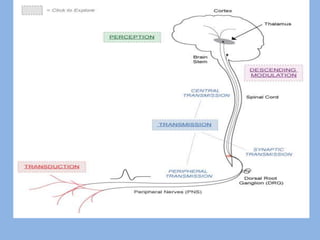
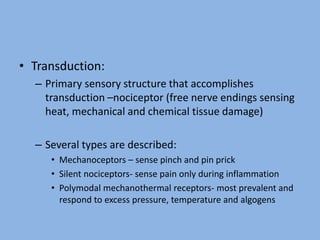
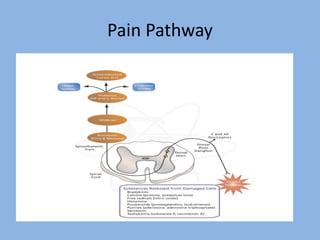
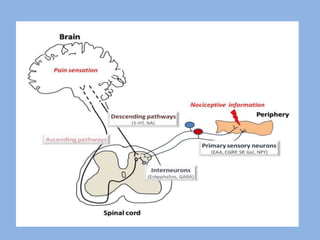
1) Pain physiology involves transduction, transmission, perception, and modulation of nociceptive signals from the periphery to the brain.
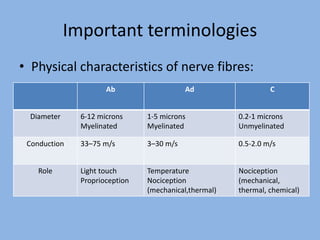
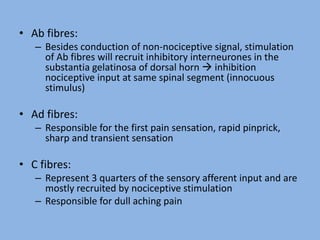
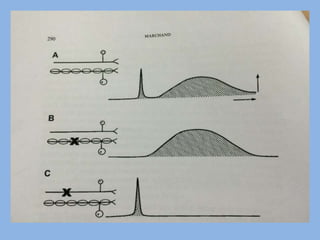
2) Pain signals are transmitted via Aδ and C nerve fibers to the spinal cord and then to the brain. Aδ fibers transmit fast, sharp pain while C fibers transmit slow, dull pain.
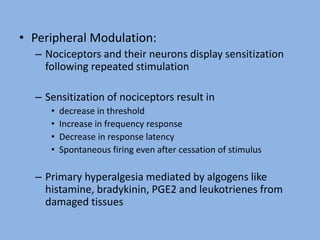
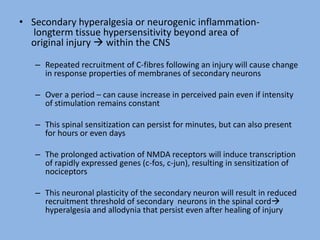
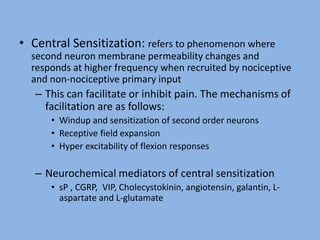
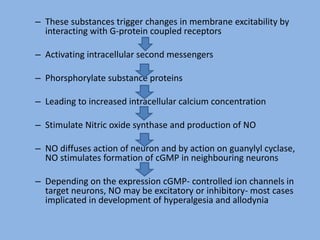
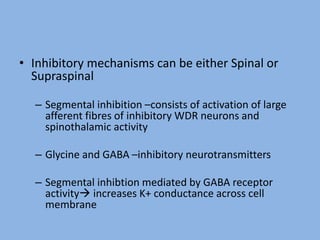
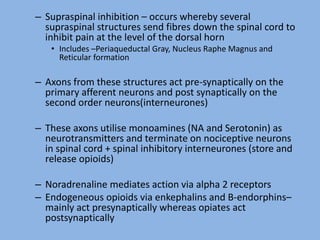
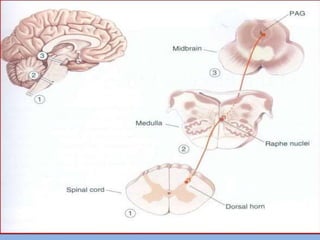
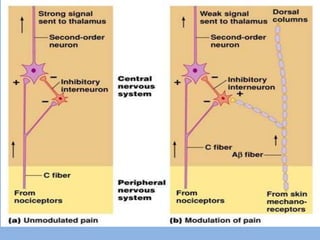
3) Central modulation occurs in the spinal cord and brain and can either facilitate or inhibit pain transmission and perception through mechanisms like windup, sensitization, and the release of neurotransmitters.