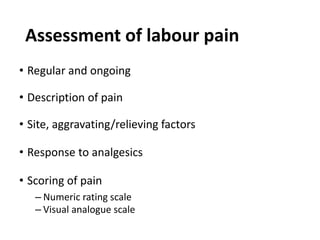
The document provides an overview of labour pain management, highlighting factors influencing pain perception and the importance of controlling acute pain to prevent chronic pain. It discusses various pain management techniques including pharmacological methods such as opioids and regional analgesia, as well as nonpharmacologic approaches. The text emphasizes the significance of pain assessment and suggests interventions tailored to individual needs and circumstances during labour.









![Dosages
Drug Usual dose Onset IV/IM Duration Caution
Morphine 2-5 mg IV/
5-10 mg IM/SC
5 min 3-4 hours Infrequent used during labor due to
greater respiratory depression
in neonate than pethidine
Fentanyl 50-100 mcg IV/
100mcg IM
2-3 min IV10 min
IM 60m
Short acting, potent respiratory depressant, used
as continuous infusion
Max 600 mcg [6 hrs] and/or PCA;
Cumulative effect
with large doses over
time.
Pethidine 50-100mg IM every 3-4
hours
25 -50mg IVevery 60-90
minutes+ Promethazine
25mg IM every 3-4hours
Within 10 minutes
for IM
IM Onset 30-45
minutes
IV onset 5minutes
Maternal sedation
Newborn respiratory depression (max 3-5hours
after dose least if given within 1 hour)
Associated low apgar scores
Tramadol 100mg IM/IV in active
phase of labour
Within 15min 4Hours Minimal maternal side effects(nausea,vomiting,
drowsiness).](https://image.slidesharecdn.com/15-230616135044-8b291605/85/15-Labour-pain-Edt-7th-ppt-11-320.jpg)