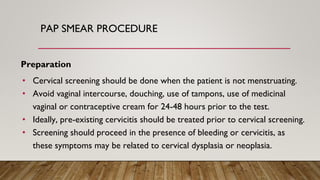
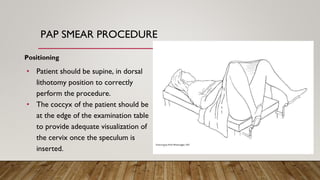
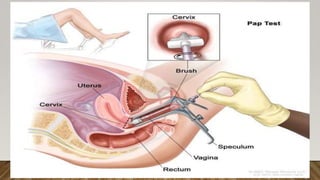
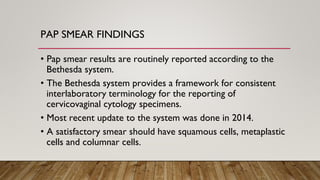
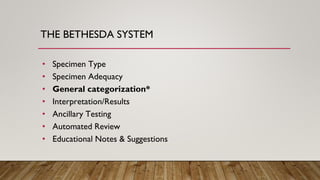
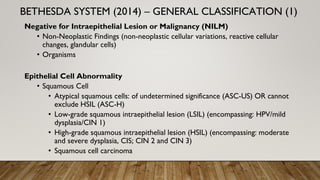
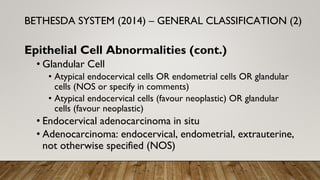
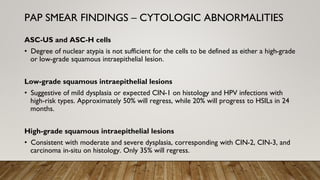
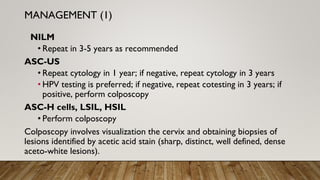
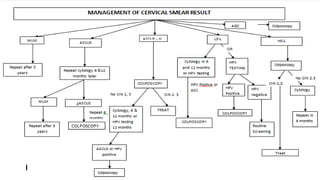
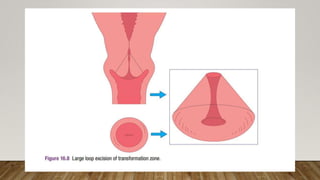
This document outlines the procedure and findings of Pap smear screening and management of abnormal results. A Pap smear involves collecting cervical cells to screen for precancerous lesions. Findings are reported using the Bethesda system and include categories like normal, atypical squamous cells, low-grade lesions, and high-grade lesions. Abnormal results require follow up like colposcopy, treatment of precancerous lesions, or hysterectomy for more severe cases. Regular Pap smear screening can effectively reduce cervical cancer incidence and mortality.


![REFERENCES
1. Cervical Screening: Overview, Human Papillomavirus, Papanicolaou Test. 2021 Aug 22
[cited 2022 Mar 10]; Available from: https://emedicine.medscape.com/article/1618870-
overview
1. Gynaecology by ten teachers, 20E
1. HPV and premalignant disease of the cervix by Prof Anorlu](https://image.slidesharecdn.com/abnormalcervicalsmear-opsunit-240201095942-4e0156b2/85/Abnormal-Cervical-Smear-Presentation-pptx-22-320.jpg)