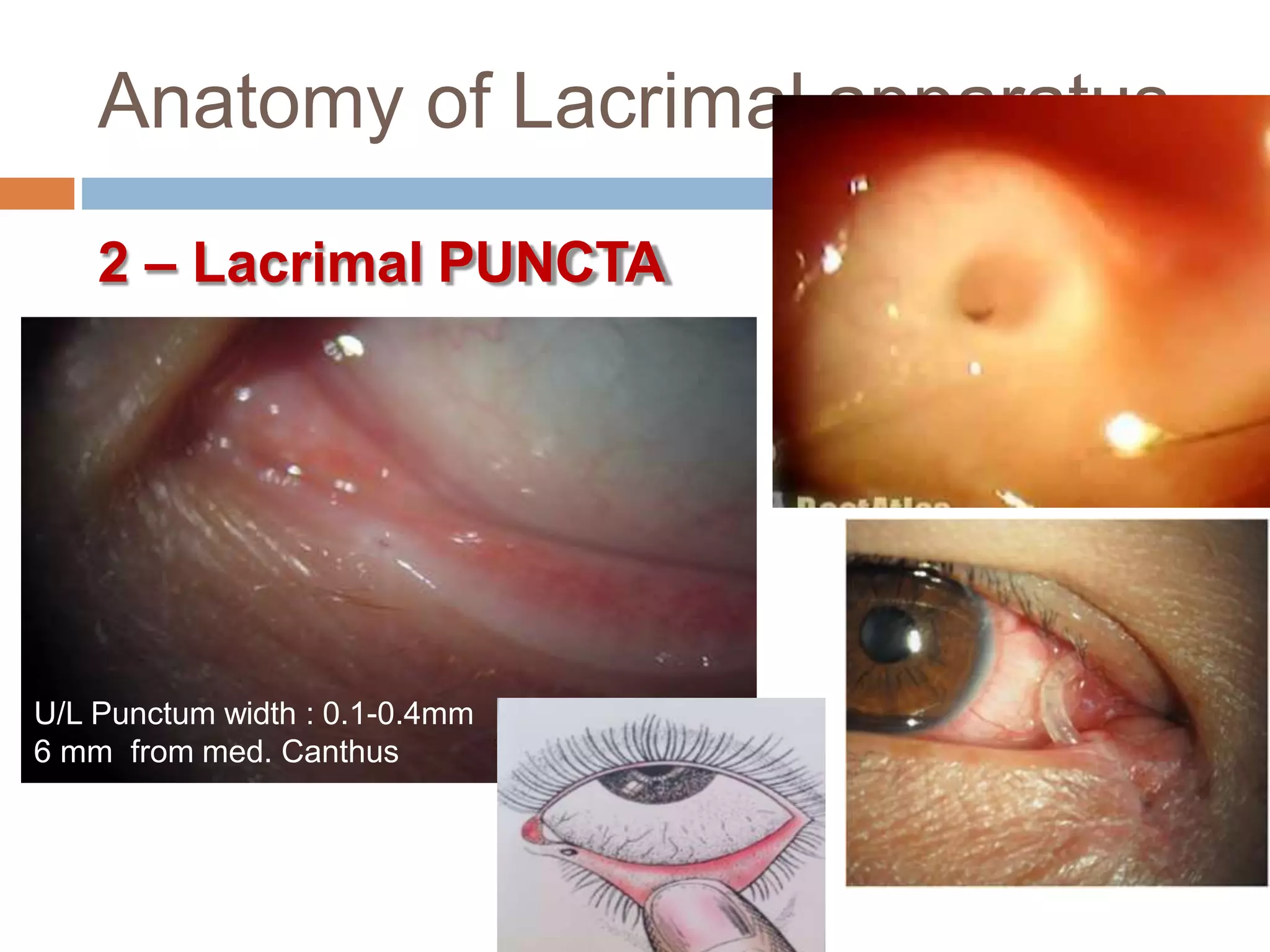
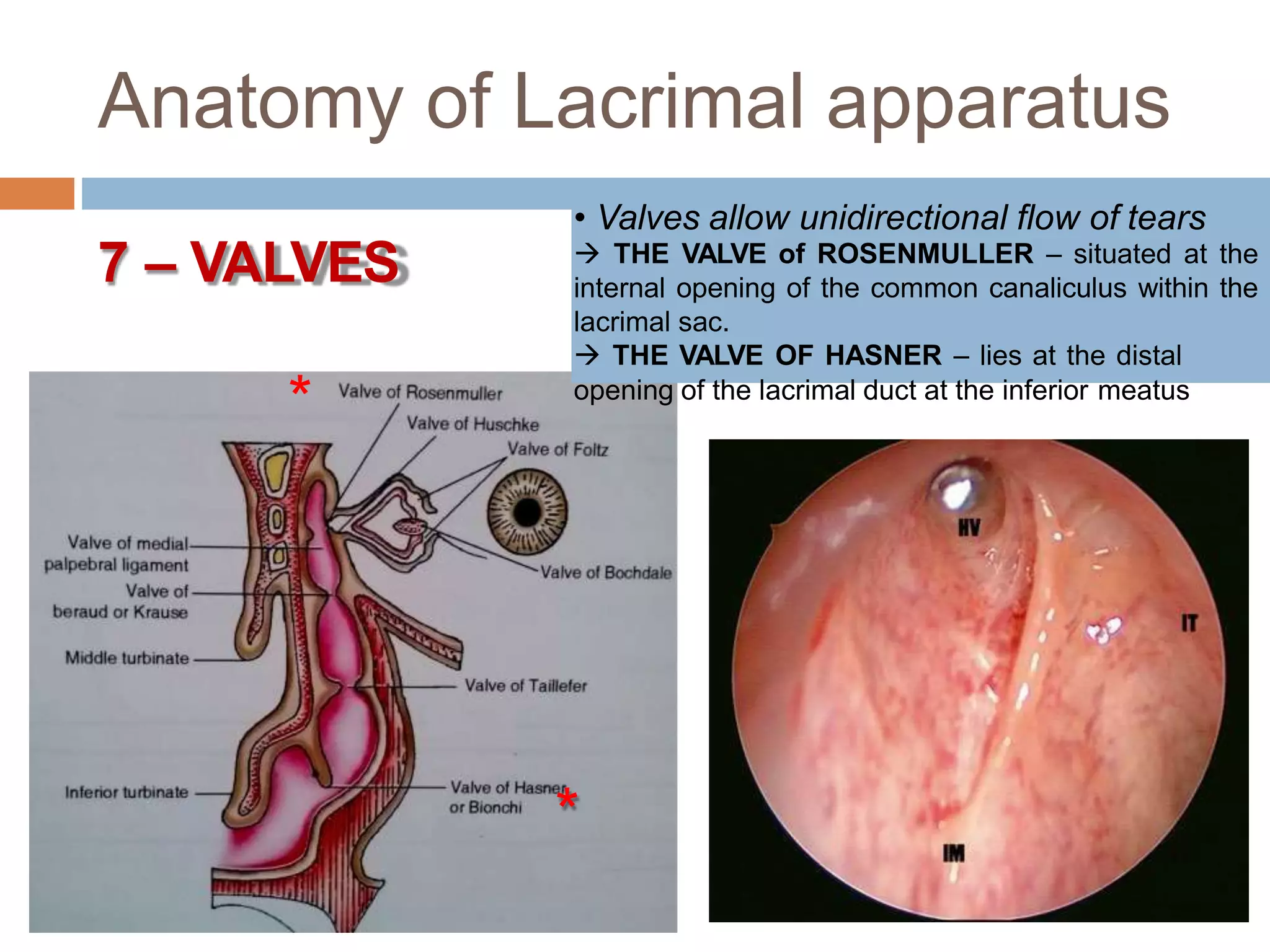
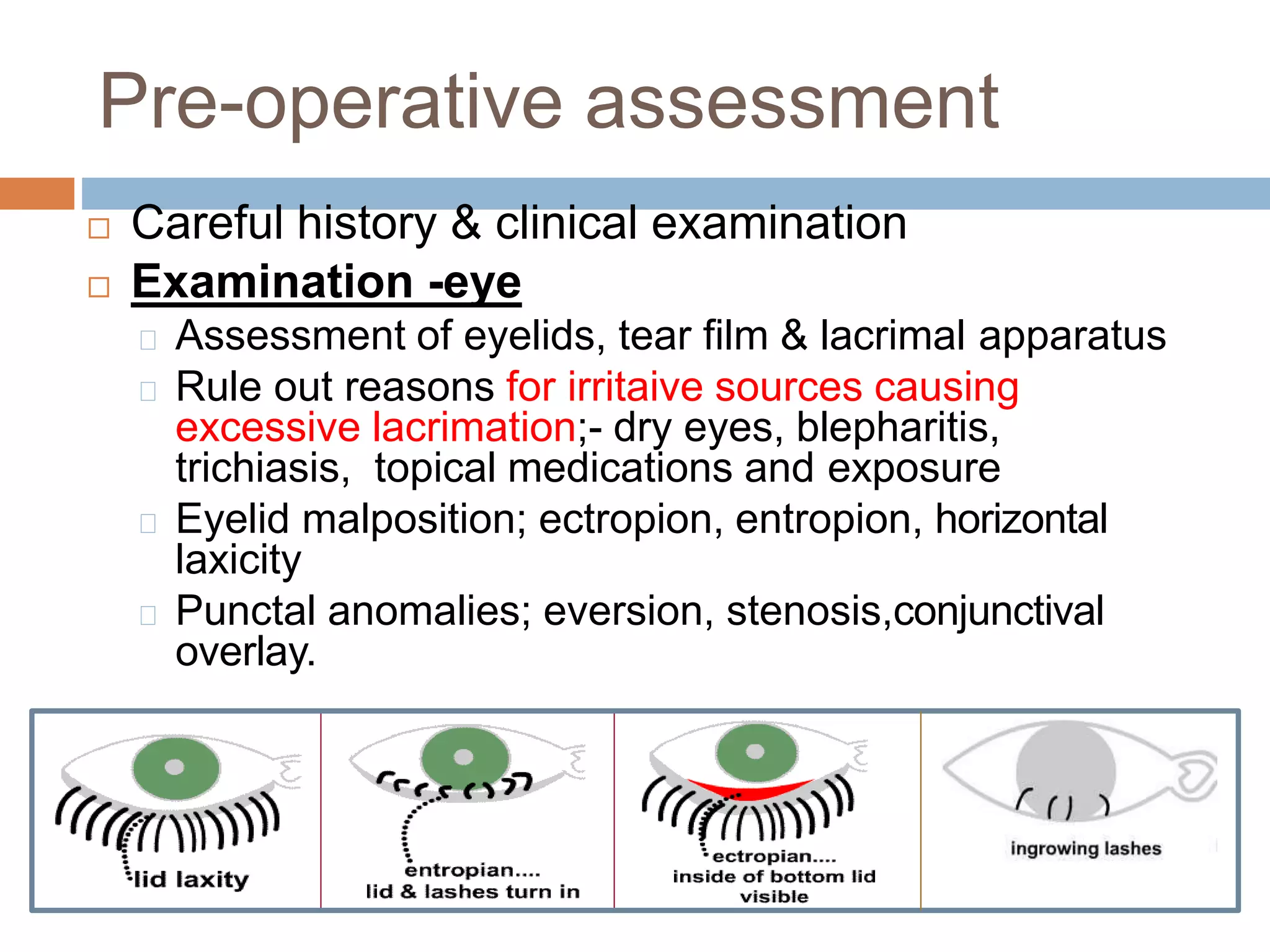
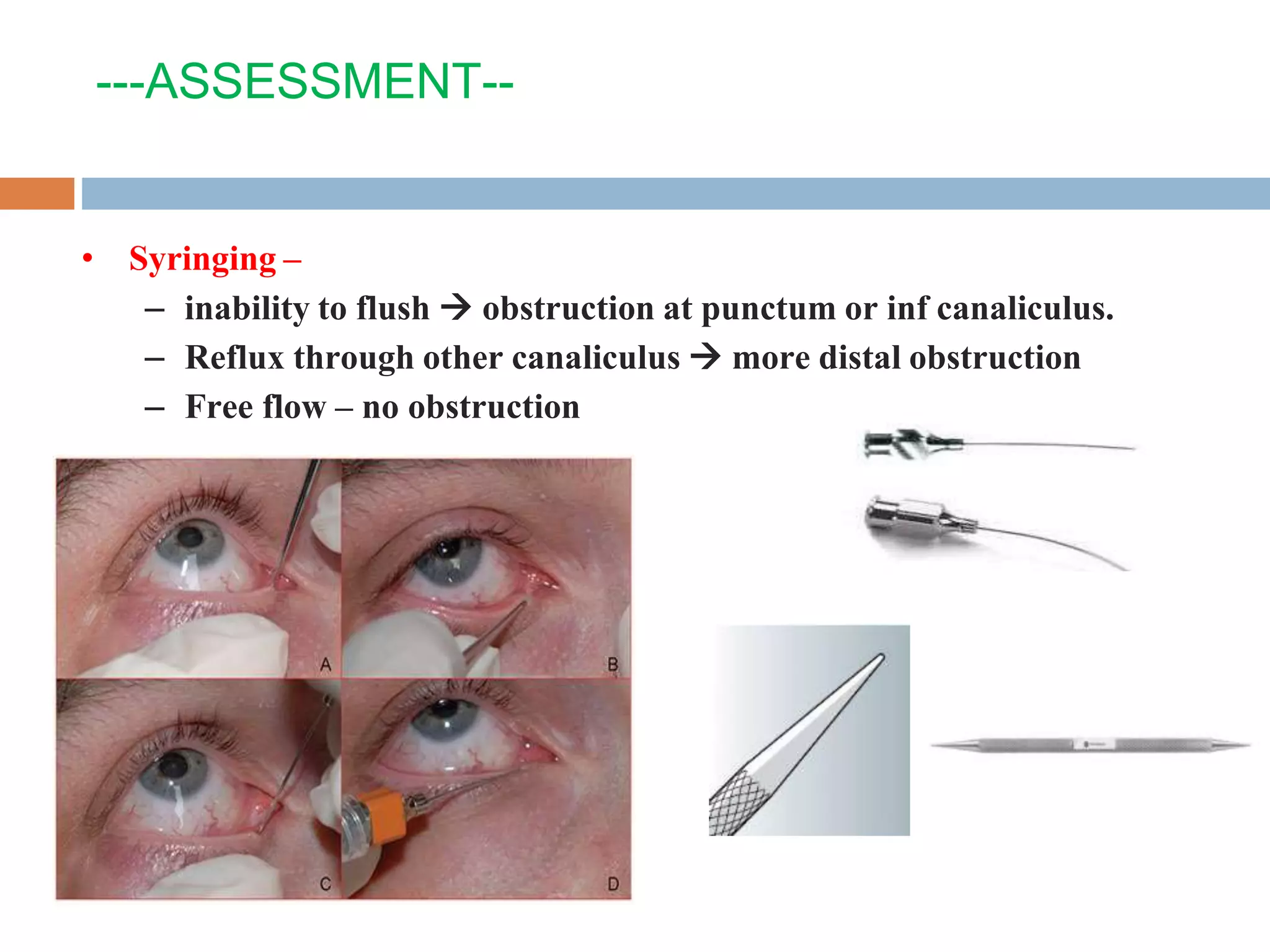
