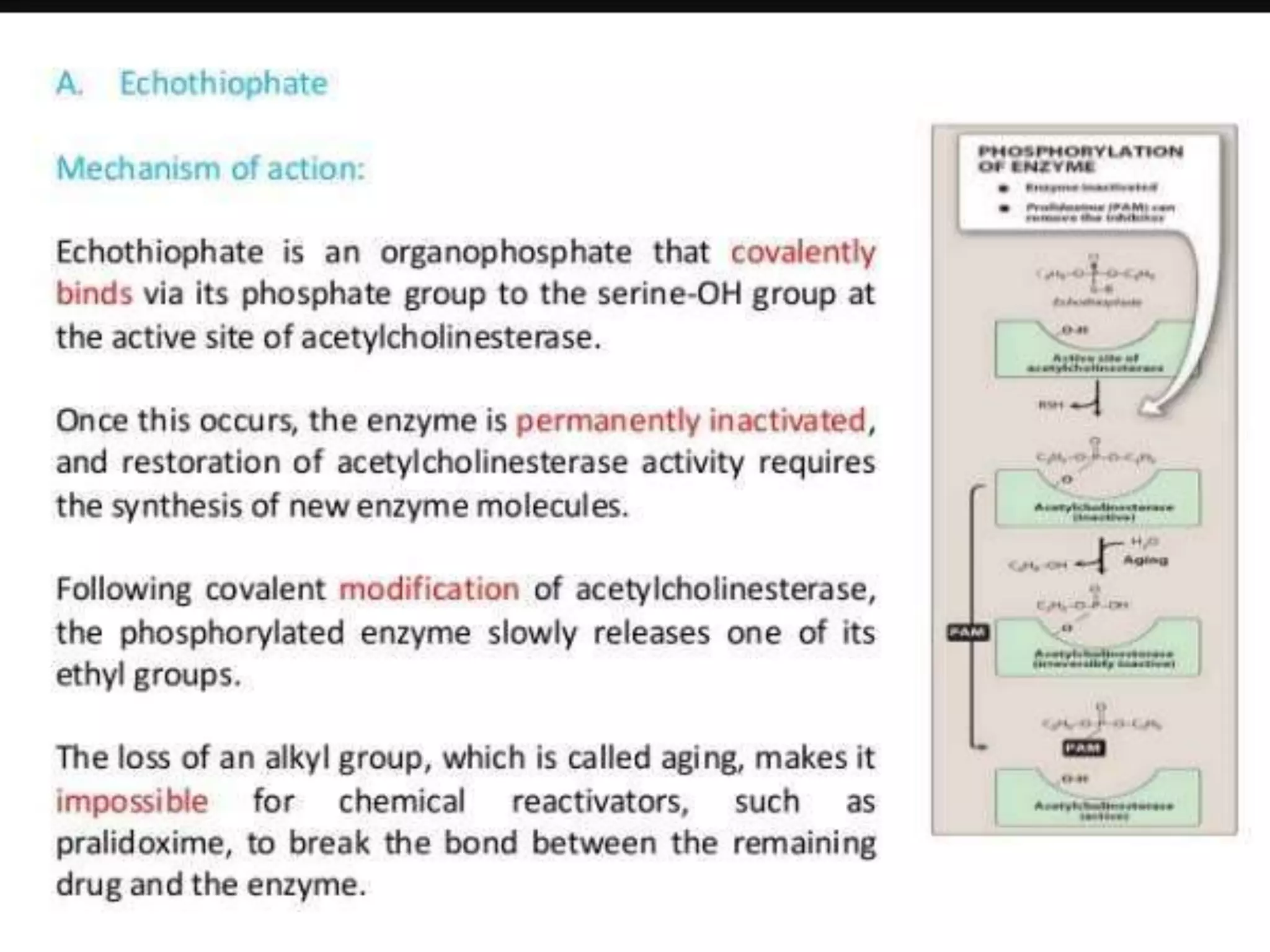
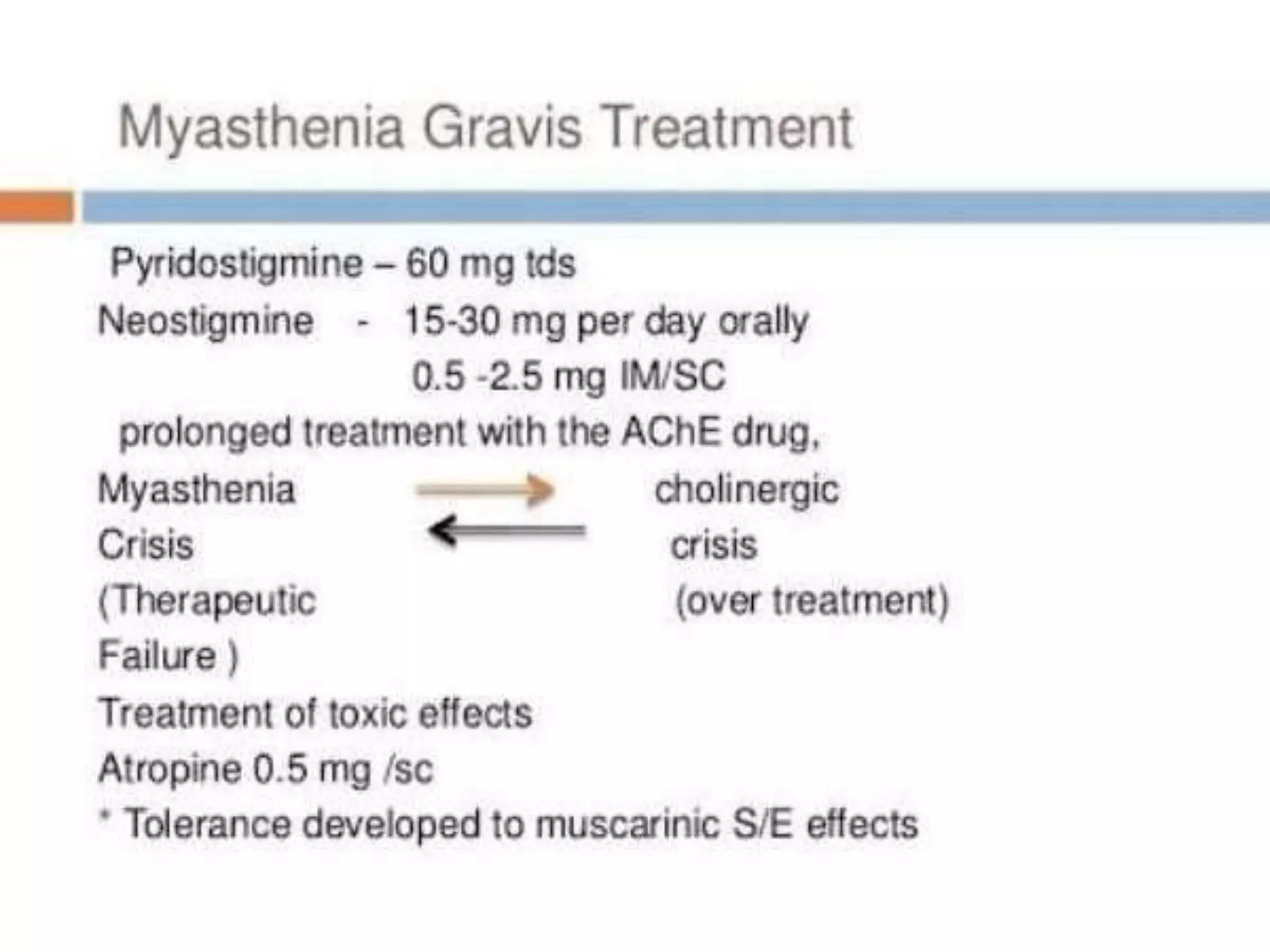
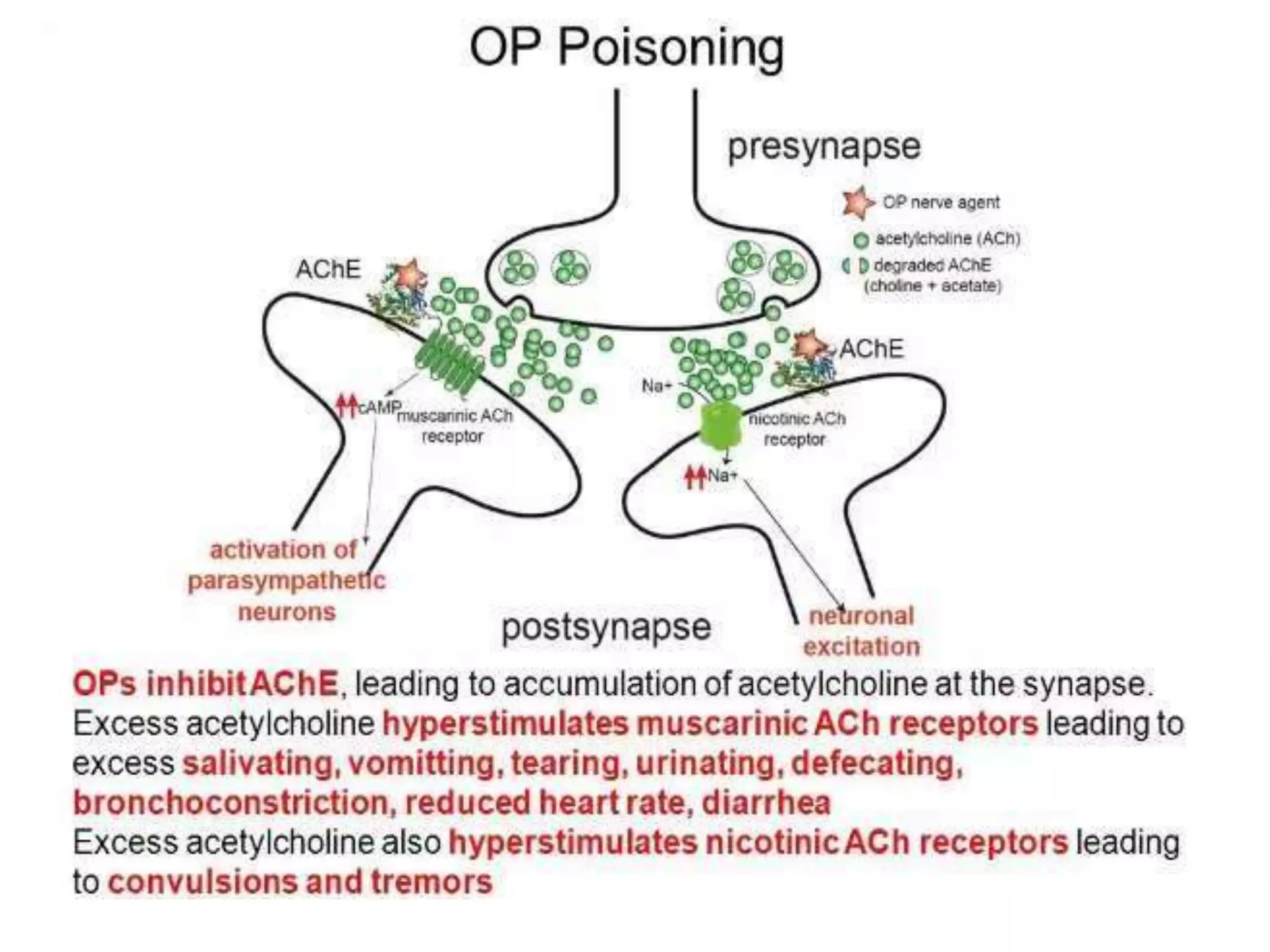
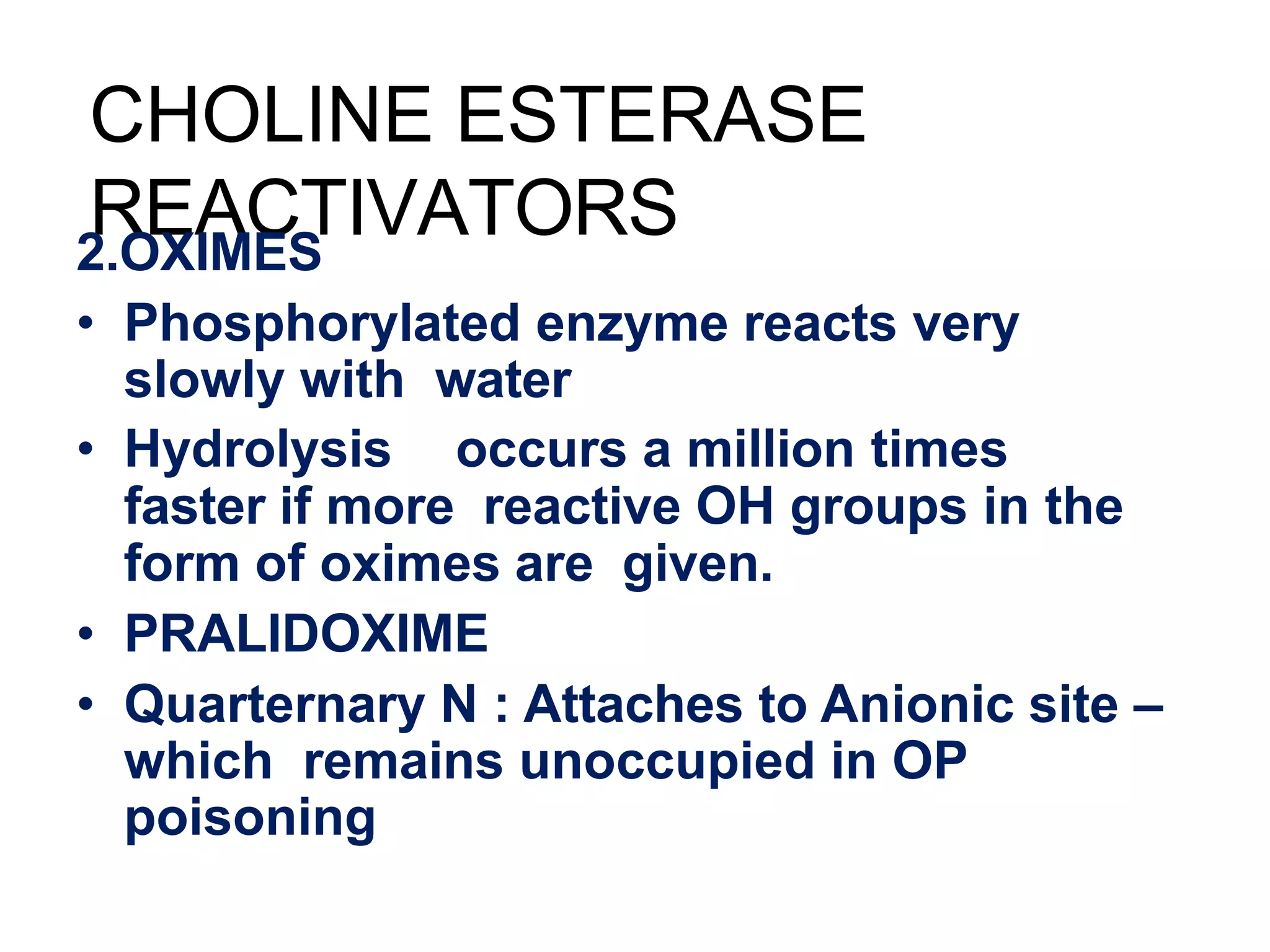
