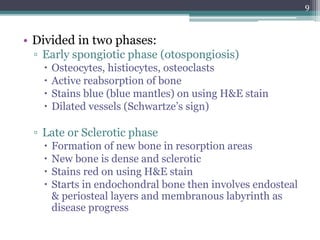
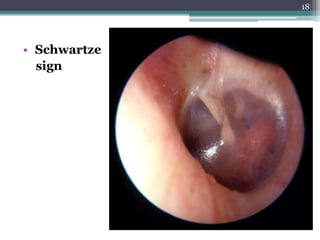
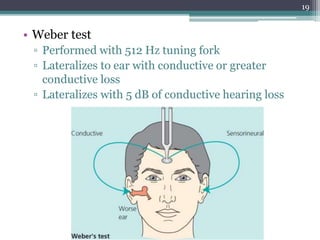
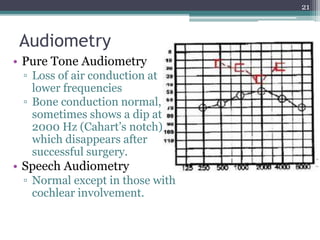
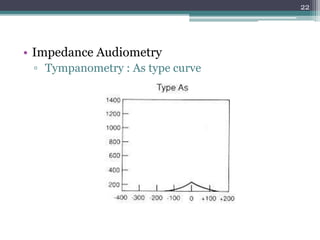
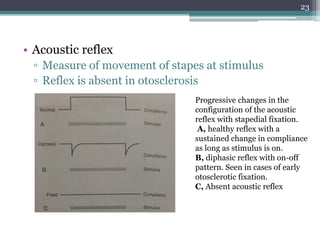
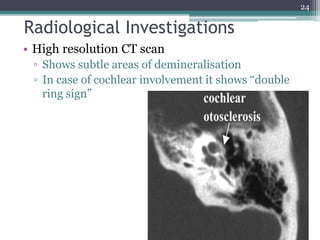
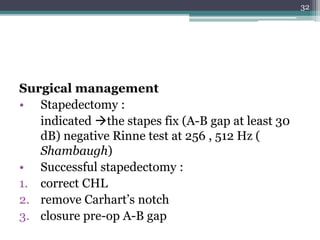
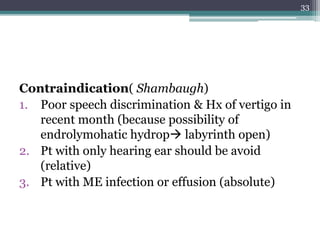
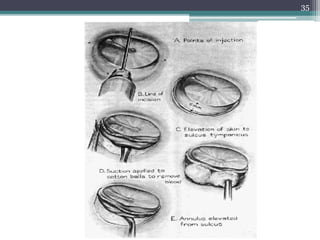
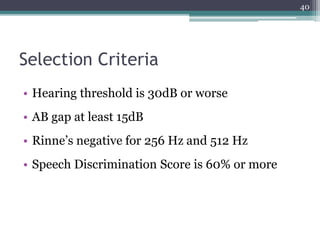
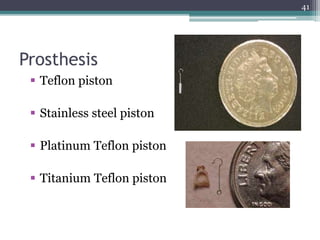
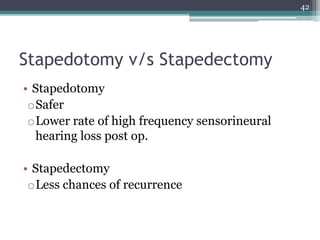
Otosclerosis is a primary disease of the bony otic capsule characterized by abnormal bone resorption and replacement with thicker woven bone. It commonly causes progressive conductive hearing loss. Diagnosis involves history of gradual hearing loss, physical exam finding of Schwartze's sign or positive Rinne test, and audiometry showing conductive loss. Treatment options include hearing aids, medication to slow progression, or stapedotomy/stapedectomy surgery for severe cases. The goal of surgery is to create a new connection between the middle and inner ear by placing a prosthesis between the incus and stapes footplate.