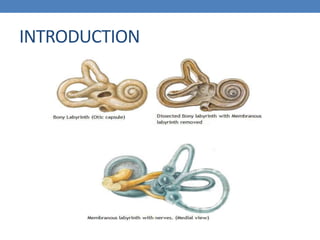
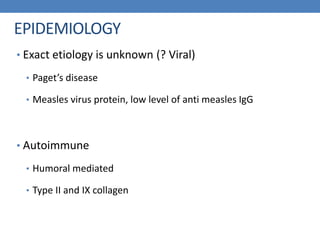
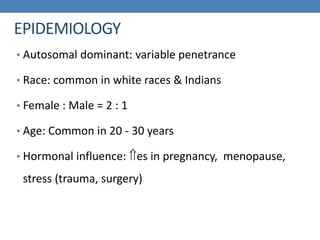
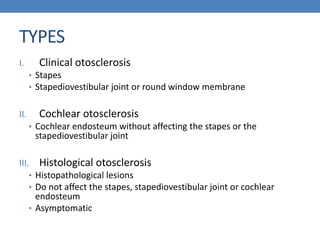
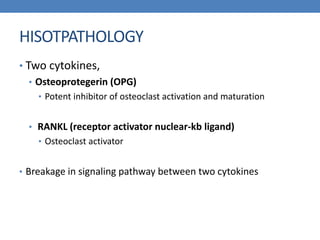
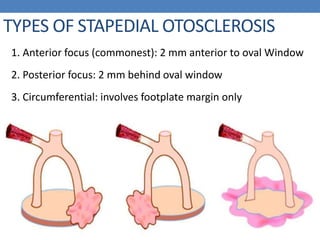
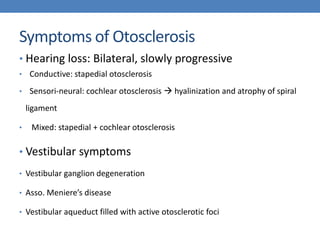
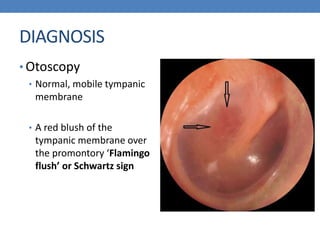
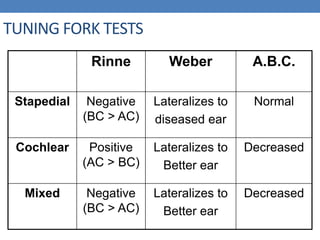
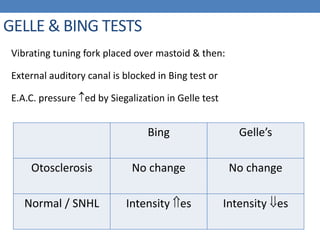
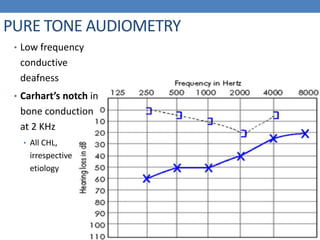
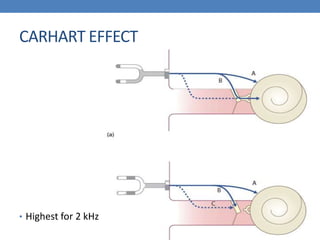
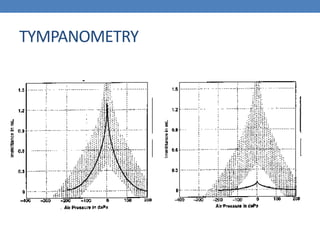
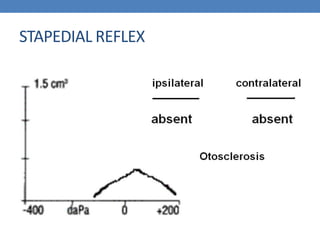
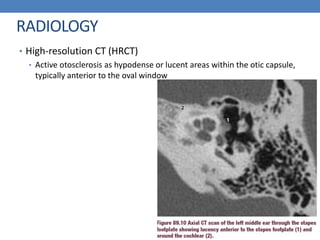
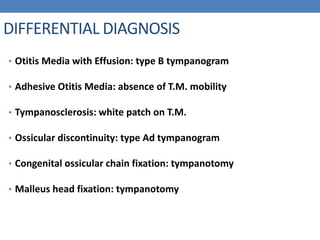
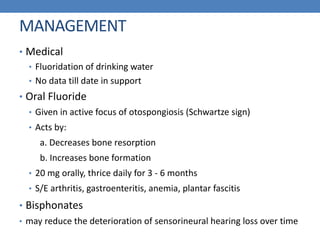
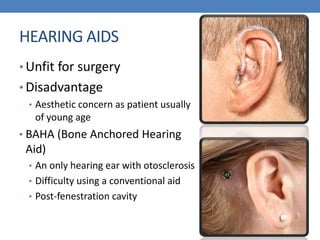
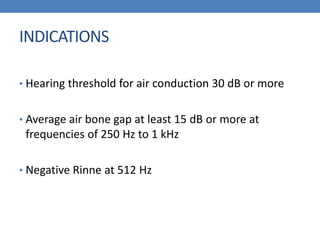
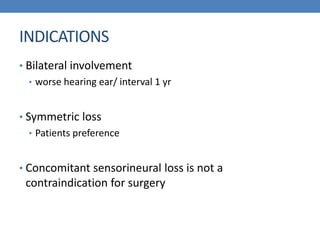
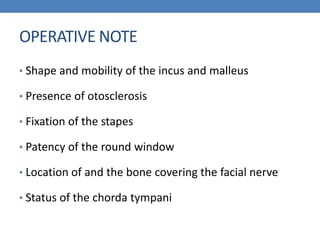
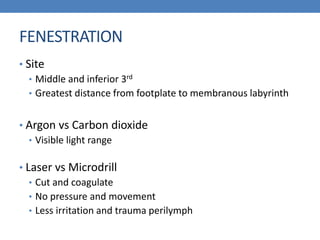
