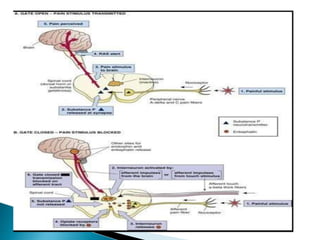
The document discusses the gate-control theory of pain proposed by Melzack and Wall, which explains how pain transmission is modulated in the spinal cord, particularly in the substantia gelatinosa. It describes the roles of different types of nerve fibers (A-β, A-δ, and C fibers) in inhibiting or facilitating pain signals and how various therapeutic modalities can influence these pain pathways. It also highlights the interaction between spinal mechanisms and higher brain centers in pain modulation.