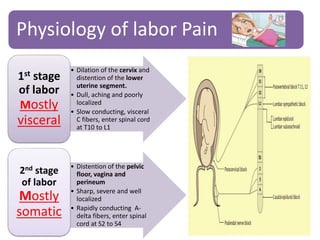
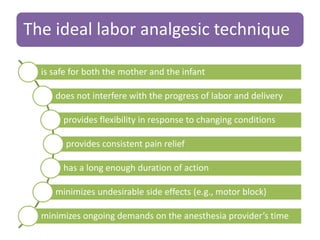
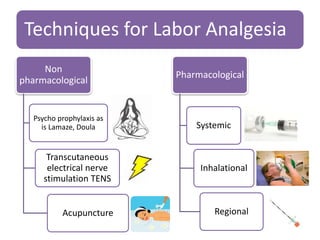
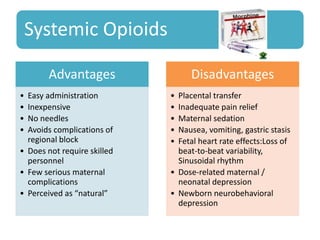
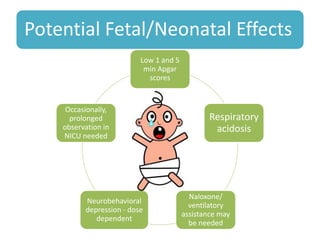
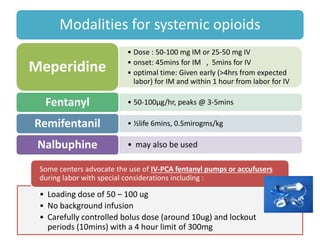
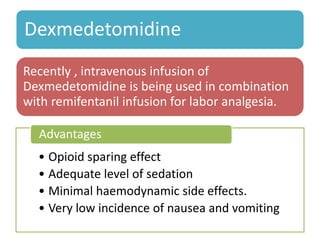
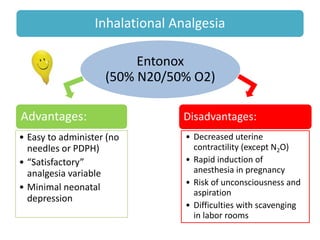
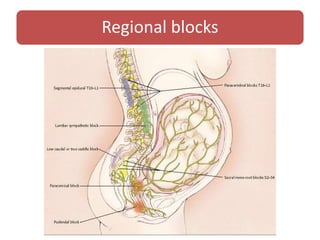
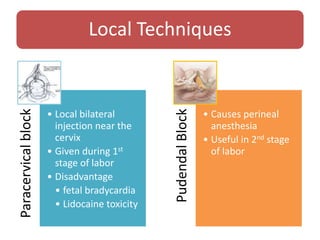
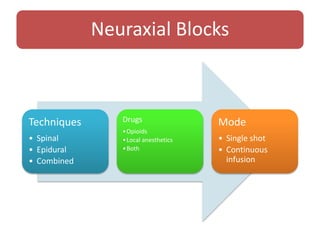
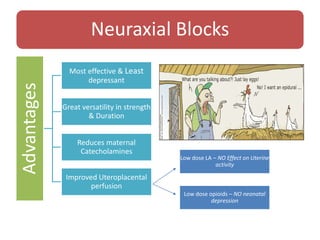
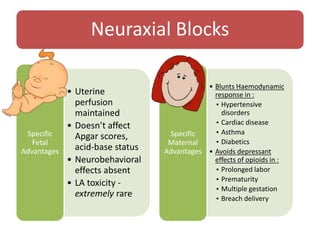
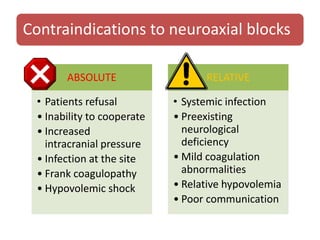
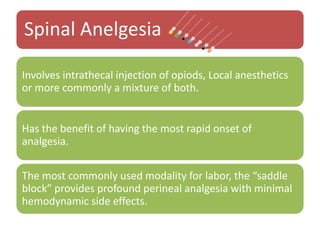
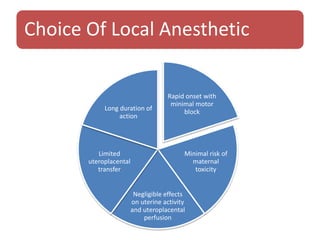
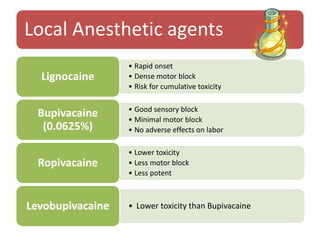
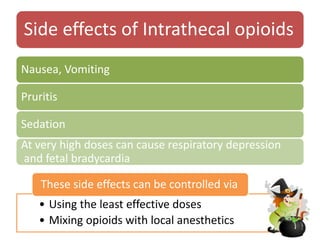
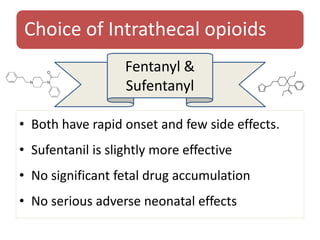
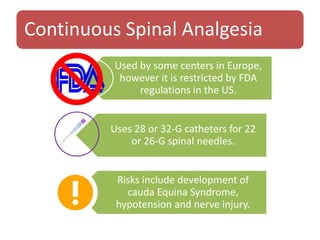
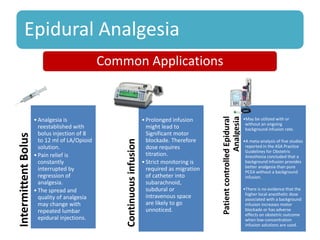