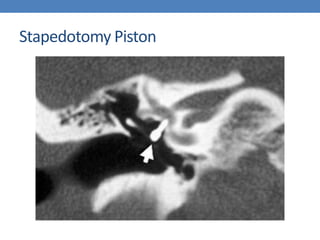
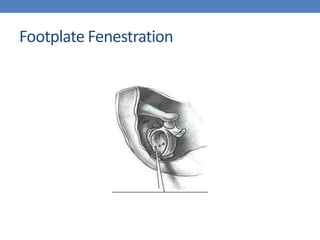
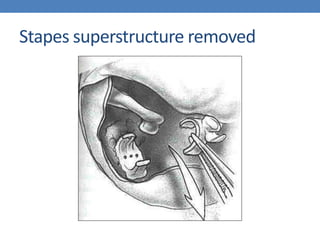
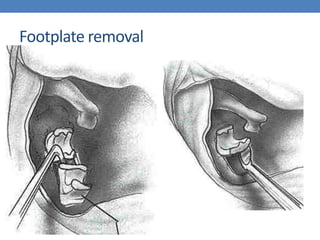
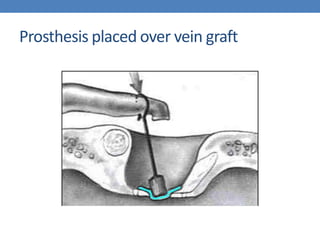
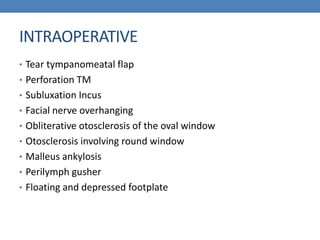
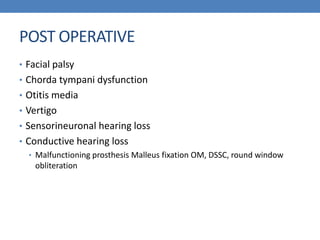
Otosclerosis is a hereditary disorder of bone metabolism in the otic capsule that causes fixation of the stapes footplate, resulting in conductive hearing loss. It involves abnormal bone resorption and deposition by osteoclasts and osteoblasts. Diagnosis is based on audiometry showing conductive hearing loss and Carhart's notch. Treatment options include hearing aids, stapedectomy to remove the fixed stapes footplate and replace it with a prosthesis, and cochlear implantation for advanced cases. Complications of stapedectomy include facial nerve injury, vertigo, and sensorineural hearing loss.