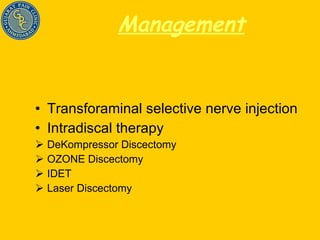
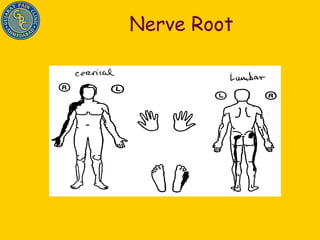
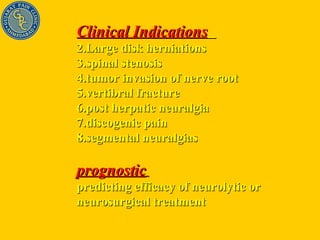
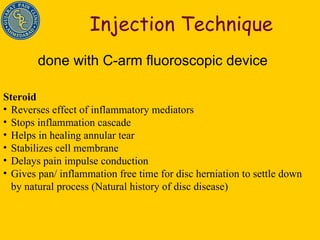
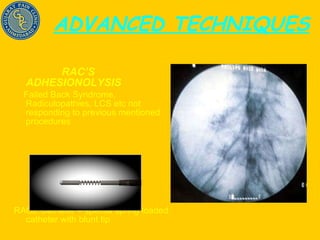
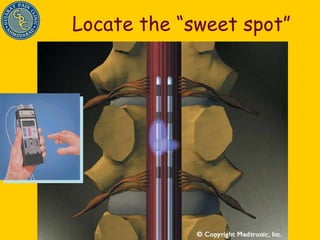
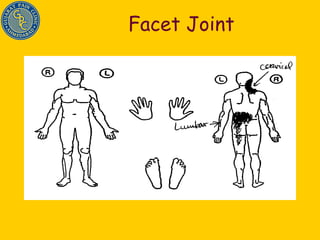
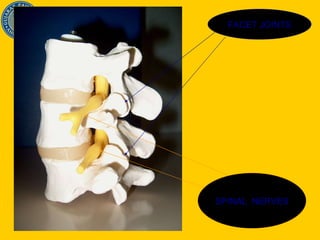
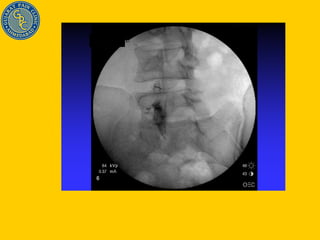
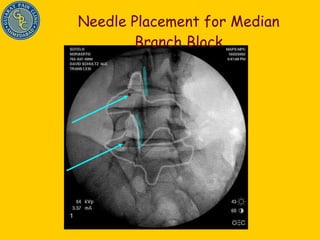
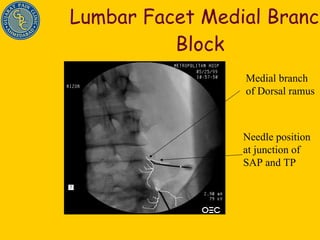
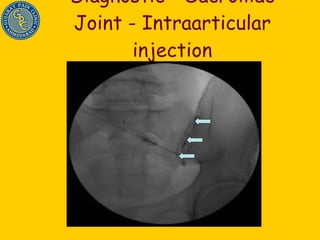
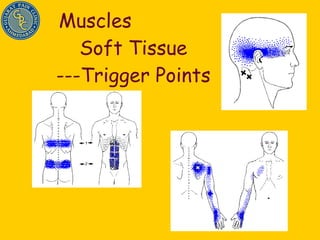
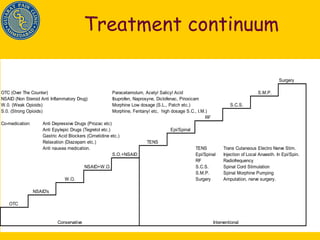
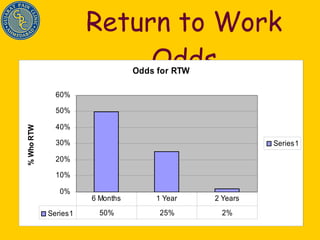
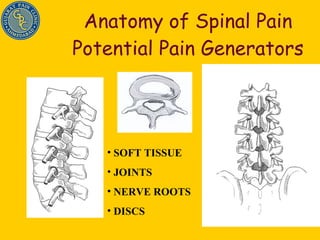
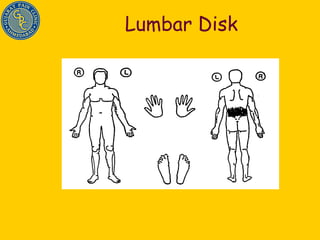
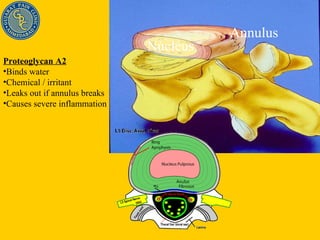
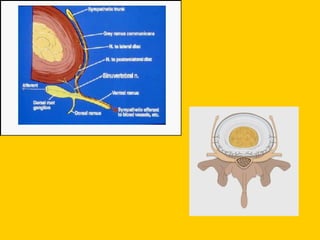
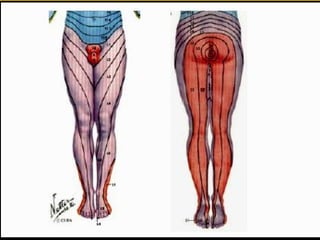
Dr. Shiraz Munshi discusses his approach to treating chronic back pain, which involves precision diagnosis through a combination of history, physical exam, imaging, and diagnostic injections to identify the specific source of pain in 70% of cases. This allows for targeted, minimally invasive treatments like nerve blocks, radiofrequency ablation, and spinal cord stimulation to effectively manage pain and improve outcomes like returning to work. The document outlines various potential sources of spinal pain and techniques for diagnosing and treating conditions of the discs, facet joints, sacroiliac joints, and nerves.




![CONTRAST DISTRIBUTION [80] : (AS EVALUATED BY FLUOROSCOPY ) Disk has a complete radio fissure that allows injected fluid to escape. Can be in any stage of degeneration. “ Ruptured” (R) Degenerated disk with radio fissure leading to the outer edge of the annulus. “ Fissured” (F) Degenerated disk with fissures and clefts in the nucleus and inner annulus. “ Irregular” (I) Mature disk with nucleus starting to degenerate into fibrous lumps. “ Lobular” (L) No signs of degeneration, Soft white amorphous nucleus “ Cotton Ball” (CB) Stage of Disk Degeneration (C-arm View) Discogram Type “ Ruptured” “ Fissured” “ Irregular” “ Lobular” “ Cotton Ball”](https://image.slidesharecdn.com/backpain-091210140458-phpapp02/85/Back-Pain-22-320.jpg)