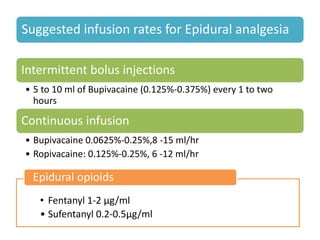
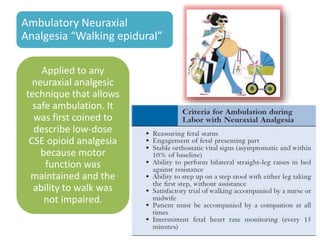
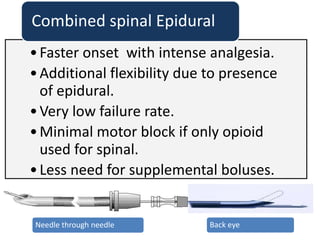
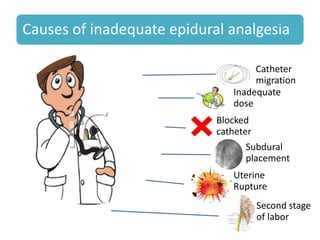
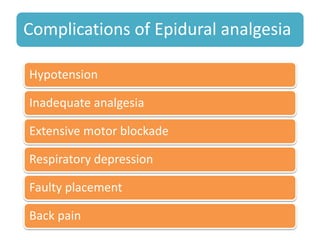
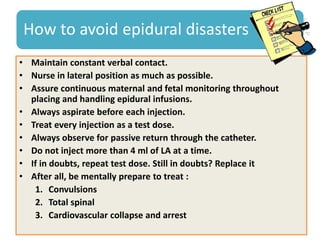
This document discusses pain management techniques for labor and delivery. It begins by noting recommendations from professional organizations that pain relief should be provided during labor when possible. It then describes the physiology of labor pain and the ideal characteristics of labor analgesic techniques. Both non-pharmacological and pharmacological techniques are outlined, including systemic opioids, inhalational analgesia, and various regional nerve blocks like epidural analgesia. Specific drugs, doses, and considerations for safe administration are provided. Complications are also discussed.