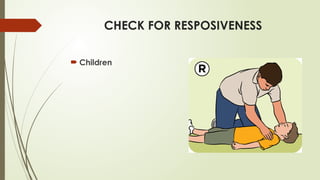
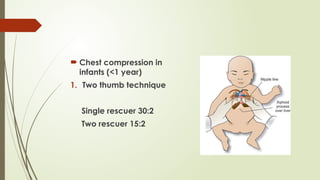
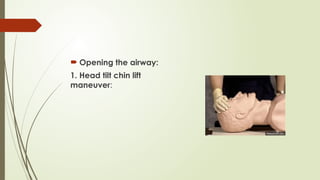
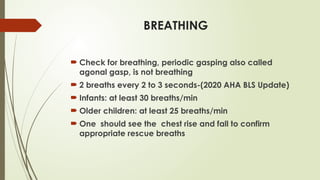
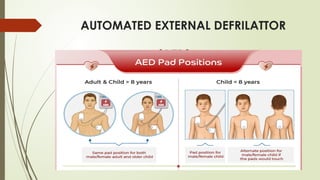
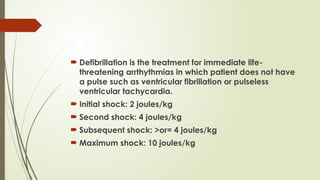
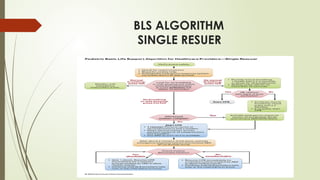
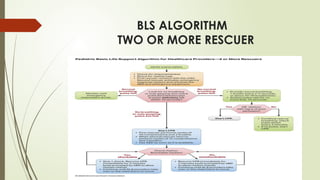
The document outlines the basic life support (BLS) protocols for pediatric patients, emphasizing the importance of cardiopulmonary resuscitation (CPR) and the sequence of assessment, circulation, airway, and breathing. It details techniques for chest compressions and the use of automated external defibrillators (AED) for managing cardiac arrest and life-threatening arrhythmias in children. Post-resuscitation care is highlighted as crucial for optimizing tissue perfusion, particularly to the brain, within a 30-minute timeframe.