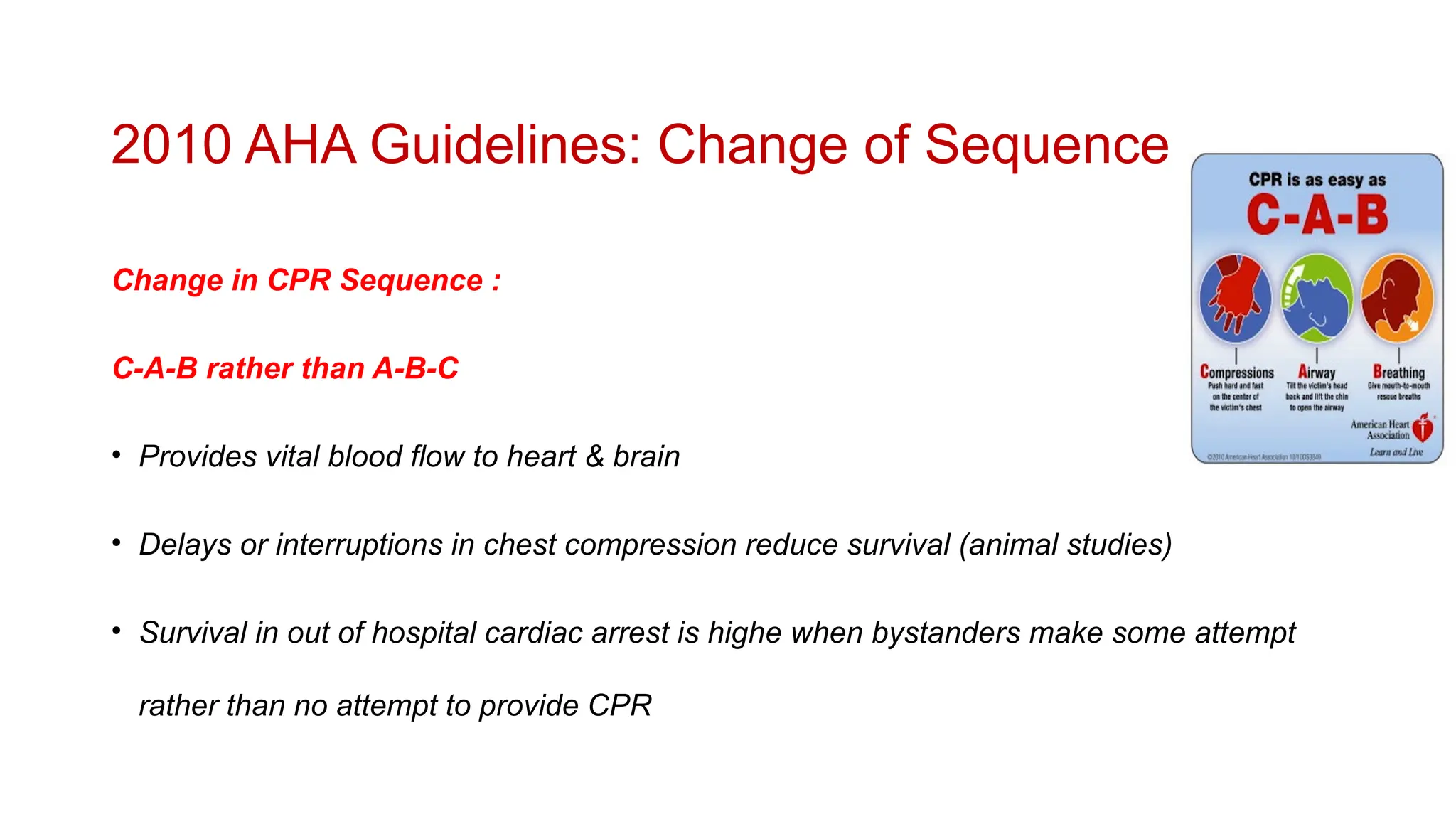
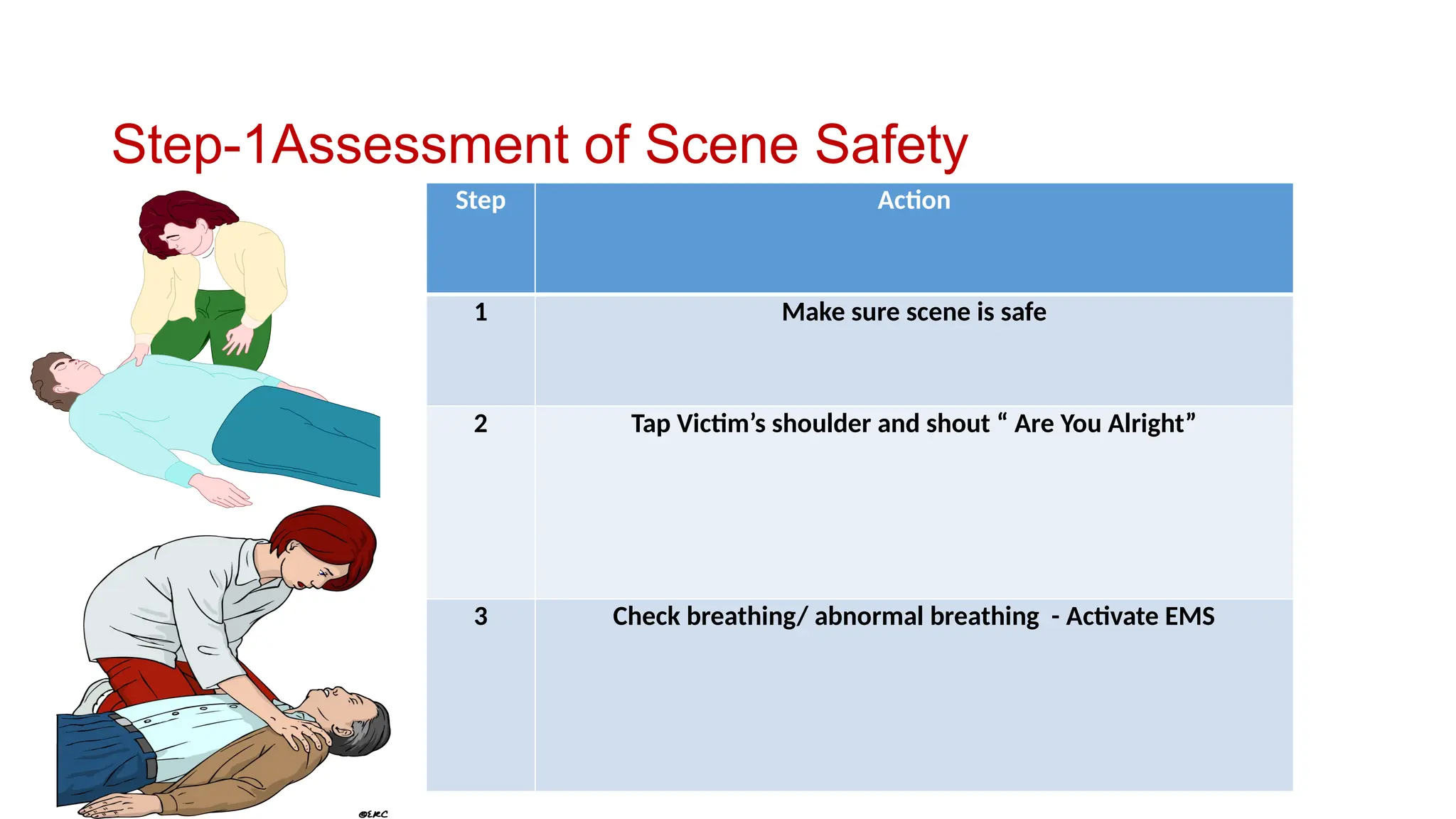
The document covers basic life support (BLS) concepts, emphasizing the critical steps and techniques to perform CPR effectively on adults, children, and infants. It highlights the importance of immediate response, high-quality chest compressions, and the use of AEDs, while detailing protocols for both single and multiple rescuers. Post-cardiac arrest care and strategies to increase survival rates through early intervention are also discussed.