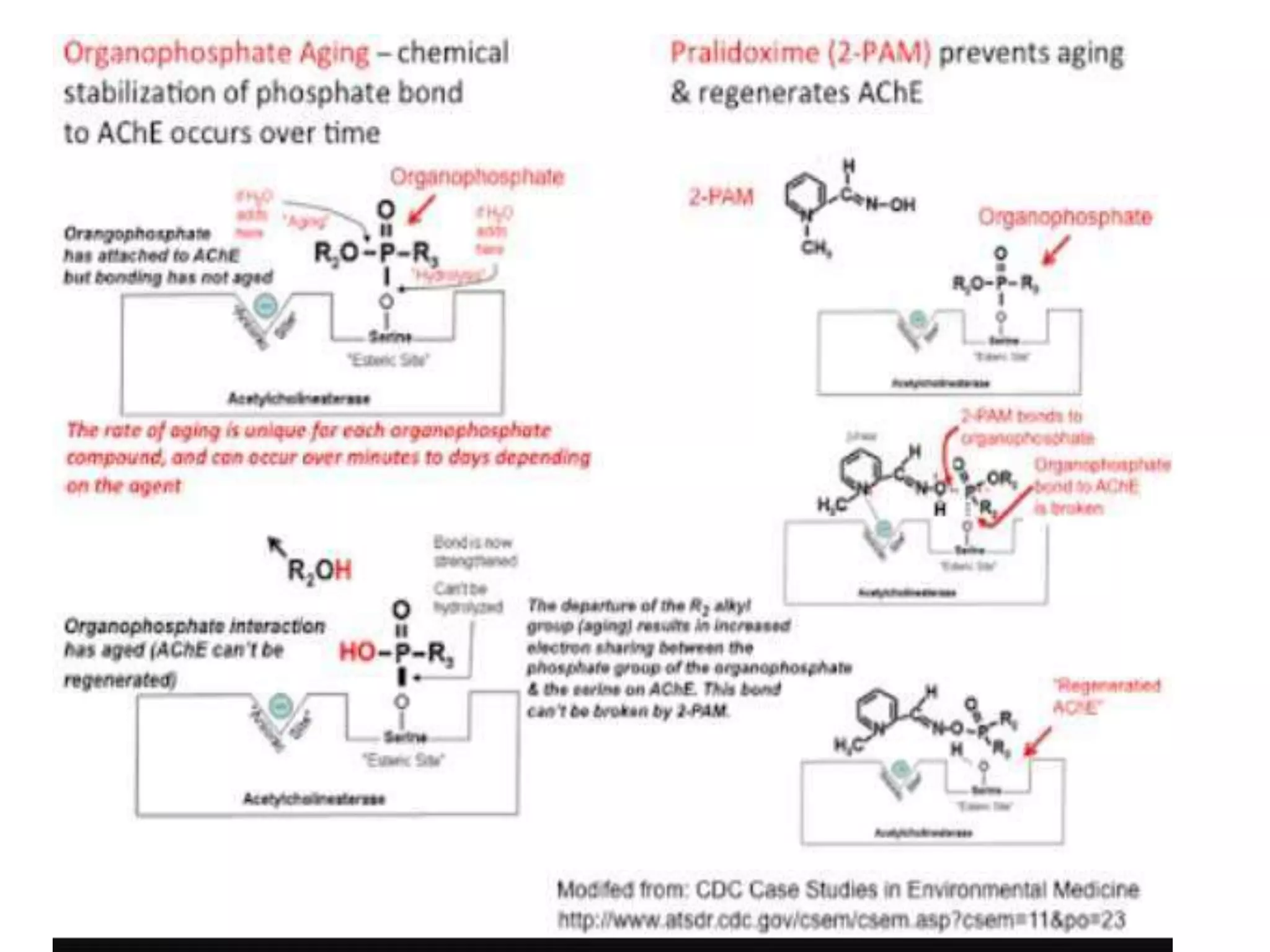
Cholinergic drugs, including acetylcholine, act at autonomic, somatic, and central sites by interacting with two types of receptors: muscarinic and nicotinic. Acetylcholine synthesis involves choline uptake and enzymatic modification, with its effects mediated via direct receptor activation or through cholinesterase inhibition. Pharmacological actions include cardiovascular, gastrointestinal, respiratory, and ocular effects, with therapeutic applications ranging from glaucoma treatment to reversing neuromuscular paralysis.