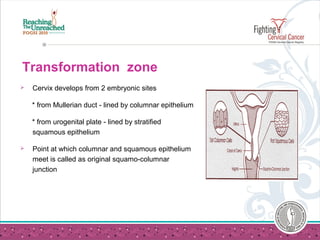
This document discusses Pap smear testing for cervical cancer screening. It begins by outlining the history of Pap smears and their endorsement as an effective screening method. It then discusses cervical cancer as the most common cancer in Indian women. The document covers the histological types of cervical cancer, the transformation zone of the cervix, and why screening is an important strategy. It provides details on taking a Pap smear, including sampling techniques and fixation. The document also discusses reporting systems, screening guidelines, limitations of Pap smears, and liquid-based cytology as an improved method. Throughout, it emphasizes that early detection of pre-cancerous lesions through regular Pap smear screening can prevent the majority of cervical cancers.

![How to take a Pap Smear ?
Spatula is rotated through 360 degrees
maintaining contact with ectocervix
Do not use too much force [bleeding /pain]
Do not use too less force [inadequate sample]
Sample is smeared evenly on the slide and fixed
immediately
Both sides of spatula are to be smeared](https://image.slidesharecdn.com/takingapapsmear-090731232623-phpapp01-140827080206-phpapp01/85/PAP-test-methods-17-320.jpg)
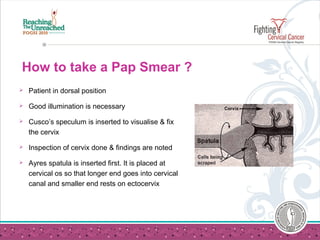
![How to take a Pap Smear ?
Endocervical sample is collected using an
endocervical brush
Insert the cytobrush into canal, so that last bristles
of brush are visible
Rotate the brush through 180 degrees. [more
rotations increase the chance of bleeding]
Sample is rolled on the slide and fixed.](https://image.slidesharecdn.com/takingapapsmear-090731232623-phpapp01-140827080206-phpapp01/85/PAP-test-methods-18-320.jpg)