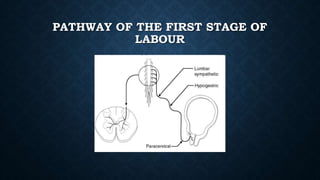
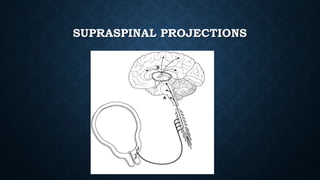
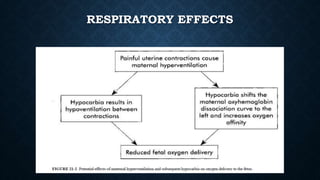
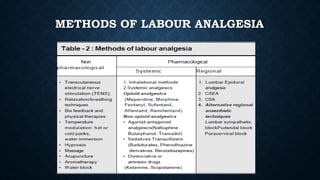
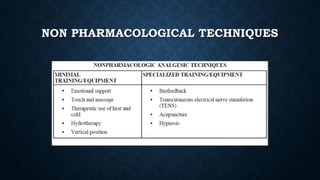
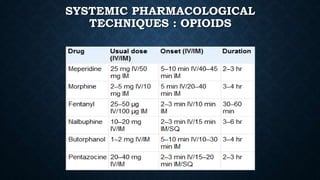
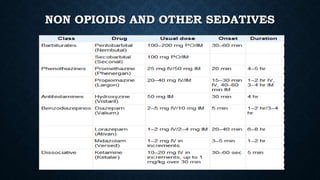
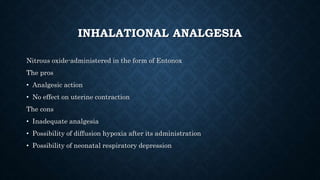
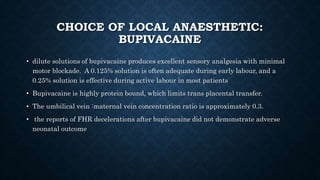
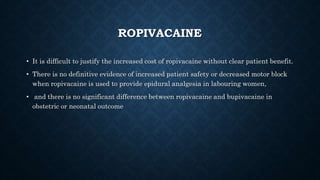
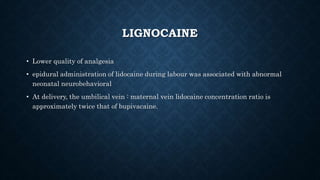
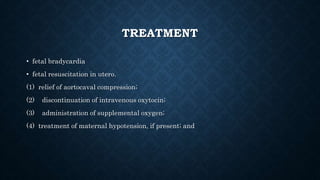
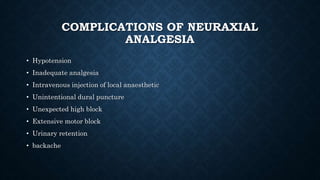
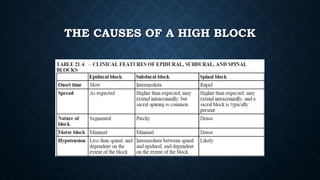
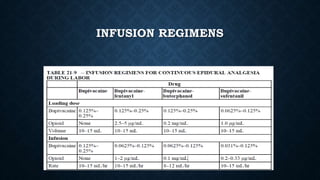
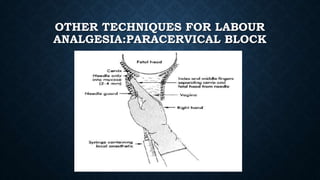
The document discusses various methods of labour analgesia including non-pharmacological techniques, systemic drugs, inhalational agents, epidural analgesia and spinal analgesia. It describes the stages of labour and mechanisms of labour pain. For epidural analgesia, it recommends bupivacaine with lipid-soluble opioids like fentanyl or sufentanil. It outlines administration techniques and discusses complications and fetal effects for different analgesic methods.