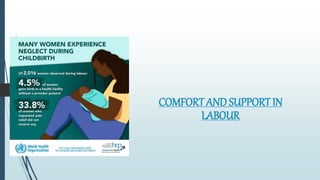
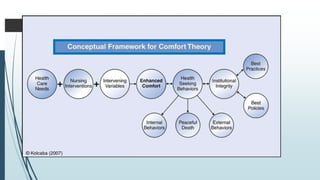
1) The document discusses comfort and support during labor, including definitions of labor and methods to promote comfort such as emotional, physical, and informational support.
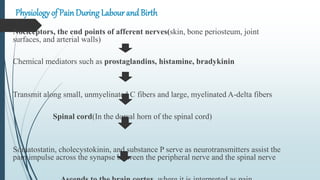
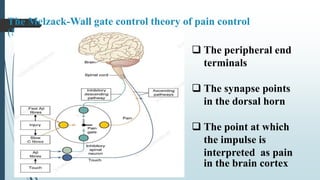
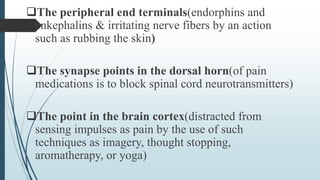
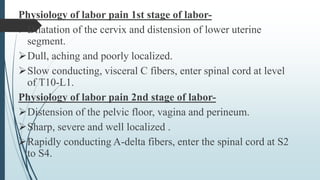
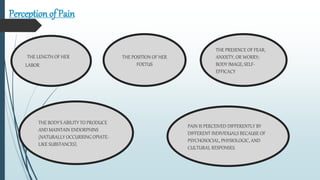
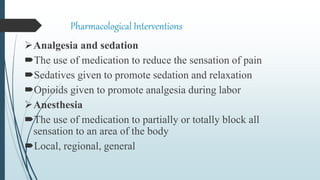
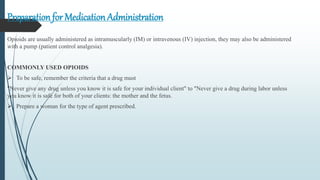
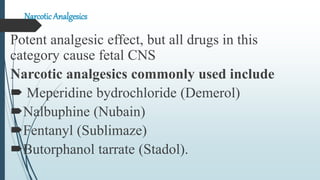
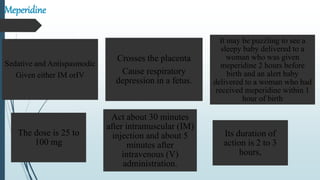
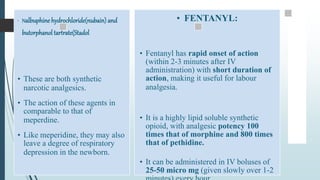
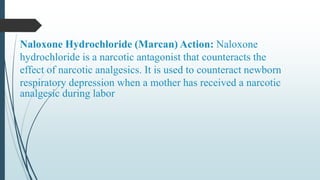
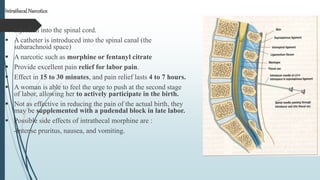
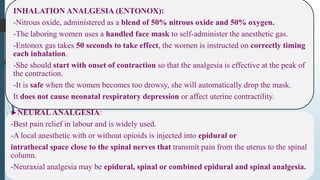
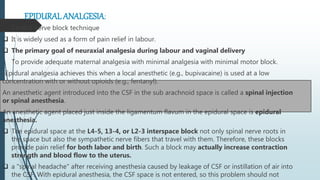
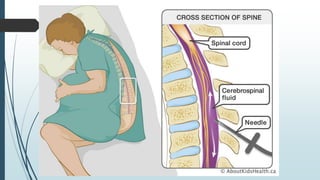
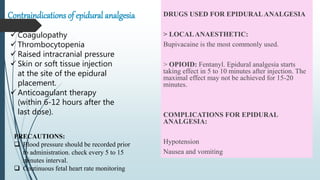
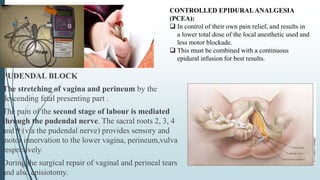
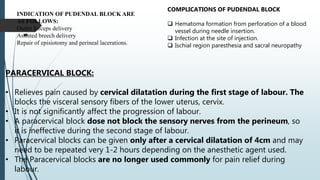
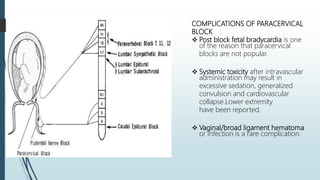
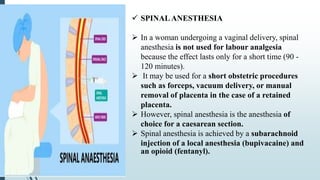
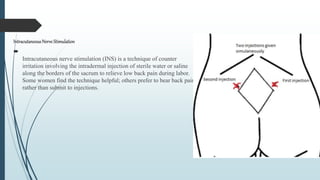
2) It describes the experience of pain during childbirth, including the physiological and cultural factors that influence pain perception. Various pharmacological methods are discussed for pain relief, including narcotic analgesics, inhalation analgesia, neural analgesia techniques like epidural analgesia.
3) Procedures for epidural analgesia administration are provided, noting the importance of aseptic technique and monitoring for side effects like hypotension. Drugs commonly used in epidural analgesia like bupivacaine and fentanyl are also mentioned.