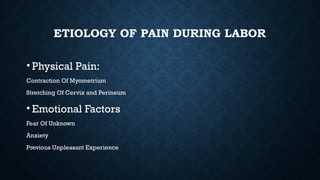
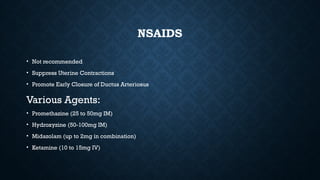
The document provides an overview of various methods for managing labor pain, including pharmacological and non-pharmacological techniques. It discusses systemic opioids and regional anesthesia options, such as epidural and spinal analgesia, highlighting their advantages, disadvantages, and potential complications. The text emphasizes the importance of informed consent, careful monitoring, and the selection of appropriate techniques based on individual patient needs.