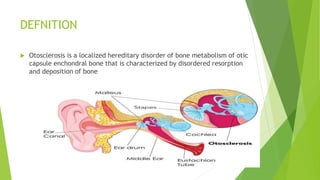
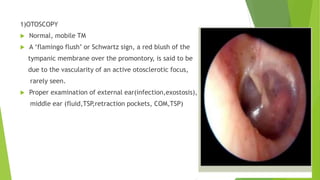
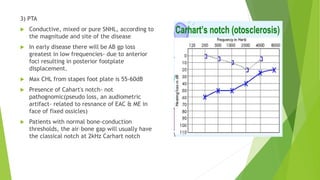
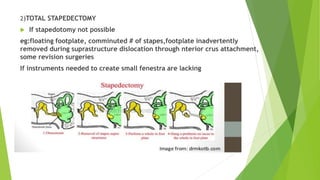
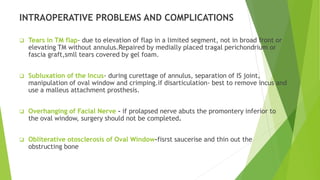
Otosclerosis is a hereditary disorder characterized by abnormal bone remodeling in the otic capsule. It commonly causes conductive hearing loss but can rarely cause sensorineural hearing loss. There are several types but the most common is clinical otosclerosis which affects the stapes and causes conductive hearing loss. It is more prevalent in Caucasians than other populations and more common in females. Treatment options include hearing aids, fluorides/bisphosphonates to slow progression, and surgery like stapedotomy or total stapedectomy to reconstruct the ossicular chain. Potential surgical complications include facial nerve injury, taste disturbance, infection, and sensorineural hearing loss.