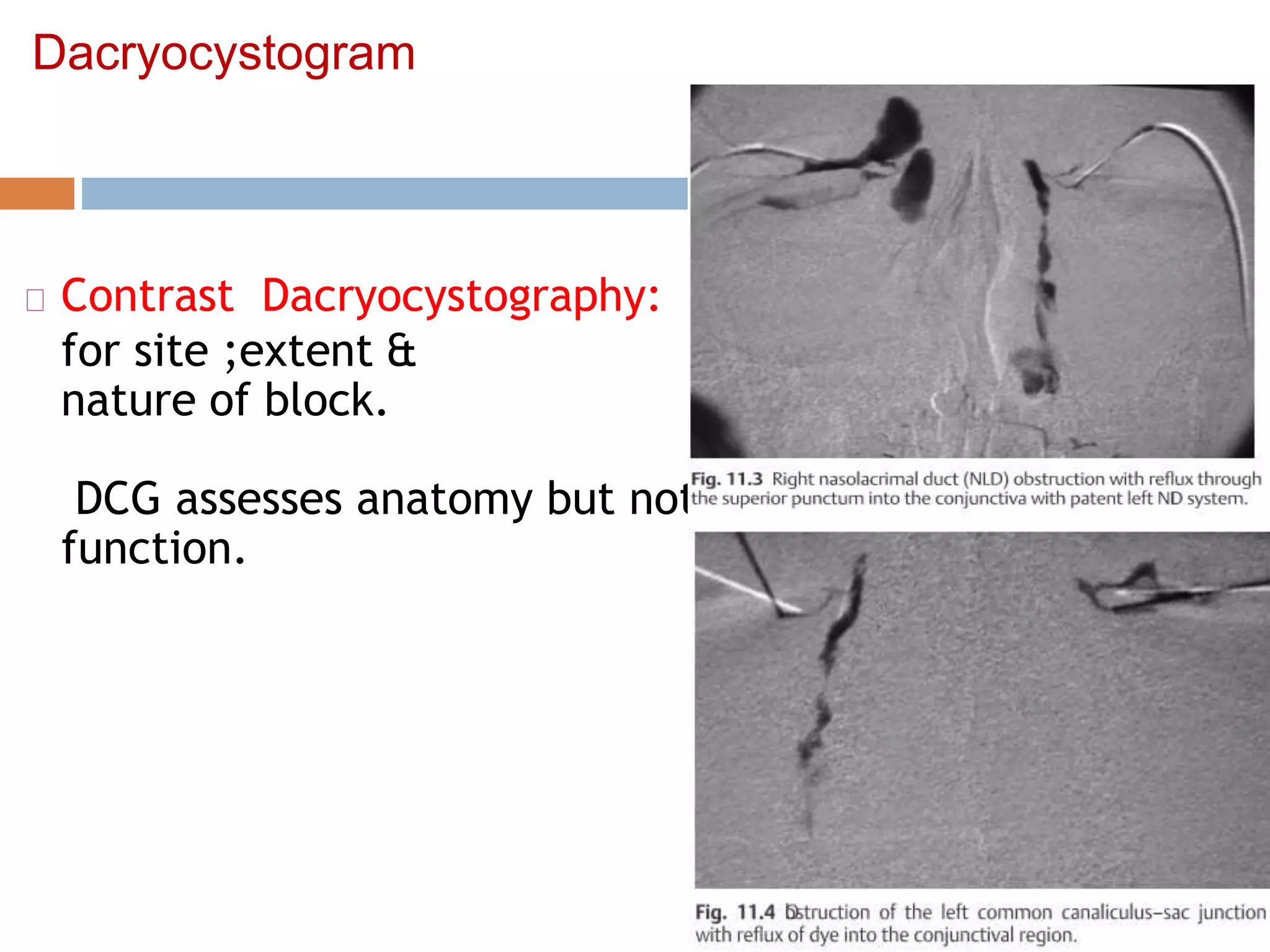
The document describes the anatomy and surgical procedure of endoscopic dacryocystorhinostomy (DCR). It details the anatomy of the lacrimal apparatus including the lacrimal gland, ducts, puncta, canaliculi, sac, and valves. It then explains the steps of an endoscopic DCR including identifying landmarks, raising mucosal flaps, removing lacrimal bone with punches or forceps, and opening the lacrimal sac to drain into the nose. Key anatomical structures like the lacrimal sac, frontal process, and uncinate process are highlighted to safely perform this surgery and relieve epiphora caused by nasolacrimal duct obstruction.