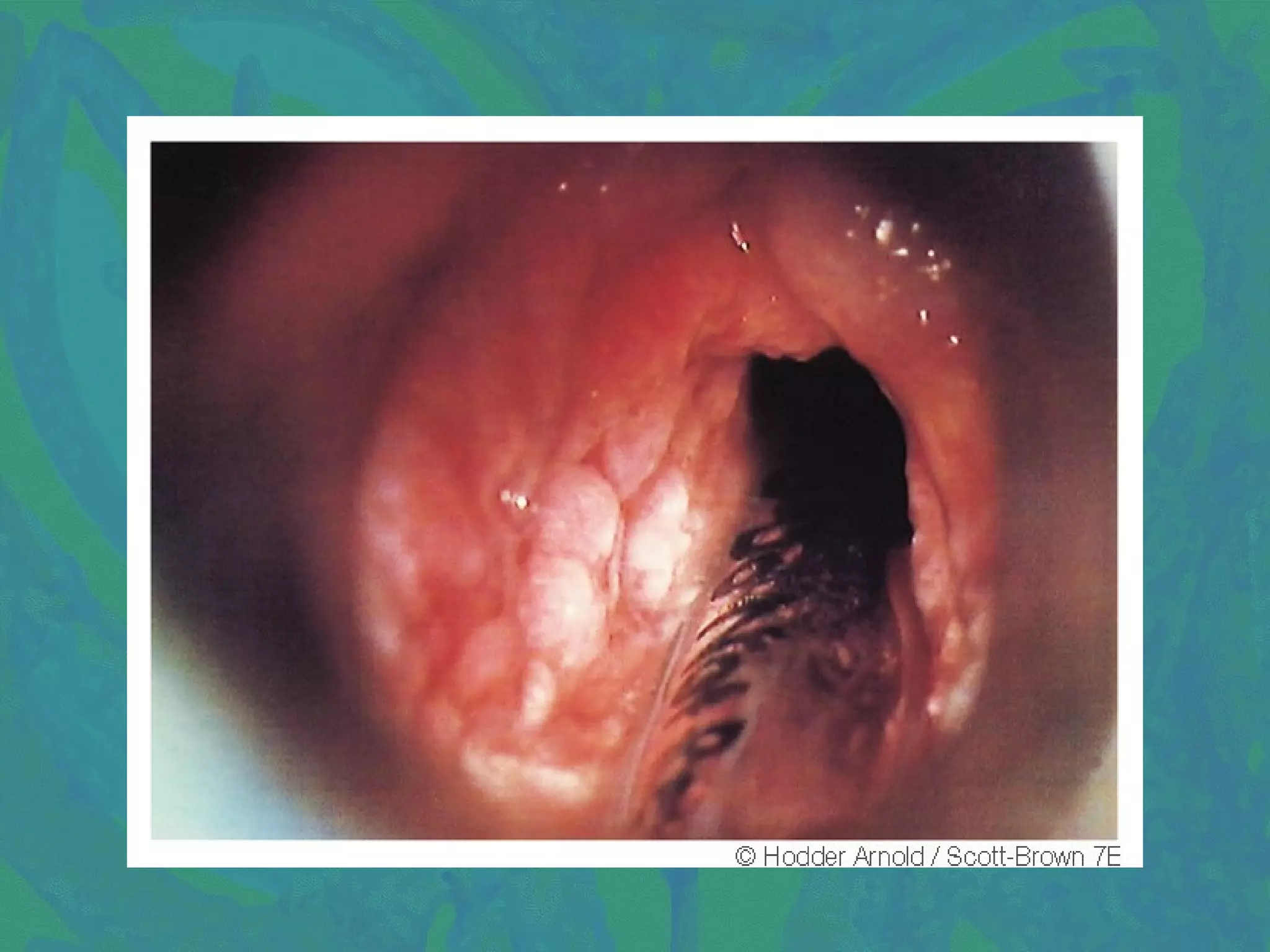
1. Tuberculosis of the larynx commonly affects the posterior larynx, causing submucosal tubercles that can ulcerate, forming undermined ulcers. Symptoms include throat pain, hoarseness, and dysphagia. Diagnosis involves chest X-ray, sputum examination, laryngoscopy, and biopsy. Treatment consists of anti-tubercular drugs, vocal rest, and nutrition supplements.
2. Scleroma of the larynx is caused by Klebsiella rhinoscleromatis and commonly involves the subglottic region, presenting as a smooth red swelling. Diagnosis involves biopsy and culture. Treatment includes antibiotics, steroids, and surgery for stenosis