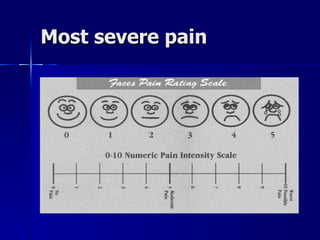
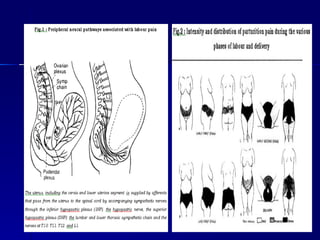
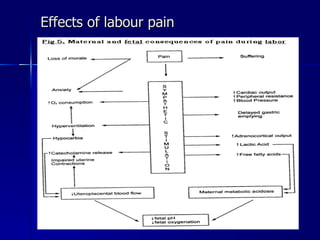
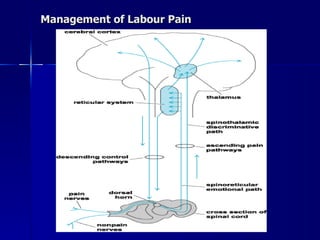
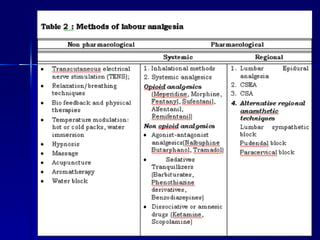
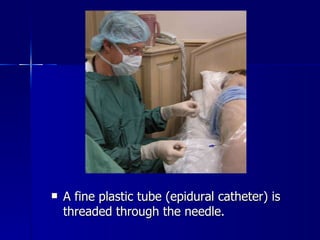
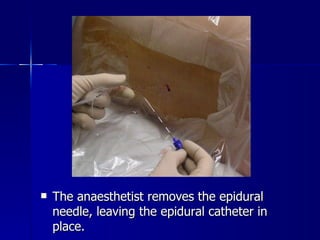
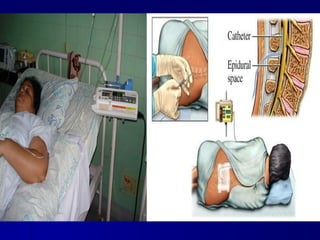
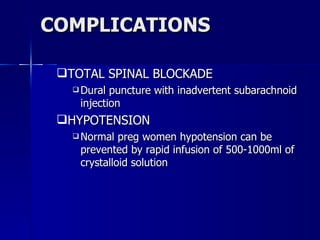
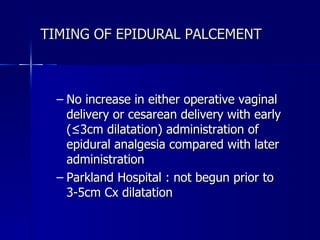
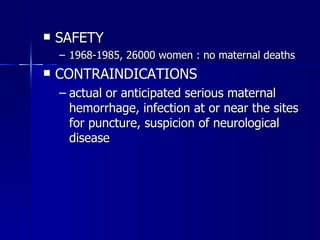
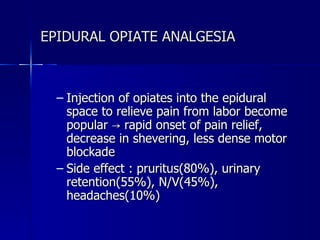
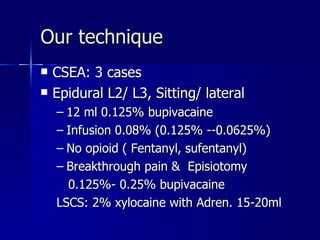
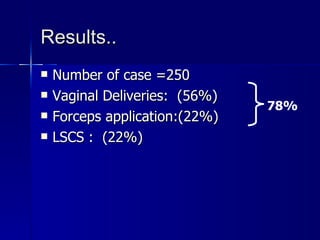
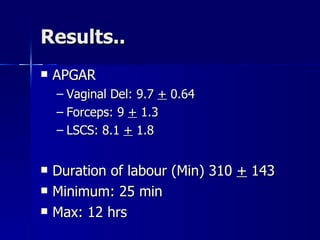
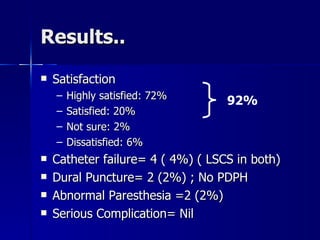
This document discusses epidural analgesia for pain relief during labor and childbirth. It provides details on how epidurals are administered, possible complications, effects on labor and delivery outcomes, and the author's experience with over 250 cases at their hospital. Their results showed high mother satisfaction rates, few complications, and no serious issues. The author concludes that their technique for epidural administration was successful and safe based on their initial experience.